Client Referral Project
advertisement

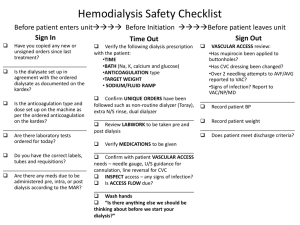
Client Referral Project a) Interns will meet with PD nurse and dialysis RN to learn about their jobs, including anemia management, bone mineral metabolism, kinetics/adequacy b) Interns will meet with social worker to learn about community resources available for renal patients c) Interns will meet with technicians to learn about the dialysis machine functions d) Interns will meet with reuse technician (not applicable as Fresenius uses one-time-use dialysate) Summary: I met with LuJuan Jakubek, PD and Home Therapies Nurse at Albany’s Fresenius Dialysis Clinic. LuJuan has been a renal nurse for over 8 years and has been with the Albany clinic for a little over 1 year. As a Home Therapies Nurse, she visits patients at their homes on an annual and an as-needed basis. During the annual visits, she must perform a home (site) inspection of the patient’s residence to ensure it is a safe environment that is free of simple hazards (i.e., untacked carpet that may facilitate falls), is organized (i.e., the patient has easy access to her/his dialysis supplies) and promotes a safe and healthy environment (i.e., relatively clean, not overrun by insects or rodents, has safety items like fire extinguishers and smoke detectors). The as-needed visits are determined by patient need and may occur at any time; often, they are due to technical difficulties with a dialysis machine, poor drainage from a (PD) catheter or a patient who has developed an infection (commonly peritonitis). A visit may last anywhere from 15 minutes to 1.5 hours. One important aspect of LuJuan’s job is helping patients with poor anemia profiles. People with end stage renal disease (ESRD) aren’t able to make erythropoietin (a hormone produced by the kidney that stimulates red blood cell production). Treatment for anemia often utilizes a pharmaceutical called Epogen (epoetin), a synthetic version of erythropoietin. LuJuan follows a protocol that allows her to adjust dosages of Epogen depending on a patient’s lab results as well as their historical response level to the drug. She may also adjust the amount of iron supplementation a patient receives, as iron is often given in conjunction with epoetin. Bone mineral metabolism often goes askew in ESRD patients and is known as secondary hyperparathyroidism. Because the kidney doesn’t function properly, phosphorus is retained (in the blood) instead of being eliminated via the urine. This increased level of serum phosphorus triggers the parathyroid (PTH) gland to work overtime. In response, the body tries to regulate the high phosphorus levels by increasing serum calcium. Hence, calcium is leached from the bones so that serum calcium may rise, but this puts bones at risk of becoming brittle and frail (osteoporotic). As if this weren’t enough, patients with ESRD often suffer from lower Vitamin D sensitivity; vitamin D helps the PTH become more sensitive to calcium so less may be removed from the bone. Thus, another helpful strategy is vitamin D supplementation (often with the pharmaceutical Zemplar; however, patients must maintain serum phosphorus, calcium and PTH levels within certain levels before Zemplar may be prescribed). It is also necessary to note that serum phosphorus is dependent on dietary phosphorus intake, so patients are also advised to keep their dietary intake of phosphorus low. While nutritional counseling is a task for the registered dietitian (RD), all dialysis staff members (including the PD nurse) work together to encourage patient compliance in decreasing phosphate from the diet. I also spoke with Nicki McClure, RN and Clinical Manager of the Albany Fresenius Dialysis Clinic. Adequacy of dialysis is primarily measured by overall fluid pull (if the patient is able to be dialyzed to their estimated dry weight (EDW), by their urea reduction ratio (URR) and by their KT/V (measurement that considers amount of urea present before and after dialysis, the length of time the patient is on dialysis and patient weight loss from dialysis). Goals are based on levels documented by research to have the most positive patient outcomes; for fluid, goal pull is usually 1-2% of body weight (with a max of no more than 5%), URR goal is > 65%, and KT/V goal is >1.4. The nurses and technicians monitor the patients during their treatment, keeping an eye on these values and the patient’s overall status (i.e., physical tolerance) to ensure proper dialysis and patient safety. Before the patient is hooked up to the machine, the nurses check the access line for signs of infection, clotting or clogging. The patient’s access is their lifeline to efficient and effective hemodialysis treatment. Megan Peters, Certified Clinical Hemodialysis Technician gave me a tour of the hemodialysis machine. This high-tech pump is attached to the patient’s access line (fistula, graft or catheter) via two tubes; one tube removes blood from the patient, the other returns blood once it has been dialyzed. Depending on the doctor’s order, fluid, filtering or both may be the indicated treatment. Once again it was reiterated that access lines are thoroughly checked before treatment begins and, every month, a procedure known as “twisters” are performed. This is when blood flow through the machine is reversed; that is, the tube that usually removes blood from the patient is used to return blood to the patient. This procedure offers another way to check the access line by measuring the [blood’s] pressure flow through the fistula or graft, and is useful in detecting small changes that may indicate if the fistula or graft is working less than optimally. I was unable to meet with the social worker due to a conflict of schedule, so I researched this role online. Social workers help patients by providing support to various challenges that pertain to their hemodialysis treatment, such as finances, career, emotions and adjustment to dialysis including lifestyle changes and emotional processes (such as confusion, grieving, anxiety and stress). The main responsibility of the social worker is to help patients and their families cope with kidney disease by teaching them about the disease process and the available treatment options. Often times, community resources are necessary to help the patient through this process (i.e., working with or referring patients to organizations to aid in obtaining insurance and other financial assistance, legal assistance, medical information, support groups, life-skills or social groups/classes, food assistance (such as SNAP or food banks), and/or spiritual needs). The social worker is a strong advocate for the patient, and, with proper communication, can help the patient find solutions to many of the complex needs commonly encountered with the diagnosis of kidney disease. By talking with the people who work directly with patients during treatment, I was able to better understand their scope of practice and where the RD fits into the picture. The RD is in charge of the nutritional component, but if a patient needs medical attention during treatment or if a machine buzzer sounds, the nursing staff needs to be informed so they may resolve the issue. Following proper procedures and remaining within the practitioner’s scope of practice is very necessary to ensure the patient receives safe, proper and complete care. Reference: DaVita. Social workers: helping patients at the dialysis center. Accessed June 10, 2013 at http://www.davita.com/treatment-options/hemodialysis/in-center-hemodialysis/social-workers:helping-patients-at-the-dialysis-center/t/5598