neonatology cme
advertisement

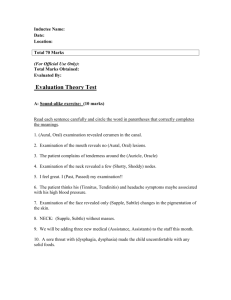
iDr Abhijit Mandal, MBBS(Cal), DNB(Family Medicine),SMO DNB Family Medicine : Tactical plan for clearing practical It’s an absolute high standard postgraduate examination.You have to study a lot but don’t go in deep.Understanding the basics is key to success.Knowledge in breadth is more required than in depth. Try to study all the topics as mentioned below. It’s one day examination from 0800hrs to 1630 hrs(time may vary from centre to centre) There five broad divisions in practicals 1.Medicine and allied 2.Surgery 3.Pediatrics 4.Community Medicine 5.Family Medicine Marks distribution as follows: A.Medicine and allied: Total 100 marks I. Long case: one total marks :45 marks II Short case: one total marks:30 marks III. Viva: a.Lab reports,x-rays,ECGs one question from each topic total 10 marks b.Drugs: one commonly used drug 05 marks c.Therapeutic and diagnostic procedure: 10 marks B.Surgery/Obs& Gynae /ENT/EYE/ORTHO: Total marks:25 I.Short case:one case C.Pediatrics: Total 75 marks I.Two Short cases: II.Viva: recent advances,neonatology,instruments,preventive pediatrics 25 marks 40 marks 35 marks D.Community Medicine: Total marks:50 a.National Health Policy: 10 marks b.Health programmes: 15 Marks c. Health indicators,health legislation,community health delivery services:10 marks d.Vital statistics, promotive & preventive medicine: 15 marks E.Family Medicine: Total marks:50 a.Morbidity pattern,Record keeping: b. Managementof cases in family set up: c.Emergencies: d. Medical Ethics,referrals,CME etc : 10 marks 15 marks 15 marks 10 marks Things to carry: Admit card,white coat,basic examination tools and above all self confidence GENERAL GUIDELINES FOR CASE PRESENTATION AND DISCUSSION: MEDICINE Cerebro-vascular disease History - Detailed history relating to the event onset, progress, neurological deficit(s); Assessment of risk factors for CVA; If young patient, to evaluate for ‘Stroke in young’; Medication/Treatment history Clinical examination - Vital Signs-pulse, BP, RR, Temp., Eval. Of carotids; Detailed Neurological exam including (Cranial N Palsies – Speech;Pupillary Signs;Motor System Examination); Exam of Heart/CNS; To evaluate for causes of stroke in young;Should be able to identify the Vascular Territory involved Fundus Exam. Investigations-All investigations but specifically-ECG;NCCT(Head);Role of CECT(Head);MRI(Brain);Carotid Doppler; Role of ECHO. Differential diagnosis-CVA ( Haemorrhagic,Thrombotic); In young patients (Aneurysm,AVM); Other Causes (Vasculitis;SOL; Causes of stroke in young) Management - Immediate M/M; Supportive Care; Specific — Role of Thrombolysis in Thrombotic Events/Infarcts— When , How; M/M of HT in setting of Stroke—How to bring down BP, Any other - Should discuss causes/Risk factors for CVA in elderly patients; Should discuss causes/Risk factors for stroke in young patients; Should be able to identify Vascular territory; Discussion on posterior circulation stroke should be there Multi-valvular heart disease History-Detailed history of symptoms– Palpitations, Dyspnoea, PND, Orthopnea, EDEMA, Hospitalizations, Embolisations; History suggestive of RHD, other connective tissue disease, IE; Should be able to identify-RT V/s LT sided Valve Lesions, Stenotic V/s Regurgitant Lesions Clinical examination- Detailed ESP, GPE-Pulse(especially for)- BP, Signs of IE, Evidence of RF, If suspected AR-Look for features of MARFAN’S, Syndrome,JVP, EDEMA; CVS – Detailed, thorough exam of CVS-all areas; Abdomen; Fundus Exam; CNS Investigations– ECG, Discuss Findings; CXR—Discuss Findings; ECHO—What all can be seen If IE – Blood c/s— How many/when; RF – ASLO/CRP, other anti strept Ab Differential diagnosis- To give diagnosis as Which all valves are involved list in order of severity; Etiology ( ? Rheumatic ? MARFANS etc. ); Presence/Absence of-Pulmonary A hypertension, Congestive cardiac failure, Arrythmias/Normal Sinus Rhythm, Rheumatic Aaivety, Infective Endo Carditis. Management - Discuss M/m in relation of; Valve involvement- Conservative, Surgical, Others of BMV; CHF; IE; RF; Emborisation; AF; Special Simulation eg. In Pregnancy discuss prognosis and outcome Any other – Discuss-Prophylaxis for RF; IE Prophylaxis; Anticoagulation; Digoxcin-Role and Toxicity; M/m of Embolisation in setting of IE; Fungal Endocarditis Cerebellar disease History- Detailed History of Onsent, Progression of complaints; Family History – should trace involvement in family for inherited forms of cerebellar disease; Drugs/Toxics – History especially of ; Other Neoplasms – Paraneoplastic involvement Clinical examination - Detailed neurological exam Especially of – CNS and also spine; Other systemsTo be able to identify cause of cerebellar involvement. Investigations - Role of MR/CT; Discuss findings Differential diagnosis-Acuteonset-Chroniconset;Symmetrical - Symmetrical;Asymmetrical – Asymmetrical.To discuss D/D according to individual situations. Management -To identify the involvement as; Degenerative; Inherited; Drug/Toxin related; Infective; Vascular involvement; Paraneoplastic; M/m of individual situation Any other -To discuss D/D appropriate IE clinical situation eg. Age. Congenital Heart Disease History - Onset of Symptoms – childhood, adolescence, adults; Discuss the symptoms; Cynosis – if yes cyanotic spells feeding; Growth and milestones in children; Respiratory infection Clinical examination-Any compiler eg. Stroke, etc.,Detailed Cardiovascular- Exam, GPE – Sxanosis, Cuilbbing, JVP, EDEMA; Evaluate for other inherited/congenital malformation/disorders. Investigations – ECG; CXR; ECHO; Polycythemia/Hci; ABG Differential diagnosis - To reach diagnosis as congenital HD. Cyanotic, Acynotic and then further discuss the individual differential thesis according to the case in hand; Eisenmenger – to discuss in detail. Management - ISSUEO regarding; M/m of cyanotic spells(in children); M/m of CHF; M/m relating to; Operability; Surgery; Prognosis and Outcome Short Case Myopathy - Disease of Muscle/Nerve History-History of symptoms,weakness especially, Onset, Progress, Prox V/s Distae, Severity, Fasciculations, Atrosphy, MSI Fatigue; To identify cause if possible on history; Paraneoplastic involvement Clinical examination - Complete physical exam including; Detailed neurological examination; Focus on demonstration of (focus on LMN signs); Refrences-Planter response, Atrophy of MSIS; Skin Exam; Spine Exam Investigations – Discuss + CPK– total = MSL Enzymes; LDH; NCN; EMG - if NM jn – Discuss tests for sis; MSI Biopsy Differential diagnosis - Should be able to give D/D of LMN involvement- N,MSI and how to differentiate, NMJ; D/D of individual disorders eg. If muscle involvement –Myopathy,MSI Dystrophy and then give elistology, Myositis Management-Depends upon clinical situation Fibro-cavitory lung disease History- Detailed history of Symptoms –Cough, dyspnoea/breathlessness, expectoration, fever, edema; Past history of TB; Family history of TB Clinical examination-GPE – Especially - Tracheal Position, cyanosis, clubbing, lymphadenopathy,Edema, Detailed respiratory examination Investigations- CXR; ECG; Role of CI Differential diagnosis - Discuss complications GENERAL GUIDELINES FOR CASE PRESENTATION AND DISCUSSION: Pediatric cases History-Correct sequence of chief complaints, present history, past history, family history, birth history,development history, socioeconomic history. All headings to be covered even if they are normal. However relative emphasis may be on relevant history e.g. dietary history in detail is important in malnutrition and development history in cerebral palsy, family history in genetic disorders and socioeconomic history in rheumatic fever etc. Emphasize on clarity of presentation and avoid unnecessary repetition. History of Present illness-Cover points in symptoms to find etiology of disease e.g. in failure to thrive, whether it is a chronic illness, malabsorption, nutritional deficiency etc. Progress of the disease eg static, improving or worsening. Secondary effects of the disease e.g. vit deficiencies in chronic liver disease.Treatment history should be covered in detail regarding nature of medicines e.g. tablets,injections, syrups etc and their effect on the illness. Patient may be able to tell actual name of medicine and it should not be disregarded. Just saying that patient has taken treatment from outside is not enough and analysis of treatment should be done. Course of the patient during hospital stay should be also asked. Past history -Relevant past history e.g. sore throat in Rheumatic fever etc and also generally of common chronic diseases egg TB etc should be covered .Any prolonged illness and hospitalization should be recorded. SE history-Per capita income. Education of parents, type of house and other relevant details . Dietary history-Must tell actual caloric intake .Calories of foods eaten once in 2-3 days may be equally divided over the week egg if a banana is eaten twice a week then calories may be of 2/7 banana a day and foods eaten very occasionally may be ignored from calculation of dietary intake. Premorbid as well as morbid caloric intake may be asked.Try to check if anthropometry corresponds to caloric intake as if caloric intake calculated is half of required but wt and ht are normal ,then recheck the calculation of caloric intake and try to explain the reason. Development history- Details of development should be asked as relevant to the case e.g. a case of Kalazaar in 12 yr old one may ask gross mile stones only but in dev delay in 1 yr old all mile stones in minute details may be asked. Examination-Detailed examination of vitals, anthropometry, general physical and systemic examination should be done. Canditate should present the involved system first. Various techniques of examination should be checked and demonstrated during the CME. Diagnosis and differential diagnosis-First most likely diagnosis should be told.Then diagnosis which can not be ruled out by clinical examination but require investigations for the same should be given.Then the similar conditions which have been clinically ruled out. Investigations-Should be relevant to the case. Ask interpretation of investigations. Discuss x ray, ECG , CT, ECHO findings etc. Treatment-Discuss specific treatment. Supportive treatment. Problems in treatment regarding side effects etc. Cost of treatment. Prognosis-Prognosis should be discussed. Counseling-Counseling in each case should be discussed. Routine care –Immunization; Family welfare; Psychological aspects.