ADULT AND PEDIATRIC NEUROSURGERY, P
advertisement
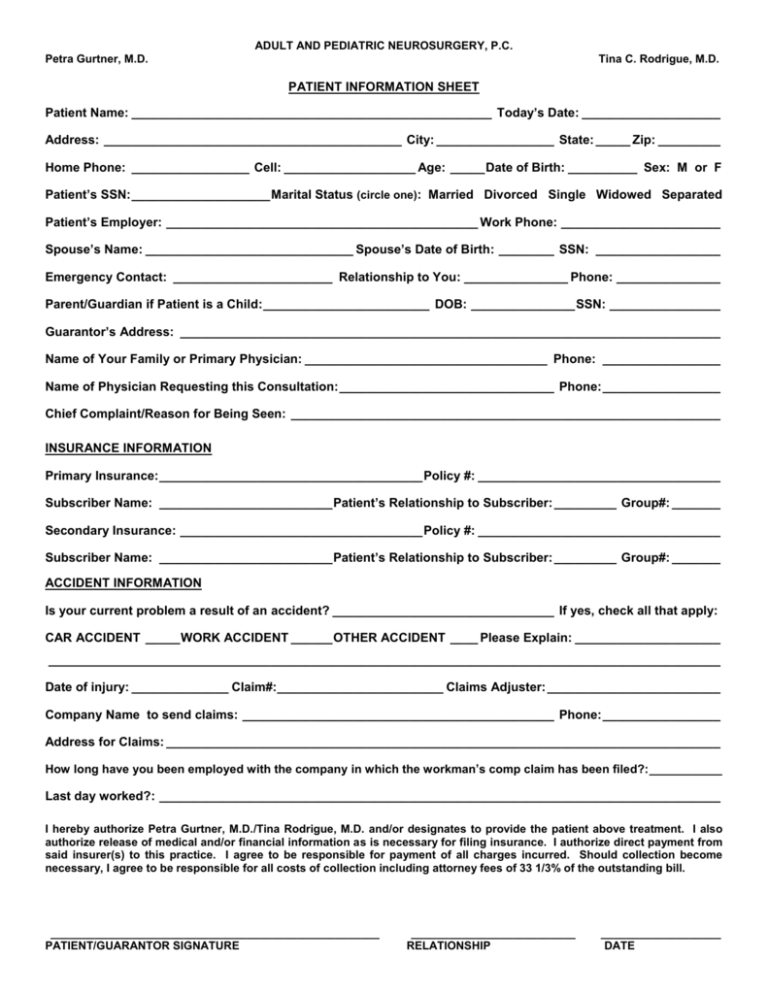
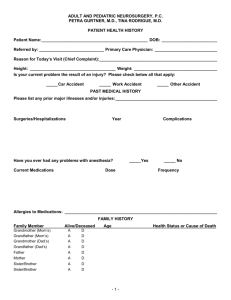
ADULT AND PEDIATRIC NEUROSURGERY, P.C. Petra Gurtner, M.D. Tina C. Rodrigue, M.D. PATIENT INFORMATION SHEET Patient Name: ____________________________________________________ Today’s Date: ____________________ Address: ___________________________________________ City: _________________ State: _____ Zip: _________ Home Phone: _________________ Cell: ___________________ Age: _____ Date of Birth: __________ Sex: M or F Patient’s SSN: ____________________ Marital Status (circle one): Married Divorced Single Widowed Separated Patient’s Employer: _____________________________________________ Work Phone: _______________________ Spouse’s Name: ______________________________ Spouse’s Date of Birth: ________ SSN: __________________ Emergency Contact: _______________________ Relationship to You: _______________ Phone: _______________ Parent/Guardian if Patient is a Child: ________________________ DOB: _______________ SSN: ________________ Guarantor’s Address: ______________________________________________________________________________ Name of Your Family or Primary Physician: ___________________________________ Phone: _________________ Name of Physician Requesting this Consultation: _______________________________ Phone: _________________ Chief Complaint/Reason for Being Seen: ______________________________________________________________ INSURANCE INFORMATION Primary Insurance: ______________________________________ Policy #: ___________________________________ Subscriber Name: _________________________ Patient’s Relationship to Subscriber: _________ Group#: _______ Secondary Insurance: ___________________________________ Policy #: ___________________________________ Subscriber Name: _________________________ Patient’s Relationship to Subscriber: _________ Group#: _______ ACCIDENT INFORMATION Is your current problem a result of an accident? ________________________________ If yes, check all that apply: CAR ACCIDENT _____ WORK ACCIDENT ______ OTHER ACCIDENT ____ Please Explain: _____________________ _________________________________________________________________________________________________ Date of injury: ______________ Claim#:________________________ Claims Adjuster: _________________________ Company Name to send claims: _____________________________________________ Phone: _________________ Address for Claims: ________________________________________________________________________________ How long have you been employed with the company in which the workman’s comp claim has been filed?: ___________ Last day worked?: _________________________________________________________________________________ I hereby authorize Petra Gurtner, M.D./Tina Rodrigue, M.D. and/or designates to provide the patient above treatment. I also authorize release of medical and/or financial information as is necessary for filing insurance. I authorize direct payment from said insurer(s) to this practice. I agree to be responsible for payment of all charges incurred. Should collection become necessary, I agree to be responsible for all costs of collection including attorney fees of 33 1/3% of the outstanding bill. ____________________________________________________ PATIENT/GUARANTOR SIGNATURE __________________________ RELATIONSHIP ___________________ DATE Adult and Pediatric Neurosurgery, P.C. Petra Gurtner, M.D. Tina C. Rodrigue, M.D. 248 W. Bute St., Suite 100, Norfolk, VA 23510 Phone: 757-622-1003 Fax: 757-622-1108 AUTHORIZATION TO RELEASE HEALTHCARE INFORMATION Patient’s Name: Date of Birth: Previous Name: Social Security #: I request and authorize release healthcare information of the patient named above to: to Name: Address: City: State: Zip Code: This request and authorization applies to: Healthcare information relating to the following treatment, condition, or dates: All healthcare information Other: Definition: Sexually Transmitted Disease (STD) as defined by law, RCW 70.24 et seq., includes herpes, herpes simplex, human papilloma virus, wart, genital wart, condyloma, Chlamydia, non-specific urethritis, syphilis, VDRL, chancroid, lymphogranuloma venereuem, HIV (Human Immunodeficiency Virus), AIDS (Acquired Immunodeficiency Syndrome), and gonorrhea. Yes No I authorize the release of my STD results, HIV/AIDS testing, whether negative or positive, to the person(s) listed above. I understand that the person(s) listed above will be notified that I must give specific written permission before disclosure of these test results to anyone. Yes No I authorize the release of any records regarding drug, alcohol, or mental health treatment to the person(s) listed above. Patient Signature: Date Signed: Adult and Pediatric Neurosurgery, P.C. Petra Gurtner, M.D. Tina C. Rodrigue, M.D. 248 W. Bute Street, Suite 100 Norfolk, Virginia 23510 Phone:757-622-1003 Fax: 757-622-1108 Disability, FMLA, Insurance and Medical Records Policy February 1, 2007 Disability Forms, Insurance Forms, and FMLA Forms: We will be happy to complete these forms for you. Please fill out all personal information on all forms before presenting them to the office. Allow at LEAST TWO WEEKS for completion of forms. The following pre-paid charges will apply: First Form, one page $20.00 First Form, multi page $35.00 Subsequent forms, one page (monthly, or recurring) $10.00 Subsequent forms, multi page (monthly, or recurring) $15.00 Medical Record Copies: We will be happy to provide copies of your medical records at your request. These records will be released to you or your authorized agent. A Medical Records Release Form is required before this information can be released. Please allow at LEAST TWO WEEKS for these records to be released. The following pre-paid charges will apply: Patient Requests $0.00 Base charge (chart retrieval, copying, postage, and labor) $10.00 Pages 1 – 50 $.50 per page Pages 51 and over $.25 per page I have read the above policy of Adult & Pediatric Neurosurgery, and understand that it applies to all forms, and medical records. Patient Signature: _______________________________________ Date: ___________________________ ADULT AND PEDIATRIC NEUROSURGERY, P.C. PETRA GURTNER, M.D., TINA RODRIGUE, M.D. PATIENT HEALTH HISTORY Patient Name: ______________________________________________ DOB: ________________________ Referred by: ____________________________ Primary Care Physician: ___________________________ Reason for Today’s Visit (Chief Complaint): ___________________________________________________ Height: _____________________________________ Weight: ____________________________________ Is your current problem the result of an injury? Please check below all that apply: _____ Car Accident _____ Work Accident _____ Other Accident PAST MEDICAL HISTORY Please list any prior major illnesses and/or injuries: ____________________________________________ Surgeries/Hospitalizations Year Have you ever had any problems with anesthesia? Current Medications Complications _____Yes Dose _____ No Frequency Allergies to Medications: __________________________________________________________________ FAMILY HISTORY Family Member Alive/Deceased Grandmother (Mom’s) Grandfather (Mom’s) Grandmother (Dad’s) Grandfather (Dad’s) A A A A D D D D Father A D Mother A D Sister/Brother A D Sister/Brother A D Age Health Status or Cause of Death -1- ADULT AND PEDIATRIC NEUROSURGERY, P.C. PETRA GURTNER, M.D., TINA RODRIGUE, M.D. PATIENT HEALTH HISTORY Patient Name: ______________________________________________ DOB: ________________________ SOCIAL HISTORY Occupation: _____________________________________________________________________________ Marital Status: ___ Single Do you have children: ___ Married ___ No Do you live alone?: ___ No ___ Yes ___ Yes ___ Separated ____ Divorced ___ Widowed How Many?: ____________________________________ Who lives with you?: _____________________________ Do you smoke cigarettes? _____ No, I have never smoked cigarettes. _____ No, I quit ____ years ago. At that time I was smoking __ pks per day for ____ years. _____ Yes, I smoke____ packs of cigarettes per day for ____ years. Do you smoke cigars or a pipe? __ No ___ Yes How often? _______ How many years? ________ Do you drink alcohol? ____ No, never (or rarely). ____ No, but I used to. Explain: _________________________________________________ ____ Yes. If yes, how often? ____ Daily ____ 1 or more times a week. _____ 1 or more times a month. Are you at risk for AIDS (e.g., sexual orientation, drug abuse, previous blood transfusion)? ____ No ___ Yes. Please Explain: ______________________________________________ REVIEW OF SYSTEMS Are you currently, or have you ever had problems with: (Circle Yes or No) CONSTITUTIONAL Fever ___________________________ Excessive Fatigue ________________ Yes/No Yes/No Weight Loss ____________________ Night Sweats ___________________ EYES Infections _______________________ Glaucoma _______________________ Wear Glasses ____________________ Yes/No Yes/No Yes/No Injuries ________________________ Yes/No Cataracts ______________________ Yes/No Date of Last Eye Exam _____________________ Yes/No Yes/No Yes/No Ear Pain _______________________ Yes/No Ringing in Ear (Right/Left) ________ Yes/No Nasal Drainage __________________ Yes/No Amount ________ Color________ Nasal Congestion _______________ Yes/No Sinus Problems _________________ Yes/No Sore Throat ____________________ Yes/No Date of Last Exam _________________________ EARS, NOSE, THROAT AND MOUTH Wear Hearing Aids ________________ Hearing Loss ____________________ Ear Infections ____________________ Balance Disturbances (e.g., Vertigo) Spinning __________________ Nose Bleeds _____________________ Inability to Smell _________________ Sinus Headaches _________________ Mouth Sores _____________________ Yes/No Yes/No Yes/No Yes/No Yes/No -2- Yes/No Yes/No ADULT AND PEDIATRIC NEUROSURGERY, P.C. PETRA GURTNER, M.D., TINA RODRIGUE, M.D. PATIENT HEALTH HISTORY Patient Name: ______________________________________________ DOB: ________________________ CARDIOVASCULAR High Blood Pressure ______________ Heart Murmur ____________________ Swelling in Feet or Hands __________ Chest Pain or Angina _____________ Yes/No Yes/No Yes/No Yes/No Irregular Pulse __________________ Yes/No High Cholesterol ________________ Yes/No Leg Pain While Walking __________ Yes/No Date of last EKG __________________________ RESPIRATORY Asthma _________________________ Yes/No Emphysema _____________________ Yes/No Bronchitis _______________________ Yes/No Lung Cancer _____________________ Yes/No Date of Last Chest X-ray ____________________ Chronic Cough __________________ Shortness of Breath _____________ Pneumonia _____________________ Bloody Sputum _________________ Yes/No Yes/No Yes/No Yes/No GASTROINTESTINAL Indigestion or Pain w/Eating________ Vomiting ________________________ Liver Disease ____________________ Abdominal Pain __________________ Ulcers or Gastritis ________________ Yes/No Yes/No Yes/No Yes/No Yes/No Nausea ________________________ Blood in Your Vomit _____________ Jaundice _______________________ Change in your Bowel Habits ______ Colon Cancer ___________________ Yes/No Yes/No Yes/No Yes/No Yes/No GENITOURINARY Urinary Tract Infections ___________ Blood in Your Urine _______________ Incontinence_____________________ Prostate Cancer (males) ___________ Uterine or Cervical Cancer (females) _ Yes/No Yes/No Yes/No Yes/No Yes/No Painful Urination ________________ Difficulty Starting or Stopping Stream Kidney Stones __________________ Endometriosis __________________ Yes/No Yes/No Yes/No Yes/No MUSCULOSKELETAL Arm or Leg Weakness _____________ Arm or Leg Pain __________________ Arthritis _________________________ Yes/No Yes/No Yes/No Back Pain ______________________ Yes/No Joint Pain or Swelling ____________ Yes/No Broken Bones __________________ Yes/No List: ___________________________________ INTEGUMENTARY Skin Disease_____________________ Nipple Discharge (females)_________ Yes/No Yes/No NEUROLOGICAL Fainting Spells or “Black Outs” _____ Problems with your Memory________ Difficulty with your Speech_________ Double or Blurred Vision __________ Coordination in Arm and/or Legs____ Yes/No Yes/No Yes/No Yes/No Yes/No Skin Cancer ____________________ Yes/No Breast Pain, Tenderness/Swelling (females) _________________ Yes/No Date and Results of Last Mammogram (females) _______________________________________________ Seizures _______________________ Disorientation __________________ Inability to Concentrate ___________ Face Weakness _________________ Yes/No Yes/No Yes/No Yes/No PSYCHIATRIC Anxiety _________________________ Yes/No Depression _____________________ Yes/No Other Psychiatric Disorder or Treatment _____________________________________________________ -3- ADULT AND PEDIATRIC NEUROSURGERY, P.C. PETRA GURTNER, M.D., TINA RODRIGUE, M.D. PATIENT HEALTH HISTORY Patient Name: ______________________________________________ DOB: ________________________ ENDOCRINE Diabetes ________________________ Increased Appetite________________ Excessive Thirst or Urination _______ Yes/No Yes/No Yes/No Thyroid Disease _________________ Hormone Problems ______________ Yes/No Yes/No HEMATOLOGIC/LYMPHATIC Anemia _________________________ Yes/No Bleeding Tendencies ______________ Yes/No Blood Transfusion ________________ Yes/No If yes, when? _____________________________ Hemophilia _____________________ Persistent Swollen Glands or Lymph Nodes ___________________ Yes/No ALLERGIC/IMMUNOLOGIC Food Allergies ___________________ Inhalant (Nasal) Allergies __________ Immunologic Disorders____________ List _____________________________________ List _____________________________________ Yes/No Yes/No Yes/No Yes/No THE ABOVE INFORMATION IS ACCURATE TO THE BEST OF MY KNOWLEDGE. ______________________________________________ PATIENT SIGNATURE ___________________________________ DATE ______________________________________________ PATIENT SIGNATURE ___________________________________ DATE ______________________________________________ PATIENT SIGNATURE ___________________________________ DATE I HAVE REVIEWED THE ABOVE INFORMATION WITH THE PATIENT. ______________________________________________ PHYSICIAN SIGNATURE ___________________________________ DATE ______________________________________________ PHYSICIAN SIGNATURE ___________________________________ DATE ______________________________________________ PHYSICIAN SIGNATURE ___________________________________ DATE -4-