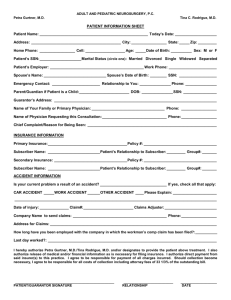
ADULT AND PEDIATRIC NEUROSURGERY, P
advertisement
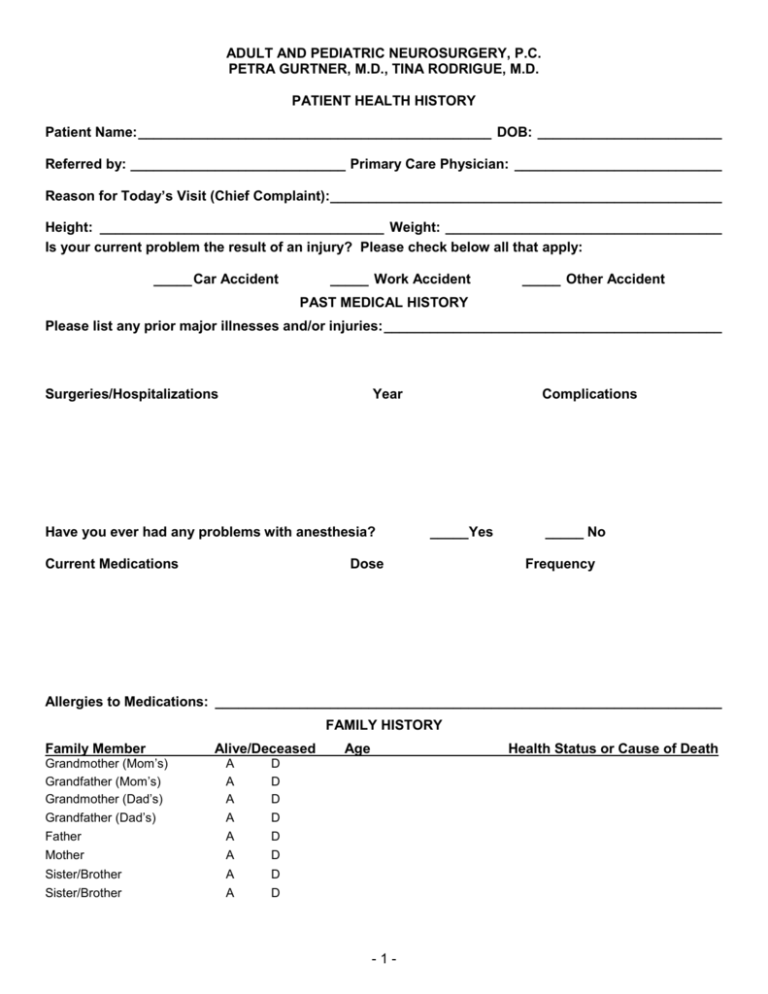
ADULT AND PEDIATRIC NEUROSURGERY, P.C. PETRA GURTNER, M.D., TINA RODRIGUE, M.D. PATIENT HEALTH HISTORY Patient Name: ______________________________________________ DOB: ________________________ Referred by: ____________________________ Primary Care Physician: ___________________________ Reason for Today’s Visit (Chief Complaint):___________________________________________________ Height: _____________________________________ Weight: ____________________________________ Is your current problem the result of an injury? Please check below all that apply: _____ Car Accident _____ Work Accident _____ Other Accident PAST MEDICAL HISTORY Please list any prior major illnesses and/or injuries: ____________________________________________ Surgeries/Hospitalizations Year Have you ever had any problems with anesthesia? Current Medications Complications _____Yes Dose _____ No Frequency Allergies to Medications: __________________________________________________________________ FAMILY HISTORY Family Member Alive/Deceased Grandmother (Mom’s) Grandfather (Mom’s) Grandmother (Dad’s) Grandfather (Dad’s) A A A A D D D D Father A D Mother A D Sister/Brother A D Sister/Brother A D Age Health Status or Cause of Death -1- ADULT AND PEDIATRIC NEUROSURGERY, P.C. PETRA GURTNER, M.D., TINA RODRIGUE, M.D. PATIENT HEALTH HISTORY Patient Name: ______________________________________________ DOB: ________________________ SOCIAL HISTORY Occupation: _____________________________________________________________________________ Marital Status: ___ Single Do you have children: ___ Married ___ No Do you live alone?: ___ No ___ Yes ___ Yes ___ Separated ____ Divorced ___ Widowed How Many?: ____________________________________ Who lives with you?: _____________________________ Do you smoke cigarettes? _____ No, I have never smoked cigarettes. _____ No, I quit ____ years ago. At that time I was smoking __ pks per day for ____ years. _____ Yes, I smoke____ packs of cigarettes per day for ____ years. Do you smoke cigars or a pipe? __ No ___ Yes How often? _______ How many years? ________ Do you drink alcohol? ____ No, never (or rarely). ____ No, but I used to. Explain: _________________________________________________ ____ Yes. If yes, how often? ____ Daily ____ 1 or more times a week. _____ 1 or more times a month. Are you at risk for AIDS (e.g., sexual orientation, drug abuse, previous blood transfusion)? ____ No ___ Yes. Please Explain: ______________________________________________ REVIEW OF SYSTEMS Are you currently, or have you ever had problems with: (Circle Yes or No) CONSTITUTIONAL Fever ___________________________ Excessive Fatigue ________________ Yes/No Yes/No Weight Loss ____________________ Night Sweats ___________________ EYES Infections _______________________ Glaucoma _______________________ Wear Glasses ____________________ Yes/No Yes/No Yes/No Injuries ________________________ Yes/No Cataracts ______________________ Yes/No Date of Last Eye Exam _____________________ Yes/No Yes/No Yes/No Ear Pain _______________________ Yes/No Ringing in Ear (Right/Left) ________ Yes/No Nasal Drainage __________________ Yes/No Amount ________ Color________ Nasal Congestion _______________ Yes/No Sinus Problems _________________ Yes/No Sore Throat ____________________ Yes/No Date of Last Exam _________________________ EARS, NOSE, THROAT AND MOUTH Wear Hearing Aids ________________ Hearing Loss ____________________ Ear Infections ____________________ Balance Disturbances (e.g., Vertigo) Spinning __________________ Nose Bleeds _____________________ Inability to Smell _________________ Sinus Headaches _________________ Mouth Sores _____________________ Yes/No Yes/No Yes/No Yes/No Yes/No -2- Yes/No Yes/No ADULT AND PEDIATRIC NEUROSURGERY, P.C. PETRA GURTNER, M.D., TINA RODRIGUE, M.D. PATIENT HEALTH HISTORY Patient Name: ______________________________________________ DOB: ________________________ CARDIOVASCULAR High Blood Pressure ______________ Heart Murmur ____________________ Swelling in Feet or Hands __________ Chest Pain or Angina _____________ Yes/No Yes/No Yes/No Yes/No Irregular Pulse __________________ Yes/No High Cholesterol ________________ Yes/No Leg Pain While Walking __________ Yes/No Date of last EKG __________________________ RESPIRATORY Asthma _________________________ Yes/No Emphysema _____________________ Yes/No Bronchitis _______________________ Yes/No Lung Cancer _____________________ Yes/No Date of Last Chest X-ray ____________________ Chronic Cough __________________ Shortness of Breath _____________ Pneumonia _____________________ Bloody Sputum _________________ Yes/No Yes/No Yes/No Yes/No GASTROINTESTINAL Indigestion or Pain w/Eating________ Vomiting ________________________ Liver Disease ____________________ Abdominal Pain __________________ Ulcers or Gastritis ________________ Yes/No Yes/No Yes/No Yes/No Yes/No Nausea ________________________ Blood in Your Vomit _____________ Jaundice _______________________ Change in your Bowel Habits ______ Colon Cancer ___________________ Yes/No Yes/No Yes/No Yes/No Yes/No GENITOURINARY Urinary Tract Infections ___________ Blood in Your Urine _______________ Incontinence_____________________ Prostate Cancer (males) ___________ Uterine or Cervical Cancer (females) _ Yes/No Yes/No Yes/No Yes/No Yes/No Painful Urination ________________ Difficulty Starting or Stopping Stream Kidney Stones __________________ Endometriosis __________________ Yes/No Yes/No Yes/No Yes/No MUSCULOSKELETAL Arm or Leg Weakness _____________ Arm or Leg Pain __________________ Arthritis _________________________ Yes/No Yes/No Yes/No Back Pain ______________________ Yes/No Joint Pain or Swelling ____________ Yes/No Broken Bones __________________ Yes/No List: ___________________________________ INTEGUMENTARY Skin Disease_____________________ Nipple Discharge (females)_________ Yes/No Yes/No NEUROLOGICAL Fainting Spells or “Black Outs” _____ Problems with your Memory________ Difficulty with your Speech_________ Double or Blurred Vision __________ Coordination in Arm and/or Legs____ Yes/No Yes/No Yes/No Yes/No Yes/No Skin Cancer ____________________ Yes/No Breast Pain, Tenderness/Swelling (females) _________________ Yes/No Date and Results of Last Mammogram (females) _______________________________________________ Seizures _______________________ Disorientation __________________ Inability to Concentrate ___________ Face Weakness _________________ Yes/No Yes/No Yes/No Yes/No PSYCHIATRIC Anxiety _________________________ Yes/No Depression _____________________ Yes/No Other Psychiatric Disorder or Treatment _____________________________________________________ -3- ADULT AND PEDIATRIC NEUROSURGERY, P.C. PETRA GURTNER, M.D., TINA RODRIGUE, M.D. PATIENT HEALTH HISTORY Patient Name: ______________________________________________ DOB: ________________________ ENDOCRINE Diabetes ________________________ Increased Appetite________________ Excessive Thirst or Urination _______ Yes/No Yes/No Yes/No Thyroid Disease _________________ Hormone Problems ______________ Yes/No Yes/No HEMATOLOGIC/LYMPHATIC Anemia _________________________ Yes/No Bleeding Tendencies ______________ Yes/No Blood Transfusion ________________ Yes/No If yes, when? _____________________________ Hemophilia _____________________ Persistent Swollen Glands or Lymph Nodes ___________________ Yes/No ALLERGIC/IMMUNOLOGIC Food Allergies ___________________ Inhalant (Nasal) Allergies __________ Immunologic Disorders____________ List _____________________________________ List _____________________________________ Yes/No Yes/No Yes/No Yes/No THE ABOVE INFORMATION IS ACCURATE TO THE BEST OF MY KNOWLEDGE. ______________________________________________ PATIENT SIGNATURE ___________________________________ DATE ______________________________________________ PATIENT SIGNATURE ___________________________________ DATE ______________________________________________ PATIENT SIGNATURE ___________________________________ DATE I HAVE REVIEWED THE ABOVE INFORMATION WITH THE PATIENT. ______________________________________________ PHYSICIAN SIGNATURE ___________________________________ DATE ______________________________________________ PHYSICIAN SIGNATURE ___________________________________ DATE ______________________________________________ PHYSICIAN SIGNATURE ___________________________________ DATE -4-