UoB-CLN-AES-SOP-001 Adverse Event Reporting v 1 0
advertisement

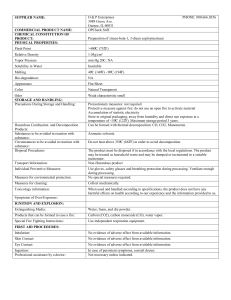
Adverse Event reporting UoB QMS reference number: UoB-CLN-AES-SOP-001 Purpose: This Standard Operating Procedure (SOP) describes the processes involved in Adverse Event reporting from trial set up to trial closure. Scope: The SOP must be adhered to in all clinical trials where the University of Birmingham (UoB) takes on the Sponsor responsibility for pharmacovigilance. This SOP may be used as a guidance document in all other cases. Implementation plan: This SOP will be implemented directly after the implementation date for any trials that have not been set up. For any trials that have already been set up, the reporting requirements to the Research Ethics Committee (REC), Competent Authority (CA) and the UoB Research Governance Team (RGT) will be implemented directly after the implementation date. All other processes should be adhered to as far as possible. Date of implementation: 16-Dec-2013 Property of the University of Birmingham, Vincent Drive, Edgbaston, Birmingham, B15 2TT, United Kingdom. Not to be printed, copied or distributed without authorisation Copies are only valid for 14 days and may be subject to amendment at any time. Refer to the electronic document management system for the latest version. Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 1 of 10 Adverse Event Reporting Abbreviations and Definitions: Term Description Adverse Event Any untoward medical occurrence in a patient or clinical trial subject administered a medicinal product and which does not necessarily have a causal relationship with this treatment. Comment: An Adverse Event can therefore be any unfavourable and unintended sign (including abnormal laboratory findings), symptom or disease temporally associated with the use of a medicinal product, whether or not related to the medicinal product. Adverse Reaction For CTIMPs, all untoward and unintended responses to an investigational medicinal product related to any dose administered. AE See ‘Adverse Event’. AR See ‘Adverse Reaction’ Reference Safety Information Term used within EC Detailed Guidance (CT3) June 2011, meaning the applicable product information which is used to determine the expectedness of an Adverse Reaction. This information is normally obtained from within the Summary of Product Characteristics or Investigator Brochure; when referring to the Investigator Brochure the relevant section must be defined. It may be a separate document in its own right. It must be defined at the start of a trial. RSI See ‘Reference Safety Information’ SAE See ‘Serious Adverse Event’. SAR See ‘Serious Adverse Reaction’ Serious Adverse Event Any untoward medical occurrence or effect that at any dose: Results in death Is life-threatening* Requires hospitalisation or prolongation of existing inpatients’ hospitalisation Results in persistent or significant disability or incapacity Is a congenital anomaly/birth defect Or is otherwise considered medically significant by the Investigator** Comments: The term severe is often used to describe the intensity (severity) of a specific event. This is not the same as serious, which is based on participants/event outcome or action criteria. * Life threatening in the definition of an SAE refers to an event in which the participant was at risk of death at the time of the event; it does not refer to an event that hypothetically might have caused death if it were more severe. ** Medical judgment should be exercised in deciding whether an AE is serious in other situations. Important AEs that are not immediately life threatening or do not result in death or hospitalisation but may jeopardise the subject or may require intervention to prevent one of the other outcomes listed in the definition above, should be considered serious. Serious Adverse Reaction For CTIMPs, an adverse reaction which also meets the definition of a Serious Adverse Event. Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 2 of 10 Adverse Event Reporting SUSAR See ‘Suspected Unexpected Serious Adverse Reaction’ Suspected Unexpected Serious Adverse Reaction For CTIMPs, A Serious Adverse Reaction that is unexpected i.e. the nature, or severity of the event is not consistent with the applicable product information. A SUSAR should meet the definition of an Adverse Reaction, an Unexpected Adverse Reaction and a Serious Adverse Reaction UAR See ‘Unexpected Adverse Reaction’ Unexpected Adverse Reaction For CTIMPs, an Adverse Reaction, the nature or severity of which is not consistent with the applicable product information (e.g. investigator's brochure for an unauthorised investigational product or summary of product characteristics for an authorised product). Unexpected and Related Event For non-CTIMPs, an event which meets the definition of both an Unexpected Event and a Related Event. Unexpected Event For non-CTIMPs, the type of event that is not listed in the protocol as an expected occurrence. Background: The process of Adverse Event reporting is key to any clinical trial, be it a Medical Devices trial, a Clinical Trial using an Investigational Medicinal Product (CTIMP) or any other trial. The needs for and responsibilities relating to Adverse Event reporting are described in the NHS Research Governance Framework; see link: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/139565/dh_4122427.pd f. This SOP covers adverse event reporting for all trials, detailing specifics for specific groups of trials where applicable. For Clinical Trials using Investigational Medicinal Products (CTIMPs), The Medicines for Human Use (Clinical Trials) Regulations 2004 and amendments detail the pharmacovigilance reporting requirements of the Sponsor or the Sponsor’s delegate. Part 5 of this act lists the legal responsibilities of Investigators and the Sponsor with regard to pharmacovigilance reporting. Additional guidance has been published by the EU 2011/C 172/01: ‘CT-3’, June 2011: Detailed guidance on the collection, verification and presentation of adverse event/reaction reports arising from clinical trials on medicinal products for human use’ (subsequently referred to as the detailed guidance: http://ec.europa.eu/health/files/eudralex/vol-10/21_susar_rev2_2006_04_11_en.pdf ). Advanced Therapies Medicinal Products are further regulated via the ‘Regulation (EC) No 1394/2007 of the European Parliament and of the council of 13 November 2007 on advanced therapy medicinal products and amending Directive 2001/83/EC and Regulation (EC) No 726/2004’; this regulation and further guidance can be found on the MHRA website, link: http://www.mhra.gov.uk/Howweregulate/Advancedtherapymedicinalproducts/Aboutadvancedt herapymedicinalproducts/index.htm . Each competent authority within the EU also publishes its own set of guidelines. The MHRA provides additional guidance and requirements for safety reporting within clinical trials in the UK. This detail is available on their website: the current link ishttp://www.mhra.gov.uk/Howweregulate/Medicines/Licensingofmedicines/Clinicaltrials/Safet yreporting-SUSARSandASRs/index.htm Feedback from MHRA Good Clinical Practice inspections may also be taken as guidance (See MHRA (2012) Good Clinical Practice Guide, UK: The Stationery Office). The MRC/DH/MHRA have also published a paper called “Joint Project Risk-adapted Approaches to the Management of Clinical Trials of Investigational Medicinal Products” (http://www.mhra.gov.uk/home/groups/l-ctu/documents/websiteresources/con111784.pdf) which defines a simple risk categorisation for clinical trials based on the marketing information Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 3 of 10 Adverse Event Reporting of the IMP and standard of care. This document specifies that a risk based strategy can be applied to safety monitoring of clinical trials. The International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) Guidelines have also been issued to describe the scope and content of a Development Safety Update Report (DSUR) which replaces the requirement to submit an Annual Safety Report in the EU as of the 1st September 2011. See link: http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E2F/Present ation/ICH_E2F_step_4_October_2010.pdf. For medical devices there are a number of directives and guidelines – details can be found on: http://www.mhra.gov.uk/Howweregulate/Devices/ and http://ec.europa.eu/health/medicaldevices/files/meddev/2_7_3_en.pdf All links are correct at the time of writing. Responsibilities: Sponsor (for UoB via the Research Governance Team): Ensure safety information is reported annually to the relevant CA(s) and REC(s) Upon request provide contact details of any trials using the same IMPs sponsored by the same Sponsor. When informed of any potential significant safety issues that may have to be reported to the Chief Investigators (CIs) of any other trials in the Sponsor’s portfolio using the same IMP, ensure further reporting is undertaken Sponsor duties delegated to Chief Investigator or delegate: Where the UoB takes on the Sponsor responsibility for pharmacovigilance, the UoB will delegate the majority of pharmacovigilance duties to the CI, who may delegate these duties further to their trials team. These include the following: Decide on the level of Adverse Event reporting and ensure this is documented in the protocol Decide on the applicable product information; for CTIMPS the Reference Safety Information (RSI) Continuously weigh anticipated benefits and risks of the clinical trial which includes ongoing safety evaluation of IMPs Where producing an Investigator Brochure (IB) for a trial, ensure that the IB is validated at least once a year Where using an existing IB or Summary of Product Characteristics (SmPC), ensure its contents is reviewed on a regular basis; e.g. once a year Set up systems for Adverse Event reporting according to the applicable regulations and/or guidance Ensure site staff are appropriately trained on the trial specific Adverse Event reporting requirements including the need for the PI or their delegate to perform the causality assessment and ensure training is documented Keep detailed records of all adverse events relating to a clinical trial reported to the Sponsor by the investigators of that trial Review causality assessments and perform expectedness assessments Categorise SAEs Notification of: For CTIMPs: Suspected Unexpected Serious Adverse Reactions (SUSARs) to CA(s) and REC within the required timelines. For Medical Devices: SAEs to CA/REC Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 4 of 10 Adverse Event Reporting For other trials: Unexpected and Related Serious Adverse Events (SAEs) to the REC within the required timelines. Where conducting a trial in a site based in a third country (i.e. a non-EU member state), ensure the local regulations are adhered to and ensure all SUSARs occurring at that site are entered in the European database Inform Principal Investigators of any safety issues in a timely fashion; for CTIMPs this includes forwarding information about SUSARs For CTIMPs: generate a DSUR annually and send to the CA(s) and REC For non-CTIMPs generate Annual Progress Report and submit to REC Site Principal Investigator or delegate As per the trial specific procedures and any local procedures Ensure the Sponsor is immediately informed of any Serious Adverse Events (SAEs) (except for those identified in the protocol as not requiring immediate reporting) Perform causality assessments When requested, provide any further information Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 5 of 10 Adverse Event Reporting Procedure: During trial set up: o Decide on the level of Adverse Event reporting o Decide on the applicable product information; for CTIMPS the RSI o Include a section in the protocol regarding adverse event reporting requirements; see section 9 of UoB-CLN-ESDo o o o o o o o o o o o o o o o QCD-001 Protocol template Develop a SAE form: · For Medical Devices, consider using the MEDDEV SAE template form; see references below · See for an optional template UoB-CLN-AES-QCD-002: SAE Form template · Develop an internal process for SAE handling; see for an example UoB-CLN-AES-QCD-003: Internal process for SAE handling example. Ensure any Sponsor specific requirements are embedded in the process. Note this process may be embedded in local SOPs Ensure site staff are appropriately trained on the trial specific Adverse Event reporting requirements, including the need for the PI or their delegate to perform the causality assessment and that training is documented Remind sites of possible need of reporting any SAEs to their R&D departments as per their local practices Consider developing pregnancy notification form Consider setting up as SAE tracking log Consider registering the trial at the eSUSAR website; see references below During trial – monitor Adverse Event reporting Continuously weigh anticipated benefits and risks of the clinical trial which includes ongoing safety evaluation of IMPs Keep detailed records of all adverse event relating to a clinical trial reported to the Sponsor by the investigators of that trial Process any SAEs as per pre-defined process: · Review causality assessments, perform expectedness assessments and categorise SAEs · For CTIMPs report SUSARs to the REC and the CA, for MHRA using the MHRA eSUSAR form; see reference below · For non-CTIMPs report Unexpected and Related SAEs to the REC; see NRES website referenced below · For Medical Devices, report any SAEs to the CA and REC following their guidelines; for the UK see the MHRA website referenced below for further guidance Inform Principal Investigators of any safety issues in a timely fashion; for CTIMPs this includes forwarding information about SUSARs Ensure annual reporting is undertaken as required: · For CTIMPs ensure a DSUR is completed and sent to the CA and REC on an annual basis; see for an optional template UoB-CLN-AES-QCD-004 DSUR template · For non-CTIMPs, ensure safety information is including in the Annual Progress Report and sent to the REC on an annual basis; see the NRES website referenced below for further guidance Where producing an IB for a trial, ensure that the IB is validated at least once a year Where using an existing IB or Summary of Product Characteristics (SmPC), ensure its contents is reviewed on a regular basis; e.g. once a year Where a Data Monitoring Committee is in place, ensure safety information is made available for their review at the scheduled time points Supply information to Sponsor as requested. For UoB (co-)sponsored trials send a copy of the reports to the RGT at the time of reports being sent to the REC and CA (if applicable); the RGT will review their trials database and ensure CIs of trials (co)sponsored by the UoB involving the same IMP are informed of any major safety issues within 5 working days of them having received the report. RGT will also assess the impact upon Sponsorship/Insurance or contractual obligations and respond as necessary. Reports include: · Reports of any major safety issues, e.g. urgent safety measures · Any SUSARs (for CTIMP) or Unexpected and Related Serious Adverse Events (non-CTIMPs); include a note from the CI explaining how this case impacts the safety profile of the study · DSURs (for CTIMPs) or ASRs (Annual Safety Reports) Ensure sites follow up on any AEs/SAEs until resolution or stabilisation o o At the end of the trial If SAE information is kept in a separate system, ensure information is reconciled with the main trial database Ensure SAE forms and related information are archived as part of the TMF Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 6 of 10 Adverse Event Reporting Reporting timelines: For CTIMPs the following timelines apply – Fatal/life threatening SUSAR: initial report to competent authority and REC within 7 days of the Sponsor being notified of the event, and any additional information within 8 days of sending the first report. Non-fatal/non-life threatening SUSAR: report to competent authority and REC within 15 days of the Sponsor being notified of the event. For all other non-CTIMPs only related and unexpected SAEs must be reported to the REC within 15 days of the Sponsor being notified of the event. For Medical Devices, all SAEs need to be reported to the competent authority; in the UK this should be done as soon as possible. Causality assessments in CTIMPs: Causality assessment decisions must be made by a qualified doctor or, when appropriate, a qualified dentist. If the investigator is not a qualified doctor (or dentist), this task must be formally delegated to a qualified doctor (or dentist) who is a member of the research team. The trial delegation log should reflect this. In addition, the EU detailed guidelines clearly state that the causality assessment given by the Principal Investigator should not be downgraded by the Sponsor. If the Sponsor (or CI where this duty is delegated to the CI) disagrees with the Principal Investigator’s causality assessment, the opinion of both parties should be documented, and where the event requires further reporting, the opinion should be provided with the report. Related documents: UoB-CLN-ESD-QCD-001: Protocol template UoB-CLN-AES-QCD-002: SAE form template UoB-CLN-AES-QCD-003: Internal process for SAE handling example UoB-CLN-AES-QCD-004: DSUR template See UoB-CLN-CTM-SOP-001 Clinical Trial Management for further inter-relations References: HRA. (n.d.). During your research project - Safety Information. Retrieved October 17, 2013, from HRA: http://www.hra.nhs.uk/research-community/during-your-research-project/safetyreporting/ Department of Health. (2005, April 24). Research governance framework for health and social care: Second edition. Retrieved February 20, 2012, from Publications policy and guidance: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidanc e/DH_4108962 European Commission. (2010, December). Clinical Investigations: Serious Adverse Event Reporting (including SAE template). Retrieved October 14, 2013, from Guidelines on Medical Devices: http://ec.europa.eu/health/medical-devices/files/meddev/2_7_3_en.pdf European Commission. (2013, October 14). Medical Devices - Regulatory Framework. Retrieved October 14, 2013, from EC Public Health: http://ec.europa.eu/health/medicaldevices/regulatory-framework/index_en.htm European Committee. (2011). ‘Detailed guidance on the collection, verification and presentation of adverse event/reaction reports arising from clinical trials on medicinal products for human use. Retrieved April 15, 2013, from Eudralex Volume 10: http://ec.europa.eu/health/files/eudralex/vol-10/2011_c172_01/2011_c172_01_en.pdf Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 7 of 10 Adverse Event Reporting MHRA. (2012). eSUSAR. Retrieved October 15, 2013, from MHRA electronic reporting site for SUSARs: https://esusar.mhra.gov.uk/ MHRA. (2013, July). Guidance for manufacturers on clinical investigations to be carried out in the UK (including SAE reporting requirements for Medical Devices). Retrieved October 17, 2013, from MHRA: http://www.mhra.gov.uk/home/groups/esera/documents/publication/con007504.pdf MHRA. (2011, July 11). How we regulate devices. Retrieved May 13, 2013 , from MHRA: http://www.mhra.gov.uk/Howweregulate/Devices/ Acknowledgements: The first version of this document and the SAE form template has been developed using examples of and with input from the Birmingham Clinical Trials Unit, Cancer Research UK Clinical Trials Unit and Primary Care Clinical Research and Trials Unit. We would like to thank all staff members within the CTUs and UHB R&D who have been involved in developing these documents for their time and efforts. Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 8 of 10 Adverse Event Reporting Development summary: Author: Name: Wilma van Riel Signature: Function: Clinical Trials Quality Assurance Manager Date: See original copy Reviewed by: Anna Grier, CRCTU Senior Trial Coordinator, Clinical Trials Oversight Committee, LES Research Support Partner See original copy Authorised by: Name: Prof. Pam Kearns Signature: See original copy Function: Chair of Clinical Trials Oversight Committee Date: See original copy Name: Prof. Chris Miall Signature: See original copy Function: Director of Research and Knowledge Transfer, LES Date: See original copy Issue date: 02-Dec-2013 Supersedes: N/A Reason for update: N/A Review of final version: Date: Reviewed by: Signature: Outcome: N/A Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 9 of 10 Adverse Event Reporting Editorial Amendments Tick box if not applicable Reason for update: Administrative update: inclusion of immediate reporting of SAE to Sponsor in process map and coding, links and style updated Date of amendment: 27-Jan-15 Supersedes: UoB-CLN-SOP-002 v1.0 16-Dec-13 – Adverse Event Reporting SOP Editor: Name: Conor McGoldrick Function: Clinical Trials Compliance Officer Date: 27-Jan-15 Signature: See original copy Signature: See original copy Authoriser: Name: Wilma van Riel Function: Clinical Trials Quality Assurance Manager Date: Document code: UoB-CLN-AES-SOP-001 Version no: 1.0 (EAv1.0) Print Date: 09-Feb-16 Page: 10 of 10