Cigdem_Benlice_Abstract_(IPAA)
advertisement
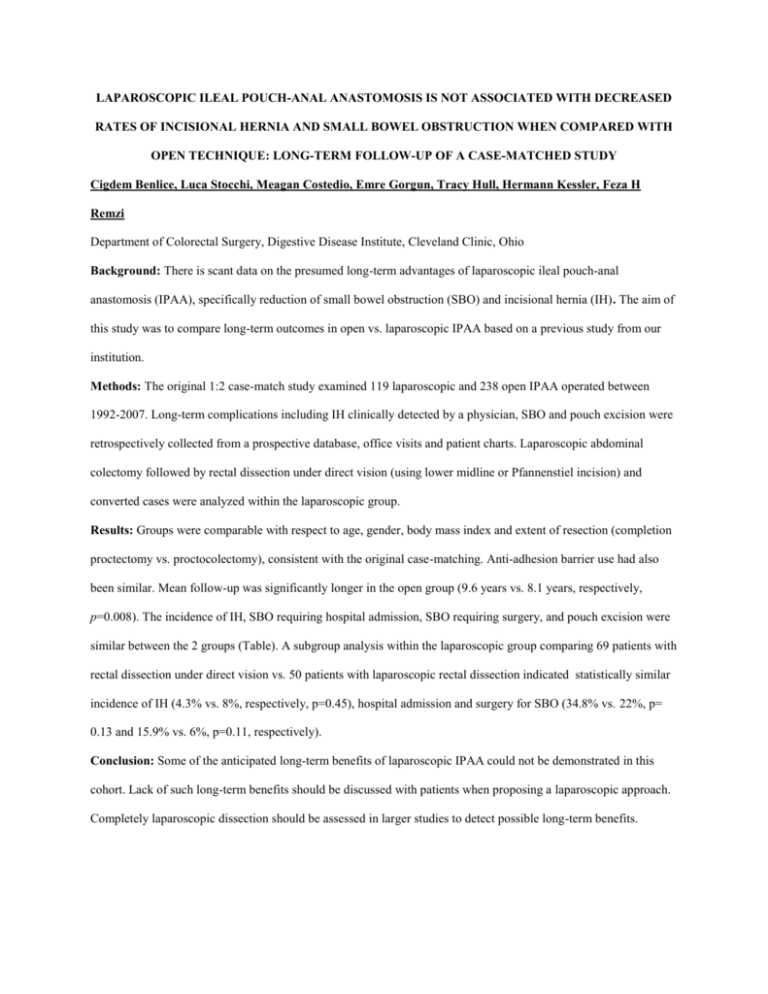
LAPAROSCOPIC ILEAL POUCH-ANAL ANASTOMOSIS IS NOT ASSOCIATED WITH DECREASED RATES OF INCISIONAL HERNIA AND SMALL BOWEL OBSTRUCTION WHEN COMPARED WITH OPEN TECHNIQUE: LONG-TERM FOLLOW-UP OF A CASE-MATCHED STUDY Cigdem Benlice, Luca Stocchi, Meagan Costedio, Emre Gorgun, Tracy Hull, Hermann Kessler, Feza H Remzi Department of Colorectal Surgery, Digestive Disease Institute, Cleveland Clinic, Ohio Background: There is scant data on the presumed long-term advantages of laparoscopic ileal pouch-anal anastomosis (IPAA), specifically reduction of small bowel obstruction (SBO) and incisional hernia (IH). The aim of this study was to compare long-term outcomes in open vs. laparoscopic IPAA based on a previous study from our institution. Methods: The original 1:2 case-match study examined 119 laparoscopic and 238 open IPAA operated between 1992-2007. Long-term complications including IH clinically detected by a physician, SBO and pouch excision were retrospectively collected from a prospective database, office visits and patient charts. Laparoscopic abdominal colectomy followed by rectal dissection under direct vision (using lower midline or Pfannenstiel incision) and converted cases were analyzed within the laparoscopic group. Results: Groups were comparable with respect to age, gender, body mass index and extent of resection (completion proctectomy vs. proctocolectomy), consistent with the original case-matching. Anti-adhesion barrier use had also been similar. Mean follow-up was significantly longer in the open group (9.6 years vs. 8.1 years, respectively, p=0.008). The incidence of IH, SBO requiring hospital admission, SBO requiring surgery, and pouch excision were similar between the 2 groups (Table). A subgroup analysis within the laparoscopic group comparing 69 patients with rectal dissection under direct vision vs. 50 patients with laparoscopic rectal dissection indicated statistically similar incidence of IH (4.3% vs. 8%, respectively, p=0.45), hospital admission and surgery for SBO (34.8% vs. 22%, p= 0.13 and 15.9% vs. 6%, p=0.11, respectively). Conclusion: Some of the anticipated long-term benefits of laparoscopic IPAA could not be demonstrated in this cohort. Lack of such long-term benefits should be discussed with patients when proposing a laparoscopic approach. Completely laparoscopic dissection should be assessed in larger studies to detect possible long-term benefits. Table. Comparison of demographics and long-term results between laparoscopic and open IPAA. Conversion BMI, kg/m2 Anti-adhesion barrier use Follow-up, months Incisional hernia Midline Ileostomy site Umbilical port site Right lower quadrant port site Pfannenstiel extraction site Hospital admission for SBO Surgery for SBO Pouch excision Values are reported as mean (SD) or absolute values (%). Open (N=238) N/A 24.9 (4.5) 43 (18.1%) 116 (64) 20 (8.4%) 12 8 N/A N/A N/A 62 (26.1%) Laparoscopic (N=119) 9 (7.6%) 24.7 (5.1) 23 (19.3%) 98 (50) 7 (5.9%) 1 3 2 1 0 35 (29.4%) P value 20 (8.4%) 12 (5%) 14 (11.8%) 7 (5.9%) 0.31 0.74 0.66 0.77 0.008 0.4 0.5