Spinal Motion Restriction

Spinal Motion
Restriction
Modernizing Our Management of Injured Patients
A Valley Medical Directors Collaboration
Objectives
• Historical perspective
• Understand injury based on biomechanical principles
• Review current evidence
• Learn spinal motion restriction concept
Historical Perspective
• Clinical Suspicion = IMMOBILIZE
• Any Trauma Above Clavicles = IMMOBILIZE
• Not Sure = IMMOBILIZE
• Fear of Punishment = IMMOBILIZE
• Don ’ t Feel Like Checking = IMMOBILIZE
Historical Perspective
• How bad is it?
• > 50% of trauma patients with no complaint of back/neck pain get full spinal immobilization
• 13% get immobilized without being asked about pain
The Facts
• 1 million EMS patients per year with suspected cspine injury
• 2% have a fracture
• 1% develop neuro deficits
Why Do We Do It?
• To avoid further patient injury caused by us during movement and transport
• Focus is on stopping gross visible spinal movement
• Patient packaging stops movement
• No movement = spine, cord, and patient are safer, right???
Evidence Is Weak
• Large meta-analysis on spinal immobilization
•
“Effect on mortality, neurologic injury, spinal stability… uncertain.”
•
“possibility that immobilization may increase mortality and morbidity cannot be excluded ”
Evidence is Weak
What Really Matters?
• Visible movement is only one threat
•
•
•
•
•
•
•
•
What about…
Pulmonary function compromise
Risk of aspiration/airway compromise
Increased intracranial pressure
Delays in transport
Concealment of other injuries
Soft tissue ischemia/necrosis
Cost of unnecessary diagnostics
Column and Cord
• Movement
• Significant amount of force needed to break bone and tear ligament
• Subsequent movement by EMS is less than force required to cause damage
Column and Cord
• Movement
• Normal range of motion = non-destructive distortion
• Movement within normal range requires almost no energy
• Resistance to movement within normal range is essentially zero
• No such thing as “less than zero”
Column and Cord
• Movement
• Viscoelastic tissues of spine stiffen and spasm post-injury
• Swelling increases preload on intact ligaments
• Locked facets and bone-on-bone impingements functionally immobilize spine
• Normal patients “self-splint” to avoid pain
Column and Cord
• Post Injury Deterioration
• Tissue hypoxia (local/global)
• Direct contusion
• Biochemical cascade, cell death
Column and Cord
• Post Injury Deterioration
• Mitigated by getting to definitive care FAST
• EMS focus should be reducing delays
• Patient packing with full SI is a potential delay
Summary
• We immobilize way too many patients
• Most injured patients will be mechanically stable
• Totally unstable patients probably have maximum damage at time of impact
• All immobilized patients can be potentially harmed
Spinal Immobilization
• SI is a method of transport, not a therapy
• SI is a misnomer
• Just say “ no ” to the standing takedown
•
“ Spinal Motion Restriction ”
• Reduction of gross movement
• Prevention of duplicating damaging mechanism
Just To Be “ Safe ”
• SI harms patients
• Cannot justify an intervention known to do harm just for small possibility of benefit
• Simple risk/benefit decision
How Does SI Hurt?
• Cervical collars
• Proven to increase ICP
• Produce axial distracting force
• Transfer force to ends
• Obscure neck injuries
• Make airway management more difficult
How Does SI Hurt?
• Rigid long back boards
• Cause decubiti within 30 minutes
• Cause iatrogenic pain
• Cause 15-20% reduction in respiratory capacity
• Causes delays in transport
How Does SI Hurt?
• Penetrating trauma victims
• NNT = 1,032
• NNH = 66
How Does SI Hurt?
• “ Time Zero ” Myth
• Patient evaluation and treatment does not begin at the exact time of arrival to the ED
Now What?
• Allow EMS to selectively immobilize
• Allow EMS to use the least amount of package needed for safe transport
• Monitor outcomes
Empowering EMS
• Several studies show EMS capable of deciding
• Tools derived from NEXUS and CCR
Spinal Motion Restriction
Adult
SMR - Blunt
Adult
SMR - Penetrating
Peds
SMR - Blunt
Peds
SMR - Penetrating
What About the Equipment?
• Scoop stretchers same or superior than log roll and lift-and-slide techniques
• Kendrick devices, short boards?
• Self-extrication with collar may be better
What About the Equipment?
What About the Equipment?
• “ Back boards are like spatulas; at some point that burger has to be put on a bun… ”
• Back boards are an extrication tool, not a medical treatment.
Spinal Immobilization Algorithm:
Blunt Trauma
Altered level of consciousness (GCS less than 15)
Yes
IMMOBILIZE
Rapid transport
No
Spinal pain or tenderness?
or
Neurological deficit or complaint?
or
Anatomic deformity of spine?
Yes
IMMOBILIZE
Rapid transport
No
Concerning mechanism of injury?
(Cont ’ d)
69 Copyright © 2012 by Mosby, Inc., an affiliate of Elsevier Inc.
Spinal Immobilization Algorithm:
Blunt Trauma (Cont ’ d)
Concerning Mechanism of Injury
Yes
Presence of:
Evidence of alcohol/drugs or
Distracting injury or
Inability to communicate
Yes
IMMOBILIZE
Rapid transport
No
IMMOBILIZATION NOT
INDICATED
Transport
No
IMMOBILIZATION NOT
INDICATED
Transport
Copyright © 2012 by Mosby, Inc., an affiliate of Elsevier Inc. 71
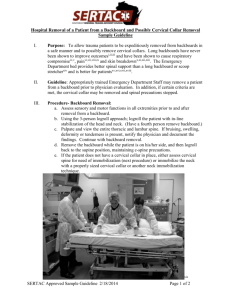
ED Transfer of Care
• Helpful to discuss with ED why you decided to package or not package patient
• Share your information and decision-making
• Patient packaging no longer a contextual clue to guide radiography needs
• ED providers will have to independently reexamine and decide if radiography indicated
Interfacility Transfers
• Medical directors need to reconsider protocols
• How is first hospital “ clearing?
”
• Crews should independently examine patients
• Implications of GCS < 15?
• Collar reasonable, but rigid long board???
• Other ways to “ puts handles on a patient ”
Thank You!
• Valley Medical Directors
• Jim Morrissey, Alameda County EMS
• Jerry Schirmer, Laura McElhatten, Mark Jones, Mesa
Fire/Medical EMS Division, Charlie Foster, Amy Gaber
• MFMD 204-A, CFD E286-C and R286-C
• SWA SW208
• SFD E601-A, P608
SMR Video
Spinal Motion
Restriction
Modernizing Our Management of Injured Patients
A Valley Medical Directors Collaboration