New Patient Health Assessment Form
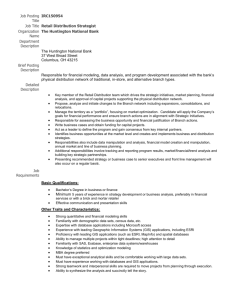
advertisement

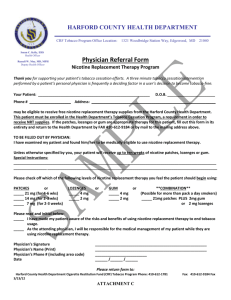
Asheville Internal Medicine Patient Name: __________________________________________ Sex: __ Age: ____ Date of birth: ____________ Address: ______________________________________________________________________________________ Phone (H): (___)__________________ (W) (___)_____________ Social Security #: _________________________ Race: Caucasian Marital Status: Work Status: Student Status: African American Single Full time Married Part time Full time Part time Asian Hispanic American Indian Legally Separated Divorced Not Employed Self Employed Other Widowed Retired Active Duty Not Student Patient’s Employer & Address: ____________________________________________________________________ Spouse’s Employer & Address: ____________________________________________________________________ Emergency Contact (Name, Address, Phone Number): _________________________________________________ _________________________________________________ Relationship to patient: _______________________ If you are ill and cannot take care of yourself, who will help you? _________________________________________ Who referred you to this office? ___________________________________________________________________ All professional services rendered are charged to the patient. We request that you pay for services when rendered unless other arrangements are made in advance. You will be given a copy of your encounter form which contains all information needed to file with your insurance company. The Patient is Responsible For All Charges, Regardless of Insurance Coverage. Medicare ID #____________________________ Policy Holder Name _____________________________________ Other Insurance Company _________________________________ ID # ___________________________________ Policy Holder Name __________________________________________ Group # ___________________________ Address Where Claim to be mailed _________________________________________________________________ Other Ins Company ___________________________________________ ID # ______________________________ Policy Holder Name _______________________________________________ Group # ______________________ Address where claim to be mailed _________________________________________________________________ AUTHORIZATION TO RELEASE INFORMATION: I give my authorization for my medical records to be sent to other doctors I may be seeing. I authorize the use of photostatic copy of this agreement and authorization in lieu of original when necessary. ___________________________________________________ Signature of Patient or Responsible Party ________________________________________ Date AUTHORIZATION FOR PAYMENT: I authorize the release of my medical information necessary to process the claim and request payment of Medicare benefits to the party who accepts assignment. I understand that I am responsible for all charges, regardless of insurance coverage. ___________________________________________________ Signature of Patient or Responsible Party _________________________________________________ Date Social/Cultural History: Do you have any children? ________ If so, how many? ________ Are there any specific personal problems or concerns you would like to discuss? ____________________________ Are there any cultural or religious concerns that you have related to our delivery of care? ____________________ Are there any specific household problems that you would like to discuss? _________________________________ Are there any financial issues that you would like to discuss? ____________________________________________ Have you had any occupational changes? Disabled Unemployed Other__________________________ Have you experienced a recent death of a family member? Spouse Parent Sibling Child Other Any other social issues that you would like to discuss? _________________________________________________ Communication: Language of preference: _________________ Any vision problems that affect your communication. Y N. If yes, please describe________________________ Any Hearing Problems: Y N. If yes, please describe: ___________________________________________ LIST ALL MEDICATIONS YOU ARE CURRENTLY TAKING: (Including exact dosage & frequency) Name Dosage How often Name Dosage How often 1.___________________________________________ 2. _________________________________________ 3. ___________________________________________ 4. _________________________________________ 5. ___________________________________________ 6. _________________________________________ 7. ____________________________________________ 8. _________________________________________ 9. ____________________________________________ 10. _________________________________________ LIST ALLERGIES TO MEDICINES: ___________________________________________________________________ ARE YOU ALLERGIC TO LATEX, IODINE, OR X-RAY DYE? (PLEASE CIRCLE) Y N Personal Medical History: Do you or have you ever had any of the following? Please explain Eye Problems ____________________________ Ulcer/Colitis/Bowel ________________________ Thyroid Disease ___________________________ Diabetes _________________________________ High Cholesterol __________________________ Neurological Disease _____________________ Blood Disease (Anemia/Leukemia) ______________ Skin Disease _____________________________ Depression/Anxiety _______________________ Abuse __________________________________ Illegal Prescription Drug Abuse ______________ GYN Problems (for women only) ____________ Kidney/Bladder Problems ________________________ Ear Problems ___________________________________ Sinus Problems _________________________________ Respiratory Disease (Pneumonia, Bronchitis, etc) ___________ High Blood Pressure _____________________________ Heart Disease (Heart attack, chest pain, ect) _______________ Stroke/ TIA ____________________________________ Circulatory Disease ______________________________ Bone/Joint Disease _____________________________ Alcohol Abuse __________________________________ Other mental health disorders _____________________ Prostate Problems (for men only) __________________ Please list past surgeries, hospitalizations or injuries: Operations/Illness Date Physician/Hospital _____________________________________________________________________________________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ Family Medical History: (Please check if grandparent, parent, sibling or child has a history with these health issues) Heart Disease _______________ High Cholesterol ________________ Glaucoma _________________ High BP ____________________ Lung Disease ___________________ Kidney Disease _____________ Stroke/TIA __________________ Asthma ________________________ Breast Cancer _____________ Diabetes ___________________ Anemia/Blood __________________ Cancer ____________________ Thyroid ____________________ Alzheimer’s Disease ______________ Depression/Anxiety _________ Alcohol Abuse _______________ Drug Abuse _____________________ Other mental health disorder _____________ Any other family medical issues _______________________ Tobacco History: Do you currently use tobacco products? Yes No If yes, please indicate the type of tobacco products below: Cigarettes Pipe Cigars Smokeless Other tobacco products (orbs, strips, sticks, hookah, etc) Packs per day (20 cigarettes/pack): _________________________________________ Bowls per day: _________________________________________________________________ Number per day: _____________________________________________________________ Cans/pouches per day: ______________________________________________________ Amount per day: _____________________________________________________________ Medication used in previous quit attempt: No medication Nicotine patch Nicotine gum Nicotine lozenge Nicotine nasal spray Nicotine oral inhaler Varenicline Bupropion Other: ______________________________________________ Readiness to Quit: Not interested in quitting Would like to quit sometime (but not within the next month) Would like to quit now or soon (within the next month) Other smokers in household? Yes No Fall Risk Assessment: Have you had any falls in the past year? Yes No Do you have any worries about falling or feel unsteady when standing or walking? Yes No If so, please explain ___________________________________________________________________________________________________ Assessment of Risky Health Behaviors: Do you drink alcohol? Y N # of drinks at a time ______ How many days per week? ____________________ When was the last time you had more than 4-5 drinks in one day? never in past 3 months over 3 months How often do you exercise? never rarely 1 to 3 times/month 1 to 3 times/ week 4 to 6 times/week 7 days/week Are you sexually active? Y N Do you have any sexual concerns? Y N Have you ever been treated for a sexually transmitted disease? Y N Do you have any reason to suspect that you have been exposed to HIV or AIDS? Y N Do you handle and control the stress in your life? Y N Do you sleep well at night? Y N How many hours? _______ Have you experienced a serious life event recently (death, divorce, new job, moved, etc?) Y N If yes, please explain ____________________________________________________________________________ Depression Assessment In the past month: Have you often been bothered by feeling down, depressed or hopeless? Y N Have you often been bothered by little interest or pleasure in doing things? Y N Are you generally happy with your life and your current health? Y N When was your last exam? (Indicate Year and Results) EKG: _____________________________________ Physical Exam: _____________________________ Chest X-ray: _______________________________ Pneumonia Vaccine: ________________________ Tetanus Vaccine: __________ Td or Tdap Zostavax: _________________________________ Colonoscopy: _______________________________ Mammogram: _______________________________ Pap Smear: _________________________________ Bone Density: _______________________________ Flu Vaccine: _________________________________ Dental Exam: ________________________________ Advance Care Planning: Do you current have any of the following? Living Will; Five Wishes; DNR; MOST; Health Care Power of Attorney; Other _______________ Review of Systems: Constitutional Good General Health Recent Weight Changes Night Sweats/ Fever Fatigue/Weakness Sleep Problems YN YN YN YN YN Cardiovascular Chest pain Palpitations Heart Trouble Swelling Hands/Feet YN YN YN YN ENT Hearing loss or ringing Sinus Problems Nose Bleeds Sore Throat YN YN YN YN EYES Wear glasses/contacts Blurred/double vision Eye disease or injury Glaucoma YN YN YN YN Respiratory Shortness of breath Cough Wheezing/Asthma Coughing up blood YN YN YN YN Musculoskeletal Muscle pain or cramps Stiffness/swelling joints Joint Pain Trouble walking YN YN YN YN Neurological Frequent headache Paralysis or tremors Convulsions/seizures Numbness/tingling YN YN YN YN Hematologic/Lymphatic Bruise easily YN Enlarged glands YN Gastrointestinal Nausea/vomiting Abdominal pain Constipation Diarrhea Rectal bleeding Integumentary (Skin/Breast) Change in hair or nails YN Rashes or itching YN Breast Lump YN Breast pain/discharge YN Endocrine Excessive thirst Thyroid disease YN YN Psychiatric Insomnia Confusion/Memory loss Depression Genitourinary Blood in urine Kidney stones Testicle pain Abnormal periods YN YN YN YN YN YN YN YN YN YN YN YN __________________________________________ Patient Signature ____________________________ Date __________________________________________ Patient Printed Name ___________________________________________ Physician Signature _____________________________ Date