Family studies of Type 1 diabetes reveal additive and non
advertisement

Family studies of Type 1 diabetes reveal additive and non-additive
effects between MGAT1 and four other polymorphisms
Zhaoxia Yu, Carey F. Li, Haik Mkhikian, Raymond W. Zhou, Barbara L. Newton, Michael
Demetriou
a
Department of Neurology, University of California, Irvine, CA 92869, USA
b
Department of Microbiology & Molecular Genetics, University of California, Irvine, CA 92869,
USA
c
Institute for Immunology, University of California, Irvine, CA 92869, USA
d
Department of Statistics, University of California, Irvine, CA 92869, USA
* Corresponding Author. Tel.: 949-824-9775; fax: 949-824-9847; e-mail: mdemetri@uci.edu
1
Abstract
In a recent study of multiple sclerosis (MS) we observed epistatic, additive and
interaction (non-additive) effects between variants of five genes that converge to induce T cell
hyper-activity by altering Asn-(N) linked protein glycosylation; namely the Golgi enzymes
MGAT1 and MGAT5, cytotoxic T-lymphocyte antigen 4 (CTLA-4), interleukin-2 receptor-α
(IL2RA) and interleukin-7 receptor-α (IL7RA). As the CTLA-4, IL2RA and IL7RA variants have
previously also been associated with Type 1 Diabetes (T1D), we examined the joint effects of the
variants in Type 1 Diabetes. Using a novel conditional logistic regression for family-based
datasets, epistatic, additive and non-additive genetic effects were observed. The MGAT5, IL2RA
and IL7RA variants had point association in MS and T1D, while the MGAT1 and CTLA-4
variants associated with only MS or T1D, respectively. However, consistent with the interactions
we observed in MS, the MGAT1 variant haplotype interacts with CTLA4 (p-value 0.03), and a
combination of IL2RA and IL7RA (p-value 0.05). Analysis of the joint effects of MGAT1,
CTLA4, IL2R, IL7R, MGAT5 and the two interactions using a multiple conditional logistic
regression gives an overall p-value of 5.67x10-10. These data are consistent with defective Nglycosylation of T cells, via interactions of variants in MGAT1, CTLA4, IL2R, IL7R and MGAT5,
contributing to T1D pathogenesis.
2
1. Introduction
With the advancement of high-throughput genotyping technologies, hundreds of common
genetic variants have been identified for human complex traits, such as type 1 diabetes [T1D,
MIM 222100]. However, it has been reported that these genetic variants explain only a small
proportion of heritability [1]. Gene-gene interactions are likely a major factor in explaining the
mystery of missing heritability [1] and thus, characterizing gene-gene interactions is of
fundamental importance to unraveling the etiology of complex human diseases. However,
successfully detecting gene-gene interactions face’s many challenges. For example, a major
constraint is the issue of multiple hypothesis testing. In a genome-wide search for gene-gene
interactions, correcting for the very large number of tests greatly diminishes the power to detect
interactions with moderate effects.
Single-gene disorders displaying Mendelian inheritance disrupt molecular pathways at a
single step. However, a similar degree of pathway disruption may be obtained through small
defects in multiple genes/environmental inputs that combine to disrupt a single pathway. These
interactions may be epistatic, additive or non-additive and may promote disease only when
combined; and therefore poorly detected by GWAS. A functional approach that groups candidate
variants based on a shared ability to alter a common molecular pathway provides an alternative
method to identify interactions. Indeed, we recently reported that multiple environmental factors
(vitamin D3 deficiency and metabolism) and multiple genetic variants (IL-7RA, IL-2RA, MGAT1,
MGAT5 and CTLA-4) converge to dysregulate Golgi N-glycosylation and T cell function in
multiple sclerosis (MS) (REF 4,5). Causality for defective N-glycosylation in MS is supported
by data in mice, where deficiencies in Golgi enzymes (eg Mgat5) induce T cell hyper-activity
and spontaneous autoimmunity, including a spontaneous MS-like disease (Demetriou et al 2001
3
Nature 409, 733-738, Lee et al 2007 J. Biol. Chem. 282, 35361-35372, Grigorian et al New York
Academy of Sciences 1253 49-57). Epistatic, additive and non-additive interactions were
observed. For example, a haplotype of the Golgi N-glycosylation enzyme MGAT1 promotes MS,
alters N-glycosylation, T cell activation thresholds, and surface expression of anti-autoimmune
cytotoxic T-lymphocyte antigen 4 (CTLA-4) in a manner that is sensitive to metabolic conditions,
Vitamin D3 signaling, altered activity of Golgi MGAT5 (rs3814022), the number of N-glycans
attached to CTLA-4 (CTLA-4, rs231775) and interleukin-7/interleukin-2 signaling modulation by
the IL-7R (rs6897932) and IL-2RA (rs2104286) variants. The interaction between the MGAT1
and CTLA-4 variants was epistatic, as CTLA-4 (rs231775) lacks point association with MS. In
contrast, a non-additive interaction was observed between the MGAT1 risk variant and a
combination of the IL-7R and IL-2RA risk variants, a result consistent with their opposing effects
on mRNA levels of the MGAT1 enzyme. The effects of the MGAT5 variant were additive with
the other variants and interactions.
These data suggest that studies only examining point
association, such as GWAS, are unlikely to adequately define heritability.
As genetic risk factors may be shared across different autoimmune diseases [6-9], here
we examine whether the five MS variants also interact in T1D to determine disease susceptibility.
By borrowing the interaction information learned from MS, we avoid conducting a genome-wide
search and significantly reduce the burden of multiple testing. The most common design for
genetic association is the case-control design; however these can be biased by population
stratification. In contrast, a family-based design, such as that of the Type 1 Diabetes Genetics
Consortium (T1DGC), provides inference of association that is robust against population
stratification. A common way to analyze family data is with conditional logistic regression (CLR)
[10,11]. Cordell et al. [12] proposed to use CLR to test genetic interaction between two variants
4
by constructing 15 pseudo controls for each affected child. This approach is difficult to be
generalized to examine multiple variants as the number of pseudo controls for each affected child
grows exponentially with the number of variants. In addition, analyzing linked variants requires
knowledge of recombination rates between variants. One way to avoid these complications is to
match each affected child to the pseudo control whose genotype is formed by all the other nontransmitted alleles by parents. Kotti et al. [13] used this matching strategy to test gene-gene
interactions. We have recently shown that Kotti’s matching strategy is suboptimal for testing
gene-gene interactions (REF). Therefore, to test both additive and non-additive genetic effects
using the multiplex family data collected by the T1DGC, we utilize a novel easy-to-implement
yet efficient method to construct pseudo controls. Using this method, we confirm additive and
non-additive effects of MGAT1, CTLA4, IL2R, IL7R and MGAT5 on T1D risk, with an overall pvalue of 5.67x10-10.
2. Data description
We analyzed Caucasian multiplex families collected by the T1DGC. The SNPs were genotyped
using a method that was previously described [4]. We excluded families with missing parents or
genotyping errors at any of the five SNPs. This lead to 2,858 affected offspring and their parents
from 1,423 families. To test genetic effects, we use conditional logistic regression with a novel
matching strategy, as described in the following section.
3. Statistical Methods
3.1. A novel matching strategy
5
In recent theoretical work [14] we examined and compared conditional logistic regressions under
two matching strategies, the 1:1 matching and the exhaustive matching. Suppose that we are
interested in testing L loci. In the 1:1 matching, we match each affected child to its “anti-self”,
i.e., a pseudo control whose genotype is formed by the nontransmitted alleles. In the exhaustive
matching, we match each affected child to 4L-1 pseudo controls. The two matching strategies at
two SNPs for a case-parent trio are illustrated in Figure 1. Compared with the exhaustive
matching, the 1:1 matching strategy is simpler, more straightforward to implement, and
computationally easier. Furthermore, the 1:1 matching does not require the knowledge of
recombination rates between markers but the exhaustive matching does. Intuitively, the 1:1
matching uses less information from the data. However, we found that the 1:1 matching is as
efficient as the exhaustive matching when the true underlying genetic effects are additive, which
requires that there are no intra- or inter-locus interactions [14]. Thus, when the focus is additive
genetic effects, we can safely use the 1:1 matching; on the other hand, when the focus is nonadditive effects, we should consider the exhaustive matching.
Based upon our prior understanding of MGAT1 and the other genetic variants altering Nglycosylation in MS [4,5], we expect both additive effects and gene-gene interactions between
variants of the following five genes: MGAT1 (rs7726005 and rs2070924), CTLA4 (rs231775),
IL2RA (rs2104286), IL7RA (rs6897932), and MGAT5 (rs3814022). At the individual gene level,
our studies for MS indicate that the MGAT1 IVA/VT-T haplotype (rs7726005 and rs2070924) has
a dominant effect while SNPs rs231775 (CTLA4), rs2104286 (IL2RA), and rs6897932 (IL7RA)
show additive effects (what about MGAT5?). Between genes, we found that the MGAT1 IVA/VTT
haplotype interacts with two sets of SNPs, rs231775 (CTLA4), and a combination of rs2104286
6
(IL2RA) and rs6897932 (IL7RA). In the following we show how this prior information is used to
facilitate our construction of pseudo controls for each affected child in the T1D study.
The rs2070924 SNP in MGAT1 is almost in complete linkage disequilibrium with rs7726005.
The haplotype formed by the rare alleles at the two SNPs shows a dominant effect, indicating
that the exhaustive matching is more efficient than the 1:1 matching; however, the frequency of
the haplotype is rare and in this case a dominant model is close to an additive model. To reduce
the complexity of matching, we use the 1:1 matching at MGAT1, as shown in Figure 2a. For the
MGAT5 rs3814022 variant, the minor C allele shows a recessive protective effect [15]; therefore
we use exhaustive matching, which is 1:3 at a single locus, matching for rs3814022, as illustrated
in Figure 2b. Because there was no evidence of genetic interaction among rs231775 (CTLA4),
rs2104286 (IL2RA), rs6897932 (IL7RA), and rs3814022 (MGAT5), we assume that the alleles at
these SNPs are co-transmitted from parents to offspring. As a result, the matching strategy for
rs231775 (CTLA4), rs2104286 (IL2RA), and rs6897932 (IL7RA) follows that of rs3814022
(MGAT5), as shown in Figure 2c. Finally, because we want to test gene-gene interactions
between MGAT1 and the other SNPs, we consider the exhaustive matching between MGAT1 and
the combination of the other four SNPs, which leads to a 1:7 matching. Note that the five genes
are in linkage equilibrium. Thus, under the null hypothesis, the 8 possible offspring genotypes,
including that of an affected child and his/her 7 matched pseudo controls, are equally likely. We
use H(GP) to denote the 8 genotypes given the parental genotype GP. The final matching strategy
to identify both additive and non-additive multi-locus genetic effects of these genes is
summarized in Figure 2d.
7
3.2. Conditional logistic regressions (CLR)
Matched case-control data are often analyzed by conditional logistic regressions. Let GiO be the
genotype of the ith child among n total affected children; and GiP be the genotype of the parents
of the ith affected child. Using the matching strategy we described above the likelihood function
of association parameters is
n
L( )
i 1
exp( GiO )
.
exp( Gi* )
{Gi*:Gi*H ( GiP )}
The form of and GiO depends on our model. For example, when testing the association of
rs3814022 (MGAT5) and T1D, because the minor allele C is the protective allele with a recessive
effect, GiO is 1 if the offspring has at least one copy of the G allele and 0 otherwise;
correspondingly, is the log of genotype relative risk (GRR) for carriers of the G allele to those
non-carriers. Another example, when testing interaction between the MGAT1 IVA/VT-T haplotype
and rs231775 (CTLA4), GiO is a vector of numerical values with the three elements be indicator
for the presence of the MGAT1 IV/V haplotype, the number of copies of the major allele of
rs231775 (CTLA4), and the product of the first two numbers, respectively. Correspondingly,
is a vector of coefficients corresponding to the main effect of the MGAT1 IV/V haplotype, the
main effect of rs231775 (CTLA4), and the interaction of the two variants, respectively.
We characterize the significance of additive and non-additive effects using p-values. P-values of
individual terms in a multiple CLR are calculated using the Wald test. When examining the joint
effect of multiple terms we use the likelihood ratio test. Conditional logistic regressions were
8
fitted using the “clogit” function in the Survival package in R (http://
cran.r-
project.org/package=survival).
4. Results
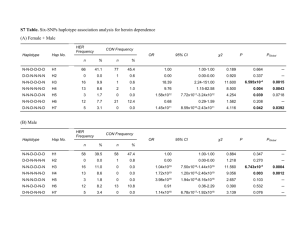
4.1 Effects of individual variants
We first examine the individual effects of the five variants. All variants are significantly
associated with T1D except the MGAT1 IVA/VT-T haplotype. This differs from MS, where all
variants were associated except CTLA-4. We use the risk alleles (column 3 of Table 1) as the test
alleles and the protective alleles as the reference alleles. Association between T1D and CTLA4,
IL2RA, and IL7RA has been reported by many groups, such as [2,3]. In a previous analysis of the
T1DGC data, we found that the minor allele C of rs3814022 [MGAT5] shows a protective and
recessive effect for T1D [15]. Thus here we test the dominant effect of the major allele, i.e., the
G allele. The GRR (define GRR) for subjects with the G allele to those without is 1.40 with a 95%
CI [1.16, 1.70]. The p-value is 4.50x10-4, indicating that the G allele is likely to be associated
with a risk factor for T1D. Note that in a recent study we found that the allele C is a risk allele
for MS. The opposite direction is not surprising. As reported in [6,8], many confirmed loci of
MS and T1D show opposite directions, which could be important in pathogenic processes of
complex diseases. Table 1 demonstrates that MGAT1 is not significant, which also differs from
MS. Therefore, we next examined for epistatic interaction of MGAT1 with the other variants. .
4.2 Gene-gene interactions and joint effects
Motivated by the interactions between MGAT1 and CTLA4, IL2RA, and IL7RA for MS
susceptibility, here we test their genetic interactions for T1D susceptibility.
Although the
9
MGAT1 IVA/VT-T haplotype does not show point association with T1D, it is a protective, neutral,
and risk allele for AA, AG, and GG CTLA-4 genotypes, respectively. For subjects with the AG
genotype at rs231775 (CTLA-4), the MGAT1 IVA/VT-T haplotype shows no association with T1D;
for subjects with the AA genotype, i.e., the low risk group based on CTLA-4, the MGAT1
IVA/VT-T haplotype leads to increased risk of T1D with a GRR 1.47 (p-value=0.023); for subjects
with the GG genotype, i.e., the high risk group based on CTLA-4, the MGAT1 VA/VT-T haplotype
has a protective role for T1D with a GRR 0.58 (p-value=0.028). The different effects of the
MGAT1 VA/VT-T haplotype under the three CTLA-4 genotypes suggest a gene-gene interaction
between the two variants. The p-value for interaction is 0.032. Stratified point estimates of GRRs,
95% confidence intervals, and p-values can be found in Table 2.
One of our recent studies showed that the MGAT1 IVA/VT-T haplotype also interacts with a
combination of the IL2RA and IL7RA risk alleles [4]. Our conditional logistic regression
indicates that the MGAT1 IVA/VT-T haplotype also show differential effects on T1D
susceptibility between subjects with four risk alleles of IL2RA and IL7RA and other subjects. The
MGAT1 IVA/VT-T haplotype increases T1D risk for subjects in high risk based on IL2RA and the
IL7RA; it has a protective risk in the rest of the population, as can be seen from the point
estimates of the GRRs in Table 3. Testing the interaction between them leads to a p-value of
0.052.
Since the variants we considered here are in linkage equilibrium, we expect the interactions we
observed cannot be explained by each other. To confirm this and evaluate the overall impact of
the variants, we fit a multiple CLR with the five variants and the two interactions. Table 4
10
indicates that the point estimations of the GRRs and p-values for the five variants in the multiple
CLR are similar to those from individual CLRs.
The two interaction terms are significant in the multiple CLR, indicating that they are still
important after accounting for the main effects, consistent with what we observed from Tables 2
and 3. Therefore, we used a likelihood ratio test of two degrees of freedom to examine the joint
effect two interaction terms. The p-value based on the likelihood ratio test is 0.014. Finally, we
use a likelihood ratio test of seven degrees of freedom to test the joint effect of both main and
interaction effects. The p-value is 5.67x10-10.
Discussion
In this article we present two gene-gene interactions that are involved in dysregulating Nglycosylation and T1D susceptibility. While validity of the interactions needs to be confirmed by
independent studies, our analysis is knowledge-driven and is motivated by the fact that genegene interactions were observed in MS. It is known that both MS and T1D are autoimmune
diseases and they share many common pathways. Different from a genome-wide search for genegene interactions, our analysis avoids multiple testing thus potentially improves power. We also
examined the African American families collected by the T1DGC. In this data set, there are 58
affected African American children that have both parents genotyped. Because of this small
sample size, no variant or interaction was significant at the 0.05 level of significance. However,
the directions of the point estimates of the GRRs for the interactions agree with what were
observed here. This provides another encouraging evidence that the observed interactions are
likely to be true.
11
There were several important differences between the results in MS and T1D. Point association
of the MGAT1 IVA/VT-T haplotype was observed in MS but not T1D, while the G allele of CTLA4 (rs231775) associated with T1D but not MS; yet in both diseases epistatic interaction was
observed between the two variants. The MGAT1 IVA/VT-T haplotype enhanced risk of MS in
combination with the GG and AG genotypes of CTLA-4 (rs231775), whereas a protective
interaction with the GG genotype was present in T1D. This likely arises from differences in
metabolism between T1D and MS coupled with the molecular mechanisms by which the MGAT1
IVA/VT-T haplotype and CTLA-4 (rs231775) alter N-glycosylation and cell surface expression of
the CTLA-4 protein in T cells. The MGAT1 IVA/VT-T haplotype is a gain of function that
increases mRNA and protein levels of the Golgi enzyme Mgat1. When metabolism limits
substrate availability (ie UDP-GlcNAc derived from glucose) to the Golgi, the MGAT1 IVA/VT-T
gain of function haplotype paradoxically lowers N-glycan branching by limiting UDP-GlcNAc
availability to downstream Golgi enzymes, resulting in reduced cell surface expression of the
anti-autoimmune CTLA-4 protein. The G allele of CTLA-4 (rs231775) decreases the number of
N-glycans attached to CTLA-4 by 50%, thereby reducing surface expression of the CTLA-4
protein. Thus, when metabolism limits Golgi substrate (UDP-GlcNAc) availability, the MGAT1
IVA/VT-T haplotype and the G allele of CTLA-4 (rs231775) combine to lower CTLA-4 cell
surface expression (Mkhikian et al 2011), consistent with the genetic interaction observed in MS.
In contrast, when metabolism increases Golgi UDP-GlcNAc substrate supply, as occurs with
high glucose levels present in T1D, the MGAT1 IVA/VT-T haplotype has the opposite effect on Nglycan branching and CTLA-4 surface expression and therefore is expected to counteract the G
allele of CTLA-4 (rs231775), consistent with the protective genetic interaction observed in T1D.
12
Most existing multi-locus methods for family data only provide an overall significance of
multiple loci or specific combinations of alleles. Examples of such methods include haplotypebased methods [16-22], genotype-based methods[22-26], family-based multiple dimension
reduction [27], and contrasting linkage disequilibrium [28]. Compared to these existing methods
the method we used here has two advantages. First most of existing multi-locus methods are
based upon the 1:1 matching, which is not efficient for testing non-additive effects. Second,
these methods are mainly for hypothesis testing; our method, by contrast, not only provides
significance level of main, interaction, and joint effects, but also provides points estimates of
GRRs.
13
Figure 1
Aa
Bb
Aa
BB
AA
Bb
H E ( Aa, Bb; Aa, BB )
aa aa aa aa Aa Aa Aa Aa Aa Aa Aa Aa AA AA A
BB BB Bb Bb BB BB Bb Bb BB BB Bb Bb BB BB Bb
A
: the affected child
H1 ( Aa, Bb; Aa, BB )
: the “anti-self” of the affected child
Figure 1: The 1:1 and the exhaustive matching strategies for a case-parents trio at two SNPs.
Suppose that SNP 1 has A and a alleles and SNP2 has B and b alleles. H1: all possible offspring
genotypes given the couple’s genotypes under the 1:1 matching; HE: all possible offspring
genotypes given the couple’s genotypes under the exhaustive matching. Under the null
hypothesis of no association, the two genotypes in H1 are equally likely; under the null
hypothesis of no association and linkage equilibrium between the two SNPs, the 16 genotypes in
HE are equally likely.
Figure 2
Figure 2:
14
15
Table 1: Individual genetic effects
alleles
MGAT1 IVA/VT-T
(rs7726005, rs2070924)
rs231775 (CTLA-4)
A, G
rs2104286 (IL2RA)
A, G
rs6897932 (IL7RA)
C, T
rs3814022 (MGAT5)
C, G
freq
GRR
95% CI
p-value
0.039
G: 0.414
A: 0.775
C: 0.751
G: 0.725
1.05
1.17
1.24
1.11
1.40
0.86-1.27
1.08-1.26
1.14-1.35
1.02-1.21
1.16 -1.70
0.654
6.40 x10-5
8.23 x10-7
0.015
4.50 x10-4
Table 2: The effects of MGAT1 IVA/VT-T, stratified on CTLA4 genotypes
CTLA-4 genotypes
GRR of MGAT1 IVA/VT-T
Est
95% CI
p-value
AA (2)
1.47
1.05-2.06
0.023
AG (1)
1.00
0.75-1.33
1.000
GG (0)
0.58
0.36-0.95
0.028
The p-value for interaction is 0.032.
Table 3: The effects of MGAT1 IVA/VT-T, stratified on IL* genotypes
IL*
GRR of MGAT1IVA/VT-T
Est
95% CI
p-value
4
1.28
0.94-1.74
0.118
<4
0.89
0.69-1.15
0.362
The p-value for interaction is 0.052.
*: IL=IL2RA+IL7RA
Table 4:
Variable
Est
95% CI
P-value
MGAT1 IVA/VT-T
1.08 0.80-1.47 0.611
CTLA-4
1.17 1.08-1.27 1.22x10-4
IL2RA
1.20 1.09-1.31 9.41 x10-5
IL7RA
1.09 0.99-1.18 0.084
MGAT5
1.40 1.15-1.71 7.66x10-4
MGAT1 IVA/VT-T
1.41 1.02-1.96 0.037
*CTLA-4
MGAT1 VA/VT-T *(IL=4) 0.79 0.62-1.00 0.048
The p-value (LRT) for the two interaction terms is 0.014. The p-value (LRT) for the joint effect
and additive and non-additive effects is 5.672x10-10.
16
1
Manolio TA, Collins FS, Cox NJ, Goldstein DB, Hindorff LA, Hunter DJ, McCarthy MI, Ramos EM,
Cardon LR, Chakravarti A, Cho JH, Guttmacher AE, Kong A, Kruglyak L, Mardis E, Rotimi CN, Slatkin M,
Valle D, Whittemore AS, Boehnke M, Clark AG, Eichler EE, Gibson G, Haines JL, Mackay TFC, McCarroll SA,
Visscher PM: Finding the missing heritability of complex diseases. Nature 2009;461:747-753.
2
Pociot F, Akolkar B, Concannon P, Erlich HA, Julier C, Morahan G, Nierras CR, Todd JA, Rich SS,
Nerup J: Genetics of type 1 diabetes: What's next? Diabetes 2010;59:1561-1571.
3
Santiago JL, Alizadeh BZ, Martinez A, Espino L, de la Calle H, Fernandez-Arquero M, Figueredo
MA, de la Concha EG, Roep BO, Koeleman BPC, Urcelay E: Study of the association between the capslil7r locus and type 1 diabetes. Diabetologia 2008;51:1653-1658.
4
Mkhikian H, Grigorian A, Li CF, Chen HL, Newton B, Zhou RW, Beeton C, Torossian S, Tatarian GG,
Lee SU, Lau K, Walker E, Siminovitch KA, Chandy KG, Yu ZX, Dennis JW, Demetriou M: Genetics and the
environment converge to dysregulate n-glycosylation in multiple sclerosis. Nat Commun 2011;2
5
Li CF, Zhou RW, Mkhikian H, Newton BL, Yu Z, Demetriou M: Hypomorphic mgat5
polymorphisms promote multiple sclerosis cooperatively with mgat1 and interleukin-2 and 7 receptor
variants. J Neuroimmunol 2013;256:71-76.
6
Cotsapas C, Voight BF, Rossin E, Lage K, Neale BM, Wallace C, Abecasis GR, Barrett JC, Behrens T,
Cho J, De Jager PL, Elder JT, Graham RR, Gregersen P, Klareskog L, Siminovitch KA, van Heel DA,
Wijmenga C, Worthington J, Todd JA, Hafler DA, Rich SS, Daly MJ, Consortia FN: Pervasive sharing of
genetic effects in autoimmune disease. Plos Genet 2011;7
7
Smyth DJ, Plagnol V, Walker NM, Cooper JD, Downes K, Yang JHM, Howson JMM, Stevens H,
McManus R, Wijmenga C, Heap GA, Dubois PC, Clayton DG, Hunt KA, van Heel DA, Todd JA: Shared and
distinct genetic variants in type 1 diabetes and celiac disease. New Engl J Med 2008;359:2767-2777.
8
Sirota M, Schaub MA, Batzoglou S, Robinson WH, Butte AJ: Autoimmune disease classification by
inverse association with snp alleles. Plos Genet 2009;5
9
Todd JA: Etiology of type 1 diabetes. Immunity 2010;32:457-467.
10
Self SG, Longton G, Kopecky KJ, Liang KY: On estimating hla/disease association with application
to a study of aplastic anemia. Biometrics 1991;47:53-61.
11
Schaid DJ, Sommer SS: Genotype relative risks: Methods for design and analysis of candidategene association studies. Am J Hum Genet 1993;53:1114-1126.
12
Cordell HJ, Clayton DG: A unified stepwise regression procedure for evaluating the relative
effects of polymorphisms within a gene using case/control or family data: Application to hla in type 1
diabetes. Am J Hum Genet 2002;70:124-141.
13
Kotti S, Bickeboller H, Clerget-Darpoux F: Strategy for detecting susceptibility genes with weak
or no marginal effect. Hum Hered 2007;63:85-92.
14
Yu ZX, Deng L: Pseudosibship methods in the case-parents design. Stat Med 2011;30:3236-3251.
15
Yu z, Gillen D, Li CF, Demetriou M: Incorporating parental information into familly-based
association tests. Biostatistics 2013
16
Zhao H, Zhang S, Merikangas KR, Trixler M, Wildenauer DB, Sun F, Kidd KK:
Transmission/disequilibrium tests using multiple tightly linked markers. Am J Hum Genet 2000;67:936946.
17
Allen AS, Satten GA: Statistical models for haplotype sharing in case-parent trio data. Hum
Hered 2007;64:35-44.
18
Zhang S, Sha Q, Chen HS, Dong J, Jiang R: Transmission/disequilibrium test based on haplotype
sharing for tightly linked markers. Am J Hum Genet 2003;73:566-579.
19
Van der Meulen MA, te Meerman GJ: Haplotype sharing analysis in affected individuals from
nuclear families with at least one affected offspring. Genet Epidemiol 1997;14:915-920.
17
20
Dudbridge F, Koeleman BP, Todd JA, Clayton DG: Unbiased application of the
transmission/disequilibrium test to multilocus haplotypes. Am J Hum Genet 2000;66:2009-2012.
21
Knapp M, Becker T: Family-based association analysis with tightly linked markers. Hum Hered
2003;56:2-9.
22
Fan R, Knapp M, Wjst M, Zhao C, Xiong M: High resolution t2 association tests of complex
diseases based on family data. Ann Hum Genet 2005;69:187-208.
23
Chapman JM, Cooper JD, Todd JA, Clayton DG: Detecting disease associations due to linkage
disequilibrium using haplotype tags: A class of tests and the determinants of statistical power. Hum
Hered 2003;56:18-31.
24
Zhang Z, Zhang S, Sha Q: A multi-marker test based on family data in genome-wide association
study. Bmc Genet 2007;8:65.
25
Shi M, Umbach DM, Weinberg CR: Identification of risk-related haplotypes with the use of
multiple snps from nuclear families. Am J Hum Genet 2007;81:53-66.
26
Lee WC: Testing for candidate gene linkage disequilibrium using a dense array of single
nucleotide polymorphisms in case-parents studies. Epidemiology 2002;13:545-551.
27
Cattaert T, Urrea V, Naj AC, De Lobel L, De Wit V, Fu M, Mahachie John JM, Shen H, Calle ML,
Ritchie MD, Edwards TL, Van Steen K: Fam-mdr: A flexible family-based multifactor dimensionality
reduction technique to detect epistasis using related individuals. Plos One 2010;5:e10304.
28
Yu Z, Wang S: Contrasting linkage disequilibrium as a multilocus family-based association test.
Genet Epidemiol 2011;35:487-498.
18