SERTAC Hospital Removal of a Patient from a Backboard and
advertisement

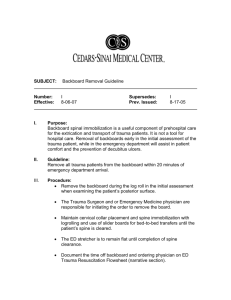
Hospital Removal of a Patient from a Backboard and Possibly Cervical Collar Removal Sample Guideline I. Purpose: To allow trauma patients to be expeditiously removed from backboards in a safe manner and to possibly remove cervical collars. Long backboards have never been shown to improve outcomesi,ii,iii and have been shown to cause respiratory compromiseiv,v, painvi,vii,viii,ix and skin breakdownx,xi,xii,xiii. The Emergency Department bed provides better spinal support than a long backboard or scoop stretcherxiv and is better for patientsxv,xvi,xvii,xviii. II. Guideline: Appropriately trained Emergency Department Staff may remove a patient from a backboard prior to physician evaluation. In addition, if certain criteria are met, the cervical collar may be removed and spinal precautions stopped. III. Procedure- Backboard Removal: a. Assess sensory and motor functions in all extremities prior to and after removal from a backboard. b. Using the 3-person logroll approach; logroll the patient with in-line stabilization of the head and neck. (Have a fourth person remove backboard.) c. Palpate and view the entire thoracic and lumbar spine. If bruising, swelling, deformity or tenderness is present, notify the physician and document the findings. Continue with backboard removal. d. Remove the backboard while the patient is on his/her side, and then logroll back to the supine position, maintaining c-spine precautions. e. If the patient does not have a cervical collar in place, either assess cervical spine for need of immobilization (next procedure) or immobilize the neck with a properly sized cervical collar or another neck immobilization technique. xix SERTAC Approved Sample Guideline 2/18/2014 Page 1 of 2 IV. Procedure- Cervical Spine Assessment and Possible Cervical Collar Removal: Patient may have their cervical collar removed (or not applied) and all spinal precautions stopped if ALL of the following conditions apply: They are conscious, cooperative and able to communicate effectively with providerxx,xxi,xxii. There is no major mechanism for severe injuryxxi (i.e. No activation of hospital Trauma Alert/Code.) Have no history of new or temporary neurologic deficit such as numbness or weakness in an extremityxx,xxi,xxii. Have no evidence of intoxication or altered mental statusxx,xxi,xxii,xxiii. Have no evidence of a distracting injuryxix,xxi such as Fractures Major burns Crush injuries Severe or distracting pain Have no midline back or neck pain or tenderness upon palpationxx,xxi,xxii. If all the above criteria are met, open the cervical collar and have the patient move their neck 45° to either side of midline and if still no painxxi, cervical collar can be removed and no spinal precautions are indicated. i Hauswald M, Ong G, Tandberg D, Omar Z. Out-of-hospital spinal immobilization: its effect on neurologic injury. Acad Emerg Med. 1998; 5: 214-9. ii Haut E, Kalish B, Efron D, Halder A, Stevens K, Kieninger A, Cornwell E, Chang D. Spinal immobilization in penetrating trauma: more harm than good? J Trauma. 2010; 68(1): 115-20; discussion 120-1. iii Kwan I, Bunn F, Roberts I. Spinal immobilization for trauma patients. Cochrane Database of Systematic Reviews. 2009; 1: 1-15. iv Bauer D, Kowalski R. Effect of spinal immobilization devices on pulmonary function in the healthy, nonsmoking man. Ann Emerg Med. 1988; 17: 915-8. v Walsh M, Grant T, Mickey S. Lung function compromised by spinal immobilization. Correspondence. Ann Emerg Med. 1990; 19: 615-6. vi Barney RN, Cordell WH, Miller E. Pain associated with immobilization on rigid spine boards. Ann Emerg Med. 1989; 18: 918. vii Lerner EB, Billittier AJ, Moscati RM. The effects of neutral positioning with and without padding on spinal immobilization of healthy subjects. Prehosp Emerg Care. 1998; 2: 112-6. viii March J, Ausband S, Brown L. Changes in physical examination caused by use of spinal immobilization. Prehosp Emerg Care. 2002; 6: 4214. ix Leonard J, Mao J, Jaffe D. Potential adverse effects of spinal immobilization in children. Prehosp Emerge Care. 2003; 7: 175. x Linares HA, Mawson AR, Suarez E, Biundo JJ. Association between pressure sores and immobilization in the immediate post-injury period. Orthopedics. 1987; 10: 571-3. xi Sheerin F, de Frein R. The occipital and sacral pressures experienced by healthy volunteers under spinal immobilization: a trial of three surfaces. J Emerg Nurs. 2007; 33: 447-50. xii Cordell WH, Hollingsworth JC, Olinger ML, Stroman SJ, Nelson DR. Pain and tissue-interface pressure during spine-board immobilization. Ann Emerg Med. 1995; 26: 31-6. xiii Berg G, Nyberg S, Harrison P, Bauchmen J, Gurss E, Hennes E. Near-infrared spectroscopy measurement of sacral tissue oxygen saturation in healthy volunteers immobilized on rigid spine boards. Prehosp Emerg Care. 2010; 14: 419-24. xiv Hauswald M. A re-conceptualisation of acute spinal care. Emerg Med J. 2012; 00:1-4. xv Vickery D. The use of the spinal board after the pre-hospital phase of trauma management. Emerg Med J. 2001; 18:51-4. xvi Yeung JHH, Cheung NK, Graham CA, Rainer TH. Reduced time on the spinal board- effects of guidelines and education for emergency department staff. Injury. 2006; 37:53-6. xvii Swartz C. Clinical decisions: resuscitation considerations to prevent pressure ulcers in trauma patients. Int J Trauma Nurs 2000; 6: 16-8. xviii Ahn H, Singh J, Nathens A, MacDonald r, Travers A, Tallon J, Fehlings M, Yee A. Pre-hospital care management of a potential spinal cord injured patient: a systematic review of the literature and evidence-based guidelines. J of Neurotrauma. 2011; 28: 1341-61. xix http://newnurseblog.com/2010/11/17/logrolling-patients-with-spinal-precautions/ xx Hoffman JR et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med 2000; 343:94-99. xxi Stiell IG et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 2001; 286:1841-1848. xxii Burton JH et al. A Statewide, Prehospital Emergency Medical Service Selective Patient Spinal Immobilization. J Trauma 2006; 61: 161-167. xxiii Evaluation for evidence of intoxication: Ask "What medications did you take today? Have you had any alcohol? Have you had any recreational drugs?" Is there slurring of speech, dilated or constricted pupils, unsteady gait? Do they smell like alcohol or marijuana? SERTAC Approved Sample Guideline 2/18/2014 Page 2 of 2