Biomimetics in dentistry
advertisement

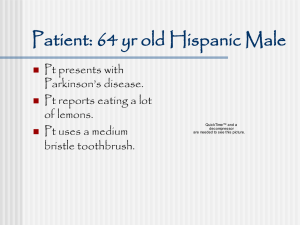
“Biomimetics in dentistry” Biomimetics is a term coined by Otto Schmitt in the 1950’s, while studying the nerves in a squid. He attempted to copy and design an artificial device that could replicate the same process of synaptic impulse. It literally means to mimic life. It is considered the study of natural structural processes to try to mimic or replicate it artificially in an attempt to restore the same function or aesthetics. It is synonomous with biomimicry, biomechanics and biomimesis. Age, disease and traditional restorations can cause further problems to the existing tooth structure. As teeth have no natural method of repair, biomimetic principles should be used to artificially repair the tooth to its natural functions and aesthetics. There are two aspects to biomimetics in Dentistry. The lost or missing dental tissue is restored, leading to the full return of function and aesthetics to the tooth. Or the material used can regenerate, replicate or mimic the missing dental tissue closely. Restorative Dentistry The physiological performance of intact teeth is the result of intimate and balanced relationships between biological, mechanical, functional and esthetic parameters. Natural teeth, through the optimal combination of enamel and dentin, constitute the perfect and unmatched compromise between rigidity, strength and resilience (Magne, 2002)1. Therefore a biomimetic approach to restorative dentistry would mean aesthetic and functional restorative materials similar to the natural tooth and its individual layers of dentine and enamel. This would exclude amalgam and other precious and non precious metal-based materials as they do not mimic the natural tooth in terms of aesthetics or properties. In 2006 Magne said “The goal of biomimetics in restorative dentistry is to return all of the prepared dental tissues to full function by the creation of a hard tissue bond that allows functional stresses to pass through the tooth, drawing the entire crown into the final functional biologic 1 2 and esthetic result The intact tooth in its ideal hues and shades, and perhaps more importantly in its intracoronal anatomy, mechanics and location in the arch, is the guide to reconstruction that determines success.”6,10. In 1956 Vale tested the biomechanics of posterior teeth. He deduced that teeth which were prepared to a certain degree became less resistant to occlusal forces2. In 1971 Grimaldi tested teeth which were unrestored, prepared and restored to see how they functioned and the biomechanics of the teeth. There have been other authors since who have investigated the biomechanics/biomimetics of teeth and restorations345. According to Magne and Douglas in 1999, teeth have a good equilibrium of strength, flexure and stiffness. They are resistant to fracture and flex to a certain degree. Dental disease, age and restorations weaken these factors6. There are certain types of restorations that can restore these factors to a better degree than other types of restorations7.By 2007 Pascal Magne did the same as Vale, but using new technology in virtual computer programming8,9. As previously mentioned, according to Magne,“the goal of biomimetics in restorative dentistry is to return all of the prepared dental tissue to full function by creating a hard tissue bond that allows functional stress to pass through the tooth, drawing the entire crown into the final functional and esthetic result”6,10. Therefore there is a large element of biomimetics on the preparation of the tooth, chemical bonding to the tooth and materials used to restore the tooth, but also the relationship between the materials. Materials We are aware that there may be some regeneration or stimulation of dentine with certain dental materials11. There are also materials that can actually remineralise acid etched dentine12. These materials would be classified as being “biomimetic”. There are still long term studies on going with the regeneration of tooth substance. Other biomimetic materials are materials used to restore the tooth which closely mimic enamel and dentine. As previously mentioned the tooth structure itself is used as a guide to reconstruct the diseased or missing parts to its original strength and properties. Adhesive bonds, glass ionomers, composites and ceramics are utilised to reconstruct and replicate these features in a 31 October 2011 3 natural tooth. The table below demonstrates the similarity of these artificial materials to natural tooth substance. Materials Table 1 From the table we can see that feldspathic ceramics are the closest to mimic enamel and hybrid composites are the closest to mimic dentine. However it is has been also advised to use composites131415 for small loss in tooth tissue and Glass ionomer cements (GIC) as a base layer161718. Magne also demonstrated that anterior teeth deform and flex more than posterior teeth. The loss of tooth substance and the properties of the tooth in anterior and posterior teeth can be restored by good bonding of porcelain to the tooth. Magne demonstrated that the porcelain not only bond well and restores the aesthetics but also restores and strengthens the teeth with porcelain veneers and adequate bonding techniques6,7,8,9,19,35. The restored tooth even behaves like the natural tooth with catastrophic testing1. Composite resins are now displaying favourable properties and longevity on par to amalgam2021. The technique involves minimal preparation22 decreasing pulpal involvement and decreasing the prognosis of fractures2324. It therefore preserves tooth substance and 31 October 2011 4 vitality. Some authors argue that composite can actually strengthen the remaining tooth structure when placed well with reduced c-factors and shrinkage2526. Small to moderate sized restorations should be restored with composite6. Glass Ionomer Cements (GIC) is considered to be useful in deep class I or II cavities to fill up the base as lining material6. They are also useful as buccal class V cavities. Composite can then be bonded over as a closed sandwhich technique. GIC can also be used to fill any undercuts for preparation of indirect restorations6. GIC releases fluoride, is bacteriacidal, stimulates sclerotic dentine and also has properties similar to dentine. As such would fit the definition of biomimetic27. However as their tensile strength is poor they are not advocated in use of high occlusal stress and force. Biodentine is a new material that may replace GIC as a liner in deep fillings28, but further research is needed. GIC is currently being the main tool for advocates of minimum invasive dentistry293031 which is under the umbrella of biomimetic restorative dentistry. Magne argues that porcelain bonded to metal and other substances like amalgam6,32 which do not follow biomimetic principles and do not attempt to restore the tooths natural properties. He also argues that gold is excessively stiff, thereby also not following biomimetic principles33. As these materials also are not bonded with the existing tooth structure there is a higher likelihood of cracks, leakage and bacterial invasion causing further deterioration19,25. This is then repaired with the same materials which fail again but with less tooth substance leading to tooth loss. Biomimetics prevents and stops the repair-replace-repair cycle of destruction and deterioration. Magne and other authors argue that the occlusal stresses of the tooth should pass through the whole tooth with a strength bond21,22. Without this bond the restoration will not be successful34,35,36. Therefore producing high strength bonds from tooth to restoration and /or restoration to restoration is the key. Bonding technology and bond strengths have increased tremendously since it began. Buonocore started in 195537 and since then techniques and materials have developed. There is self etch, total etch, all in one bonding systems and a mixture of the different types. We know that the strongest bonds are in the total etch system with separate etch, prime and bond38,39. As such we can now be more confident in bonding composite to dentine and enamel. Dentine bonding agents (DBA) are now bonding porcelain and composite restorations to a similar 31 October 2011 5 way that enamel is bonded to dentine at the Dentinoenamel junction40. Magne has incorporated Immediate Dentine Sealing (IDS) as the technique advocated in bonding indirect porcelain restorations32. IDS is essentially a total etch technique immediately after preparation of the tooth. IDS has a number of advantages:1 It bonds to freshly cut dentine which produces the strongest bonds414243. 2 There is precuring of the DBA after tooth preparation and before final impressions, which increases bond strength44,45,46,47,48. 3 IDS allows maturation of the bond without occlusal stress, improving strength of the bond49,50. 4 IDS protects against bacterial leakage during temporisation which could contaminate the bond51. IDS should be used in conjunction with proper preparation of the fitting surface of the porcelain (etching and silanisation of porcelain). There are some disadvantages with IDS and the total etch technique. Both are very technique sensitive. It has been noted that it works well in expert hands but less so in less experienced operators. It has the potential to contaminate the impression material and the DBA during the temporisation. The DBA may actually bond to the temporary restorations themselves. There is also separate session to prepare the porcelain fitting surface32. Current practices of preparation of the tooth by the modern dental drill can cause further harm to the tooth. Drilling the tooth can cause fractures, and heat which can make repair more difficult. Other more biomimetic methods to prepare teeth are being investigated, such as laser, air abrasion etc that may do less harm and preserve more tooth tissue. But currently nothing is comparable in terms of popularity, versatility and costs than the modern dental drill. 31 October 2011 6 Outside Prosthetic Dentistry Biomimetic dentistry also includes regeneration of the periodontium and alveolar bone surrounding the teeth. One of the most common techniques used is bone grafts for alveolar defects. This is utilised in oral surgery, periodontics and endodontics and is sometimes called guided bone regeneration (GBR). These grafts may be animal or human bone grafts which lay down bone matrix resulting in new bone. These grafts have osteogenic features. Other graft material may be artificial which signals the host to stmulate bone growth in that area. These are osteoinducive materials. These materials can be classed as allografts (human donor), autogenous (from the patient), alloplast (synthetic) and xenografts (animal). Sometimes bony healing cannot occur due to connective tissue growth into the bony defect. This can be prevented by the use of barrier membranes in conjunction to the bone graft material to prevent cells that form connective tissue into the defct, thereby allowing just cells that form periodontium and alveolar bone to form. Barrier membrane come in various different materials but are classified as resorbable (Alpha-hydroxyacids, Amino acid based polymers, Natural or synthetic types), or non resorbable (EPTFE, Ceramic, Titanium mesh)52. As well as regeneration of bone there are techniques to regenerate gingival tissues. This will allow gingival coverage in gingival recession areas. They are sometimes called Guided Tissue Regeneration (GTR). This Allows more aesthetic, functional and natural gingival tissue which would otherwise cause aesthetic and functional problems such as sensitivity and loss of attachment. Such techniques include free gingival grafts and connective tissue grafts (autogenous and artificial which increase attached gingivae) and a variety of root coverage techniques53. Recombinant human bone morphogenetic protein (BMP) 2, BMP 7 AND BMP 4 has been known to induce new dentine formation in exposed pulpal tissue54 The pulpal tissue actually changes into odontoblasts. The BMP have also been used to produce alveolar bone and cementum on teeth in baboon studies55. This is a exciting propect and could change the practice of endodontics, periodontics and oral surgery. However there is still a lot more research needed and currently it has been performed on canine and ape studies. Platelet rich plasma (PRP) is being researched in animal and human studies. PRP is made from the patient’s own blood and certain factors are separated to use on the patient. Other factors include platelet-derived growth factor, transforming growth factor, insulin-like growth 31 October 2011 7 factor, and epidermal growth factor. These factors help speed recovery, haemostasis and wound healing56. There has been a large number of studies and research developing in other specialities of dentistry and medicine. There are a number of materials being investigated and studied that can regenerate human dental and gingival tissue, but further research is needed before application in routine dentistry. 31 October 2011 8 References 1 Magne P, Belser U. Bonded Porcelain Restorations in the anterior dention- A Biomimetic Approach. Chicago: Quintessence Publishing Co., 2002. 2 Vale WA (1956) Cavity Preparation. Irish Dental Review 2,33—41. 52 3 Int Dent J. 1991 Feb;41(1):25-32. Biomechanics of the intact, prepared and restored tooth: some clinical implications. Hood JA 4 Morin DL, Douglas WH, et al, Biophysical stress analysis of restored teeth: experimental strain measurements. Dent Mater 4:41-8, 1988. 5 Assif D, Marshak BL, Pilo R, Cuspal flexure associated with amalgam restorations. J Prosthet Dent 63:258-62, 1990 6 Composite Resins and Bonded Porcelain: The Postamalgam Era? Pascal Magne, 2006.VOL.34.NO.2.CDA.JOURNAL 7 Int J Prosthodont. 1999 Mar-Apr;12(2):111-21. Porcelain veneers: dentin bonding optimization and biomimetic recovery of the crown. Magne P, Douglas WH. 8 Efficient 3D finite element analysis of dental 31 October 2011 9 restorative procedures using micro-CT data Pascal Magne dental materials 2 3 ( 2 0 0 7 ) 539–548 9 Dent Mater. 2007 May;23(5):539-48. Epub 2006 May 26. Efficient 3D finite element analysis of dental restorative procedures using micro-CT data. Magne P. 10 Magne P. Esthetic and Biomimetic Restorative Dentistry: Manual for Posterior Esthetic Restorations. Los Angeles: USC School of Dentistry, 2006 11 Du C, Moradian-Oldak J. Tooth regeneration: challenges and opportunities for biomedical material research. Biomed Mater. 2006;1(1):R10-R17. 12 Tay FR, Pashley DH. Guided tissue remineralisation of partially demineralised human dentine. Biomaterials. 2008;29(8):1127-1137. 13 Keen DS, von Frauhofer JA, Parkins FM. Air-abrasive “etching”: Composite bond strengths J Dent Res. 1994;73:131 14 Berry EA, Ward M. Bond strength of resin composite to air-abraded enamel. Quintessence Int. 1995;26:559–62 15 Roeder LB, Berry EA, You I, Powers JM. Bond strength of composite to air-abraded enamel and dentin. Oper Dent. 1995;20:186–90. 31 October 2011 10 16 Clinical requirements for a successful ‘sandwich’— dentine to glass ionomer cement to composite resin† Australian Dental Journal Volume 34, Issue 3, pages 259–265, June 1989 G. J. Mount 17 Glass-ionomer Restoratives: A Systematic Review of a Secondary Caries Treatment Effect R.C. Randall JDR February 1999 vol. 78 no. 2 628-637 18 A 6-year evaluation of a direct composite resin inlay/onlay system and glass ionomer cement-composite resin sandwich restorations 1994, Vol. 52, No. 6 , Pages 368-376 Jan W. V. van Dijken† 19 Alleman DS, Magne P. A systematic approach to deep caries removal end-points: the peripheral seal concept in adhesive dentistry. Academy of Minimally Invasive Biomimetic Dentistry, 2011 20 Walls AWG, Murray JJ et al. The Management of occlusal caries in permanent molars. A clinical trial comparing a minimal composite restoration with an occlusal amalgam restoration. Br Dent J 164(9):288-292, 1988. 21 A retrospective clinical study on longevity of posterior composite and amalgam restorations, Niek J.M. Opdam 31 October 2011 11 Dental Materials Volume 23, Issue 1, January 2007, Pages 2-8 22 Malterud MI. Minimally invasive restorative dentistry: a biomimetic approach. Pract Proced Aesthet Dent. 2006;18(7):409-414. 23 McCullock AJ, Smith BG, In vitro studies of cusp reinforcement with adhesive restorative material. Br Dent J 161:450-2, 1986. 24 Macpherson LC, Smith BG, Reinforcement of weakened cusps by adhesive restorative materials: an in vitro study. Br Dent J 178:341-4, 1995. 26 Morin D, Delong R, Douglas WH. Cusp reinforcement by the acid-etch technique. J Den Res 1984;63:1075-1078 27 Ngo H. Biological properties of glass-ionomers. In: An atlas of glass-ionomer cements. A clinician's guide. GJ Mount (eds). 2002, Martin Dunitz, London. p. 43-55 28 Antibacterial activity of new Ca-based cement compared to other cements 31 October 2011 12 E. VALYI, N. PLASSE-PRADELLE, D. DECORET, P. COLON, and B. GROSGOGEAT, Université Claude Bernard Lyon1, Lyon, France, Department of Operative and Preventive Dentistry University of Paris V, Villeurbanne, France, Université Claude Bernard Lyon1, UFR d'odontologie, Lyon, France, Université Claude Bernard Lyon1, Laboratoire des Multimatériaux et Interfaces (LMI), UFR d'Odontologie UMR CNRS 5615, Lyon, France 29 Quintessence Int. 2000 Oct;31(9):621-9. Minimal intervention: advanced lesions. Mount GJ, Ngo H 30 J Dent. 2006 Sep;34(8):608-13. Epub 2006 Mar 15. Chemical exchange between glass-ionomer restorations and residual carious dentine in permanent molars: an in vivo study. Ngo HC, Mount G, Mc Intyre J, Tuisuva J, Von Doussa RJ 31 Dent Update. 2010 Dec;37(10):651-2, 654-6. Caries control from cradle to grave. Kidd E. 32 Allsopp JF, Matthews JB, Marquis PM & Frame JW. Failure of amalgam restorations and their replacement in general practice. (Abstract No. 35) J Dent Res 75(3):871-878,1996 31 October 2011 13 33 The Natural Beauty of Tooth Colored Fillings Dentistry and Oral Health Magazine 11/1/2009 P Magne 34 Unterbrink GL and Liebenberg WH. Flowable resin composites as “filled adhesives”” Literature review and clinical recommendations. Quintessence International, Vol 30, No 4, 1999 35 Berry EA, Ward M. Bond strength of resin composite to air-abraded enamel. Quintessence Int. 1995;26:559–62 36 Deliperi S, Alleman DS. Stress-reducing protocol for Direct Composite Restorations in Minimally Invasive Cavity Preparations. Pract Proceed Aesthet Dent 2009;21(2):E1-E6 37 Buonocore M, J Dent Res 1955; 34: 849-53 38 De Munck J, Van Meerbeek B, Satoshi I, et al. Microtensile bond strengths of one and two-step self-etch adhesives to bur-cut enamel and dentin. Am J Dent 2003;16:414–420. 39 Van Meerbeek B, De Munck J, Yoshida Y,et al. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. 31 October 2011 14 Oper Dent 2003;28:215–235. 40 Immediate Dentin Sealing: A Fundamental Procedure for Indirect Bonded Restorations PASCAL MAGNE, J Esthet Restor Dent 17:144–155, 2005 41 Paul SJ, Schaerer P. Effect of provisional cements on the bond strength of various adhesive bonding systems on dentine. J Oral Rehabil 1997; 24:8–14. 42 Bertshinger C, Paul SJ, Luthy H, Schaerer P. Dual application of dentin bonding agents: its effect on the bond strength. Am J Dent 1996; 9:115–119. 43 Paul SJ, Schaerer P. The dual bonding technique: a modified method to improve adhesive luting procedures. Int J Periodontics Restorative Dent 1997; 17:536–545. 44 McCabe JF, Rusby S. Dentine bonding—the effect of pre-curing the bonding resin. Br Dent J 1994; 176:333–336. 45 Frankenberger R, Sindel J, Kramer N, Petschelt A. Dentin bond strength and marginal adaptation: direct composite resins vs ceramic inlays. Oper Dent 1999; 24:147–155. 31 October 2011 15 46 Ozturk N, Aykent F. Dentin bond strengths of two ceramic inlay systems after cementation with three different techniques and one bonding system. J Prosthet Dent 2003; 89:275–281. 47 Jayasooriya PR, Pereira PN, Nikaido T,Tagami J. Efficacy of a resin coating on bond strengths of resin cement to dentin. J Esthet Restor Dent 2003; 15:105–113. 48 Jayasooriya PR, Pereira PN, Nikaido T, Burrow MF, Tagami J. The effect of a“resin coating” on the interfacial adaptation of composite inlays. Oper Dent 2003;28:28–35. 49 Reis A, Rocha de Oliveira Carrilho M,Schroeder M, Tancredo LL, Dourado Loguercio A. The influence of storage time and cutting speed on microtensile bond strength. J Adhes Dent 2004; 6:7–11. 50 Dietschi D, Monasevic M, Krejci I, DavidsonC. Marginal and internal adaptation of Class II restorations after immediate or delayed composite placement. J Dent 2002; 30:259–269. 51 Cagidiaco MC, Ferrari M, Garberoglio R,Davidson CL. Dentin contamination protection after mechanical preparation for 31 October 2011 16 veneering. Am J Dent 1996; 9:57–60. 52 20 Years of GUIDED BONE REGENERATION in Implant Dentistry 2nd edition Daniel Buser 53 J Periodontol. 2000 Feb;71(2):299-307. Gingival recession treatment: guided tissue regeneration with bioabsorbable membrane versus connective tissue graft. Tatakis DN, Trombelli L. 54 Induction of Dentin Formation on Canine Amputated Pulp by Recombinant Human Bone Morphogenetic Proteins (BMP)-2 and -4 M. Nakashima JDR September 1994 vol. 73 no. 9 1515-1522 55 Arch Oral Biol. 1996 Jan;41(1):121-26. Induction of cementogenesis by recombinant human osteogenic protein-1 (hop-1/bmp-7) in the baboon (Papio ursinus). Ripamonti U, Heliotis M, Rueger DC, Sampath TK. 56 Tissue Eng Part B Rev. 2008 Sep;14(3):249-58. The biology of platelet-rich plasma and its application in oral surgery: literature review. 31 October 2011 17 Nikolidakis D, Jansen JA 31 October 2011