file - BioMed Central
advertisement

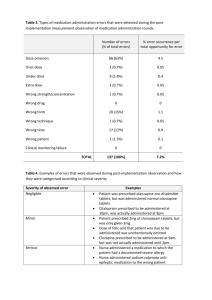
Study characteristics Study/Country Population Intervention Comparator(s) Outcomes (Primary, Secondary) Al-Ansari 2010 et al / Inclusion: Children under 18 months, diagnosed with acute 3% Hypertonic saline (HS) (5ml), 0.9% Normal saline (NS) (5ml) Bronchiolitis severity score improvement at 48 Qatar (Single centre) bronchiolitis, upper respiratory tract infection, wheezing 5% Hypertonic saline (HS) (5ml). administered every 4 hours until they hours, length of hospital stay, readmissions [67] and/or crackles on auscultation, BSS (> 4). Administered every 4 hours until were ready for discharge via a within 7 days and adverse events. Exclusion: <34 weeks gestation, history of wheezing, they were ready for discharge, via nebuliser (flow rate 10L/min). steroid use within 48 hours, obtundation and progressive a nebuliser (flow rate 10L/min). Administered with 1.5ml epinephrine. respiratory failure requiring ICU admission, apnea within 24 Administered with 1.5ml hours, oxygen saturation <85% in air, chronic lung disease, epinephrine. congenital heart disease, immunodeficiency. Espelt et al 2012 / Inclusion: Infants aged 1 to 24 months, 1st episode of 3% Hypertonic saline (HS) (3ml), 0.9% saline (NS) (3ml), administered Length of hospital stay and length of oxygen Argentina (number of bronchiolitis with clinical severity score of >5 and 02 administered 4 times per day over 4 times per day over 5 days via a use. centres unknown) saturation of <97%. 5 days via a nebuliser. nebuliser. Administered with 0.25 [25] Exclusion: Chronic respiratory or cardiovascular disease, Administered with 0.25 mg/kg mg/kg Albuterol. respiratory failure. Albuterol. Everard et al 2014 / Inclusion: Previously healthy infants under 1 year of age, 3% Hypertonic Saline (HS) (4ml), UK (Multi-centre) admitted with acute bronchiolitis, oxygen saturation <92% administered every 6 hours until discharge (length of hospital stay), admission [72] in air, consented and randomised within 4 hours of fit for discharge via PARI Sprint to intensive care units, readmission rates, admission by a medical paediatrician. nebuliser (flow rate 5L/minute). duration of respiratory symptoms within 28 Usual Care Time to fit for discharge, time to actual Exclusion: Wheezy bronchitis or asthma – children with an days of randomisation, healthcare utilisation apparent viral respiratory infection and wheeze with no or within 28 days of randomisation, Infant and occasional crepitations, reflux, previous lower respiratory parental quality of life using the Infant Toddler tract infections (requiring assessment in hospital), risk Quality of Life (ITQoL) questionnaire at 28 factors for severe disease [gestation <32 weeks, days following randomisation and adverse immunodeficiency, neurological and cardiac conditions, events. chronic lung disease], subjects where the carer’s English is not fluent and translational services are not available. Giudice et al 2012 / Inclusion: Children under 2 years, first episode of 3% Hypertonic saline (HS) 0.9% saline (NS), administered every Length of hospital stay and clinical response Italy (Single centre) bronchiolitis, 02 saturation of <94% in room air, significant administered every 6 hours via a 6 hours via a nebuliser (flow rate determined using clinical severity scores. [61] respiratory distress (Wang CSS score). nebuliser (flow rate 6L/min). 6L/min). Administered with Exclusion: Pre-existing cardiac/pulmonary disease, Administered with aerosolised aerosolised epinephrine (1.5mg). premature birth (<36 wks), previous asthma diagnosis, epinephrine (1.5mg). initial 02 stats less than 85% or respiratory distress requiring resuscitation. Kuzik et al 2007 / Inclusion: children under 18 months, first episode of 3% Hypertonic saline (HS) (4ml) 0.9% saline (NS) (4ml), administered Abu Dhabi and bronchiolitis. administered every 2 hours (3 every 2 hours (3 doses), every 4 hours Canada (Multi Exclusion: Previous history of wheezing, cardiopulmonary doses), every 4 hours (5 doses), (5 doses), every 6 hours till discharge centre) [20] disease or immunodeficiency, critical illness requiring every 6 hours till discharge via a via a nebuliser. admission to ITU, use of nebulised HS in last 12 hrs or nebuliser. Length of hospital stay and adverse events. premature birth (<34wks). Luo et al 2010 / China Inclusion: children under 2 years, first episode of viral 3% hypertonic saline (4ml), 3 0.9% saline (NS) (4ml), 3 Treatments Length of hospital stay, cough and wheezing, (Single centre) [62] bronchiolitis, mild to moderate bronchiolitis. Treatments every day every 8 every day every 8 hours until pulmonary moist crackles remission time and Exclusion: >24 months, previous wheezing episode, chronic hours until discharge via a discharge via a nebuliser. adverse events. cardiac or pulmonary disease, immunodeficiency, nebuliser. Administered with 2.5 Administered with 2.5 mg salbutamol. accompanying respiratory failure, requiring mechanical mg salbutamol. ventilation, having intervention 12 h before treatment, premature infants. Luo et al 2011 / Inclusion: infants aged <24 months, first episode of 3% hypertonic saline (HS) (4ml), 0.9% saline (NS) (4ml), administered Length of hospital stay, clinical severity scores China (Single centre) wheezing, admitted to hospital for treatment of moderate to administered every 2 hours (3 every 2 hours (3 doses), every 4 hours and remission of cough, wheezing, pulmonary [63] severe bronchiolitis. doses), every 4 hours (5 doses), (5 doses), every 6 hours till discharge moist crackles and adverse events. Exclusion: >24 months, previous episode of wheezing, every 6 hours till discharge via a via a nebuliser. chronic cardiac and pulmonary disease, immunodeficiency, nebuliser. accompanying respiratory failure needing mechanical ventilation, inhaled 3% HS 12 hours before treatment, premature birth. Maheshkumar et al Inclusion: Children under 2 years, 1st episode of 3% Hypertonic saline (HS) (3ml), Normal saline (NS) (3ml), Length of hospital stay, reduction in clinical 2013 / India (Single bronchiolitis, moderate distress. administered every 6 hours till fit administered every 6 hours till fit for severity scores, number of add on nebulisations centre) [66] Exclusion: pre-existing cardiac disease, previous wheezing for discharge, via a nebuliser (flow discharge via a nebuliser (flow rate 5- and number of treatment failures. episode, severe disease (score of >8) needing mechanical rate 5-6L/min). Administered with 6L/min). Administered with 0.15 ventilation, saturation <85% on room air, cyanosis, 0.15 mg/kg Salbutamol. mg/kg Salbutamol. obtunded consciousness and/or progressive respiratory failure. Mandelberg et al Inclusion: children up to 12 months, viral bronchiolitis with 3% hypertonic saline (HS) (4ml), 0.9% saline (NS) (4ml), administered Length of hospital stay, change in clinical 2003 / Israel (Single temperature of >38 degrees C leading to hospitalisation. administered 3 times a day every 8 3 times a day every 8 hours until severity scores and adverse events. centre) [18] Exclusion: cardiac or chronic respiratory disease, previous hours until ready for discharge via ready for discharge via an aeromist wheezing episode, saturation <85% in room air, obtunded an aeromist nebuliser (flow rate nebuliser (flow rate 5L/min). consciousness, progressive respiratory failure needing 5L/min).Administered with 1.5 mg Administered with 1.5 mg mechanical ventilation. epinephrine. Administered until epinephrine. The nebuliser was nebuliser empty. administered until empty. Nemsadze et al 2013 Children 2 months to 2 years old with bronchiolitis, 3% Hypertonic saline (HS), Normal saline (NS) administered Bronchiolitis Clinical Score, length of hospital / Georgia (Number of eligibility criteria unclear as abstract only. administered every 6 hours. every 6 hours. stay and change in oxygen saturation. centres unknown) [68] Ojha et al 2014 / Inclusion: Aged 6 weeks – 24 months, presenting with 3% Hypertonic Saline (HS) (4ml), 0.9% Normal Saline (NS) (4ml), Length of hospital stay and requirement of Nepal (Single centre) bronchiolitis for the first time. patients in each group received patients in each group received oxygen supplementation. [71] Exclusion: Previous episode of wheezing, chronic cardiac minimum of three nebulization minimum of three nebulisation each and pulmonary disease, immunodeficiency, respiratory each day delivered at 8 hour day delivered at 8 hour intervals until failure, mechanical ventilation, inhaling nebulised 3% saline intervals until discharge via a discharge via a nebuliser. and salbultamol 12 hours before treatment, premature nebuliser. infants (less than 34 weeks), oxygen saturation below 85% on room air. Ozdogan et al 2014 / Inclusion: Infants 1-24 months of age admitted to hospital 3% Hypertonic Saline (HS), 5% 0.9% normal saline (NS) administered Change in respiratory score and length of Turkey (Number of with acute bronchiolitis. Hypertonic Saline (HS). via nebulisations given three times a hospital stay. centres unknown) Exclusion: unclear – abstract only. Nebulisations given three times a day, each dose was administered with day via a nebuliser, albuterol was Albuterol. [27] given with each dose. Pandit et al 2013 / Inclusion: 2 to 12 months and admitted with acute 3% Hypertonic saline (HS) (4ml). 0.9% saline (NS) (4ml). The Length of hospital stay, improvement in India (Single centre) bronchiolitis. The nebulisation was given three nebulisation was given three times Respiratory Distress Assessment Instrument [65] Exclusion: Previous wheezing and respiratory distress, times with an interval of one hour, with an interval of one hour, there score, haemoglobin saturation, respiratory rate, family history of asthma, atopy, congenital heart disease, there after nebulisation was given after nebulisation was given every 6 heart rate, number of add on treatments and ventilation as new-born, patients with shock, seizures, heart every 6 hours until discharge via a hours until discharge via a nebuliser. adverse events. rate (>180/min), respiratory rate (>100/min) and in nebuliser (flow rate 6-8 L/minute). Administered with 1ml/1mg respiratory failure, consolidation lung on X-ray. Administered with 1ml/1mg Adrenaline. Adrenaline. Sharma et al 2013/ Inclusion: Children from 1- 24 months,1st episode of acute 3% Hypertonic saline (HS) (4ml), 0.9% saline (NS) (4ml), administered Length of hospital stay, clinical severity scores India (Number of bronchiolitis, hospitalised, clinical severity score 3-6. administered every 4 hours, 6 every 4 hours, 6 times a day till ready and adverse events. centres Exclusions: obtunded consciousness, cardiac disease, times a day till ready for discharge for discharge via a nebuliser (flow unknown)[64] chronic respiratory disease, previous wheezing episode, via a nebuliser (flow rate 7 rate 7 L/minute). Administered with progressive respiratory distress needing respiratory support L/minute). Administered with 2.5 2.5 mg salbutamol. The nebuliser was other than oxygen. mg salbutamol. Nebuliser was administered until empty. administered until empty. Silver et al 2014 / Inclusion: Patients up to 12 months of age, admitted to 3% Hypertonic Saline (HS) (4ml), 0.9% normal saline (NS) (4ml), Length of hospital stay, readmission for New York (Number hospital with bronchiolitis. administered every 4 hours until administered every 4 hours until bronchiolitis within 30 days of discharge and of centres unknown) Exclusion: Status asthmaticus, chronic cardiopulmonary discharge. Administered using a discharge via a nebulizer with 5 litres adverse events. [70] disease, Trisomy 21and immunodeficiency or transplant standard pressurised hospital wall oxygen flow. Administered until recipient or neuromuscular disease. Admission directly to nebuliser flow rate 5L/min and nebuliser treatment complete. ICU, previous use of nebulized hypertonic saline less than administered until nebuliser 12 hours prior to presentation and previous enrolment in the treatment complete. study in 72 hours prior to presentation. Sosa-Bustamante et Inclusion: Aged 2-24 months, first episode of wheezing 3% Hypertonic Saline (HS) (4ml), 0.9% Hypertonic Saline (NS) (4ml), Score respiratory distress, hours of hospital al 2014 / Mexico associated with respiratory distress, history of upper nebulized for 3 initial sessions administered via nebulisations for 3 stay, hospital readmission and frequency of (Single centre) [26] respiratory tract infections and evaluation of respiratory lasting 20 minutes each and every initial sessions lasting 20 minutes complications of the disease itself. difficulty with Scale Hospital Sant Joan de Deu from 6 – 16 4 hours during hospital stay, 100 each and every 4 hours during at entry points. micrograms / kg salbutamol was hospital stay. Administered with 100 Exclusion: Subjects with history of previous wheezing, given with each dose. micrograms / kg salbutamol. asthma, or who have received bronchodilator treatment before the present illness. Patients with chronic lung disease, heart disease, with congenital or acquired anatomic abnormalities of the airway. Tal et al 2006 / Israel Inclusion: children under 12 months, clinical presentation of 3% Hypertonic saline (HS) (4ml), 0.9% Saline (NS) (4ml), 3 treatments Length of hospital stay, change in clinical (Number of centres viral bronchiolitis that led to hospitalization. 3 treatments each day each day administered every 8 hours severity scores and adverse events. unknown) [19] Exclusion: Cardiac disease, chronic respiratory disease, administered every 8 hours via a via a nebuliser (output 0.25 ml/min). previous wheezing episode, age >12 months, 02 sats <85%, nebuliser (output 0.25 ml/min). Administered with 1.5mg epinephrine. obtunded consciousness and/or progressive respiratory Administered with 1.5mg The nebuliser was administered until failure needing ventilation. epinephrine. Nebuliser empty. administered until empty. Teunissen et al 2014 / Inclusion: Children aged 0-24 months, admitted to hospital 3% Hypertonic saline (HS) (4ml), 0.9% saline (NS) (4ml), administered Length of hospital stay, clinical severity scores, The Netherlands with viral bronchiolitis with a Wang score of >3. 6% Hypertonic saline (HS) (4ml). every 8 hours until discharge via a transfer to Paediatric Intensive Care Units, (Multi-centre) [69] Exclusion: Excluded if Wang score improved by at least 2 Administered every 8 hours until HOT Top Plus Nebuliser (flow rate 6- need/duration of tube feeding or supplemental points after inhalation, congenital heart disease, chronic pre- discharge via a HOT Top Plus 8 L/minute). Administered with 2.5 oxygen and adverse events. existent lung disease, T-cell immunodeficiency, Nebuliser (flow rate 6-8 mg salbutamol. The nebuliser was corticosteroid treatment and previous wheezing, eczema or L/minute). Administered with administered until empty. food allergy. 2.5mg salbutamol. Nebuliser administered until empty.