care planning - (S&I) Framework
advertisement
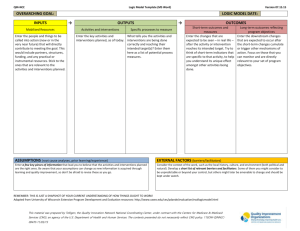
Introduction CMS requires and MU1 supports the exchange of a plan of care at the time of transfer from the hospital to the principle care physician at discharge. We have analyzed the current standards and compared them to what would be required to address the care planning needs of individuals with complex health issues. In this paper we propose a series of steps to bring the current standards for the electronic exchange of care plans into line with the requirements of a longitudinal plan of care. The complexity of a plan of care increases as the number of issues requiring management increases. Furthermore, because of the requirement for communication among providers of care, the complexity of managing a plan of care increases exponentially with the number of health care providers who are engaged with that individual. Both the number of active problems and the number of health care providers rise in parallel. As a result, there is an eight-fold increase in the complexity of managing the care of the individual with two problems and two providers compared with an individual with one issue and one provider. 5% of Medicare beneficiaries account for 70% of the care paid for by Medicare. In general, they have more than three active health issues; five different clinicians involved in their care and take more than 10 medications. The complexity of managing their care is 100-fold greater than managing the care of the individual with one problem. Currently, when the care of such individuals is managed, one health care professional assumes responsibility for coordinating care, improving communication among providers and clarification of the individual’s goals of care. Often, however, even intensive management processes are not sufficient to avoid interventions that are conflicting, duplicative and potentially harmful. Every clinician can provide examples of meticulously crafted care plans that fail. There are hundreds of ways in which these plans can fail, but most fail because of inadequate communication among providers and failure to clarify the individual’s goals of care. Current health information exchange standards have gaps and cannot fully support the range of information required to create, amend and disseminate a complex plan of care. Fortunately, some of the required components for care plans are in place. In the following sections we offer preliminary suggestions for the components and functional requirements needed for care plans that we believe are needed to support service delivery to medically complex and functionally impaired persons. We also submit our preliminary analysis of the extent to which standards are available to support these requirements. propose a model for longitudinal coordination of care, identify the categories of information required to support this model, discuss gaps in the current information exchange standards and propose a series of steps to remedy those gaps and provide the foundation for HIE assisted longitudinal coordination of care. The following diagram highlights the keys components of the care planning process that will be described in the balance of this paper. Care Planning has been an integral component of the practice of nursing since ….. The lack of a single standard nomenclature for clninical processes in nursing has long been identified as a barrier to effective communication. The Nursing Information and Data Set Evaluation Center (NIDSEC) of the American Nurses Association (ANA) recognizes ten standardized vocabularies that support the documentation of nursing care and care planning. (http://www.nursingworld.org/MainMenuCategories/ThePracticeofProfessionalNursing/HealthIT/StandardizedNursingLanguage.html#McCloskeyDochterman) “Lillibridge55 found that when nurses were asked to list the type of data they would normally collect using specific examination techniques, 23 percent provided nursing assessment details. It can be argued that if nurses were provided with an explicit nursing framework (and language) to document and communicate about their care that nurses and the interdisciplinary team members would more readily understand the importance and impact of nursing care and patient outcomes. Others have also found that the care plans typically do not reflect actual nursing practice.56, 57” http://www.ahrq.gov/qual/nurseshdbk/docs/KeenanG_DNCPP.pdf This disconnect between care plans and nursing practice is of uncertain clinical significance. Given that care plans do not typically inform care withn a clinical organization, it seems clear that the sharing of care plans across organizations during a transition is even more uncommon. Additionally, clinical summary data coming from an organization where care planning and coordination is not well integrated into clinical process is likely to underrepresent the sender plan of care to the receiver. Measures of effective transitions of care are not well developed, however, nearly all interventions attempting to improve transitions from Hospital to LTPAC measure the thirty day readmission rate. To date, there has been an intense investment at informing transitions with clinical summary data through standardization of data, document architecture, data exchange and system adoption. Implied in this strategy is that at the receiver site, this clinical data would be inputted into a care planning process to improve start of care, reducing gaps in service created by the lack of a transmitted care plan. However, given the current state of the practice of nursing described in the AHRQ report, it is likely that the clinical summary data will not require sufficient information to effectively create a new care plan at the receiving site. Although the nomenclature of clinical nursing and care planning has not achieved professional adoption of a single standard, the three major vocabularies most widely adopted (NANDA Classification,NIC,and NOC) each identify three common elements to a care plan: Problems, Outcomes and Interventions. These concepts, however, are not harmonized with the similar concept in the practice of medicine (Assessment and Plan). Many of the terms in the care planning process are used ambiguously. For example, Goals and Outcomes are often used interchangeably, however, it is clear that a person could achieve numerous desired outcomes from interventions without achieving their overall health goals. In the domain of Interventions, the concept of treatments, orders, and services are used imprecisely. Most effective interventions contain elements of all three. Care Plan problems are not synonymous with the concept of Problems as structured for inclusion in the consolidated CDA. Care plan models vary. Some are described as “strength based” and others are “deficit based”. While interventions to support retained capacity or a healthy lifestyle are well recognized, most interventions in care plans are directed at correcting or compensating for a functional deficit or symptom resulting from an illness, injury or accident or for preventing an adverse outcome from an identified risk factor or factors. The S and I Framework endorses the concept of Health Concerns to inform the care plan process. In turn, Health Concerns are informed by a number of sources, including the Problem template, multidisciplinary assessment findings including risk assessments, patient reported concerns and evidence based practice guidelines. Orders is of particular concern. As its name implies, orders are intended to provide instructions from an authorized entity based on scope of practice to a non-authorized entity. This non-authorized entity now becomes responsible for outcomes. HITECH and other investments in technology have now created standards for Order Entry Systems, however, the standards for nomenclature and structure of Order messages is only defined for a small subset of orders including diagnostic testing (Clinical Laboratory and Diagnostic Imaging) and Prescriptions. The care plan concept of Interventions is much broader and requires significantly more granular information.It is essential to recognize that care planning is a process outputs care plans. The inputs are clinical observations and judgments by multiple disciplines which were are not optimized for sharing across disciplines. Some of the input data was not intended for inclusion in the care plan. For example, a Medication list is usually the compiled list of Medication prescriptions, typlically sorted by Active (no stop date) or Inactive (with stop date). Medication information required to inform a care plan requires administration instructions, special precautions, potential side effects, duplicate therapy, and patient education requirements which are applied during the care planning process. During the care planning process, associations are made between Health Concerns, Interventions and Desired Outcomes to create a molecule of information supporting an Intervention. The inputs are transformed by the process and fused into a single concept to create the plan. To enable the creation of a care plan through technology, standards must be enhanced to include the core elements in an unambiguous way. Health Concerns should be informed by every potential contributor to the process. The component elements of Interventions beyond the elements defined for CPOE need to be structured and coded. Goals and Desired outcomes require more granularity. The care plan elements become molecules in a “many to one to many” fashion (see figure bill to do if desired). In order to inform care delivery and future assessments, these care plan molecules must then be interpreted by the systems supporting clinical assessments. Given the lack of alignment of the information streams and the ambiguity of terminology to inform the care plan, the lack of alignment between care plans and the clinical processes within health care organizations, the lack of standardized architecture of the care plan and the lack of standards to support the functional requirements for the care plan molecules, the exchange of care plans remains an elusive goal. Add summary – of our “punch line” and table showing summary of what is in rules/Components needed 1 Background The Health IT Policy Committee (HITPC) recommended that providers incented under Meaningful Use (MU) record care plan information for transitions of care and team member information for their patients.1 Proposed rules from CMS (MU Stage 2 NPRM) and the ONC (Standards and Certification NPRM) addressed these HITPC recommendations by expanding requirements for the summary care record to incorporate care plan and team member data elements. The Standards & Interoperability Framework (S&I) Longitudinal Coordination of Care Workgroup (LCC WG) applauds these efforts to move care plan content into interoperable health information exchange. Care plans have long served a critical role in cataloguing patient needs and managing patient care in a wide array of settings, including long-term and post-acute care (LTPAC). Persons with multiple chronic illnesses (CIs) and functional impairments receive health and related services from a multitude of individual and organizational providers, during single episodes of care and over time, and account for significant health care expenditures. Timely and complete health information exchange (HIE) is expected to (i) improve quality and continuity of care, and (ii) avoid unnecessary and costly hospitalizations and medical errors. 1.1 Care Plan Activities of S&I LCC WG The S&I LCC WG is keenly interested in care plans and has activities focused on near-term, pragmatic workflow solutions for the Home Health Plan of Care (HH POC) and long-term strategic visions for longitudinal, coordinated care. 1 Department of Health & Human Services, Centers for Medicare and Medicaid Services. (2012). Medicare and Medicaid Programs NPRM; Electronic Health Record Incentive Program—Stage 2. Page 13722. Home Health Plan of Care - The HH POC is a process of care initiation and coordination between Home Health Agencies and clinical professionals that provides certification of need, medical oversight (e.g. physicians) and care management. The S&I LCC WG is engaged in the identification/creation of standards for the iterative exchange of HH POC data elements and the contextual information required to authorize or update a care and service plan. Support of this process introduces an element of care coordination over time to the technical standards. Longitudinal Care Plan - Care planning over time and across multiple settings and disciplines has long challenged the health care community. The S&I LCC WG is engaged in the identification of the: , , Components/domains and other functional requirements needed for development of care plans that fully engage patients, families and care providers; Interdependencies of these requirements in the identification of goals and specification of outcome measures, and The health IT standards that are needed to support the interoperable exchange of care plans. . 1.2 Care Plans and the CMS/ONC NPRMs Based on considerations to date, the S&I LCC WG believes that clearer and more complete specification of the functional requirements for care plans and their exchange standards is needed to support the interoperable exchange of care plans and the MU of care plan content in EHRs. The considerations by and recommendations of the S&I LCC WG are presented below. The HITPC, CMS and ONC may find these remarks helpful as they consider care plan requirements for the EHR MU Program. 2 Care Plans: Recommendations From HITPC and Proposed Requirements from CMS and ONC The following table summarizes the recommendations and proposed requirements related to care plans provided by the HITPC, CMS and ONC. Recommendations from HITPC Care Plan Record care plan fields, including goals and instructions, for at least 10 percent of transitions of care CMS Proposed Rules Preamble pgs 13716 and 13722: The content of the care plan is dependent on the clinical context. We propose to describe a care plan as the structure used to define the management actions for the various conditions, problems, or issues. For purposes of meaningful use measurement, we propose that a care plan must include at a minimum the following components: Problem (the ONC Proposed Rules § 170.314(b)(1) (Transitions of care - incorporate summary care record.) . . . Electronically incorporate, at a minimum . . . care plan, including goals and instructions; § 170.314(b)(2) (Transitions of care—create and transmit summary care record.) . . . Electronically create a summary care record formatted according to the standard adopted at § Proposed Standards Create Summary Care Record § 170.205(a)(3) (Consolidated CDA) Transmit Summary Care Record § 170.202(a)(1) (Applicability Statement for Secure Health Transport); § 170.202(a)(2) (XDR and XDM for Direct Messaging); § 170.202(a)(3) (SOAP–Based Secure Transport RTM version 1.0) Recommendations from HITPC CMS Proposed Rules focus of the care plan), goal (the target outcome) and any instructions that the provider has given to the patient. A goal is a defined target or measure to be achieved in the process of patient care (an expected outcome). ONC Proposed Rules Proposed Standards 170.205(a)(3) and that includes, at a minimum . . . care plan, including goals and instructions Preamble pg. 13716: We propose to require the following information to be part of the clinical summary for Stage 2: . . . Care plan field, including goals and instructions Preamble pg. 13720: Therefore, in order to meet this objective, the following information must be made available to patients electronically within 4 business days of the information being made available to the EP: . . . Care plan field, including goals and instructions Preamble pg. 13722: All summary of care documents used to meet this objective must include the following: . . . Care plan field, including goals and instructions Problem Preamble pgs. 13716 and 13722: For purposes of meaningful use measurement, we propose that a care plan must include at a minimum the following components: Problem (the focus of the care plan) Instructions Record care plan fields, including goals and instructions, for at least 10 percent of transitions of care Preamble pgs 13716 and 13722: . . . any instructions that the provider has given to the patient). Preamble pg. 13716: We propose to require the following information to be part of the clinical summary for Stage 2: § 170.314(b)(1) (Transitions of care - incorporate summary care record.) . . . Electronically incorporate, at a minimum . . . care plan, including goals and instructions; § 170.314(b)(2) (Transitions of care—create and transmit summary care record.) . . . Electronically create a Create Summary Care Record § 170.205(a)(3) (Consolidated CDA) Transmit Summary Care Record § 170.202(a)(1) (Applicability Statement for Secure Health Transport); § 170.202(a)(2) (XDR and XDM for Direct Messaging); § 170.202(a)(3) (SOAP–Based Secure Transport RTM version Recommendations from HITPC CMS Proposed Rules . . . Care plan field, including goals and instructions Preamble pg. 13720: Therefore, in order to meet this objective, the following information must be made available to patients electronically within 4 business days of the information being made available to the EP: . . . Care plan field, including goals and instructions ONC Proposed Rules summary care record formatted according to the standard adopted at § 170.205(a)(3) and that includes, at a minimum . . . care plan, including goals and instructions Proposed Standards 1.0) Preamble pg. 13722: All summary of care documents used to meet this objective must include the following: . . . Care plan field, including goals and instructions Goals/Outcomes Record care plan fields, including goals and instructions, for at least 10 percent of transitions of care2 Preamble pgs 13716 and 13722: . . . goal (the target outcome) and any instructions that the provider has given to the patient. A goal is a defined target or measure to be achieved in the process of patient care (an expected outcome). Preamble pg. 13716: We propose to require the following information to be part of the clinical summary for Stage 2: . . . Care plan field, including goals and instructions Preamble pg. 13720: Therefore, in order to meet this objective, the following information must be made available to patients electronically within 4 business days of the information being made available to the EP: . . . Care plan field, including goals and instructions Preamble pg. 13722: All summary of care documents § 170.314(b)(1) (Transitions of care - incorporate summary care record.) . . . Electronically incorporate, at a minimum . . . care plan, including goals and instructions; § 170.314(b)(2) (Transitions of care—create and transmit summary care record.) . . . Electronically create a summary care record formatted according to the standard adopted at § 170.205(a)(3) and that includes, at a minimum . . . care plan, including goals and instructions Create Summary Care Record § 170.205(a)(3) (Consolidated CDA) Transmit Summary Care Record § 170.202(a)(1) (Applicability Statement for Secure Health Transport); § 170.202(a)(2) (XDR and XDM for Direct Messaging); § 170.202(a)(3) (SOAP–Based Secure Transport RTM version 1.0) Recommendations from HITPC CMS Proposed Rules ONC Proposed Rules Proposed Standards used to meet this objective must include the following: . . . Care plan field, including goals and instructions Team Member Record team member, including primary care practitioner, for at least 10 percent of patients Preamble: All summary of care documents used to meet this objective must include the following: . . . Any additional known care team members beyond the referring or transitioning provider and the receiving provider. § 170.314(b)(1) (Transitions of care - incorporate summary care record.) . . . Electronically incorporate, at a minimum . . . names and contact information of any additional care team members beyond the referring or transitioning provider and the receiving provider; § 170.314(b)(2) (Transitions of care—create and transmit summary care record.) . . . Electronically create a summary care record formatted according to the standard adopted at § 170.205(a)(3) and that includes, at a minimum . . . names and contact information of any additional care team members beyond the referring or transitioning provider and the receiving provider Create Summary Care Record § 170.205(a)(3) (Consolidated CDA) Transmit Summary Care Record § 170.202(a)(1) (Applicability Statement for Secure Health Transport); § 170.202(a)(2) (XDR and XDM for Direct Messaging); § 170.202(a)(3) (SOAP–Based Secure Transport RTM version 1.0) Table 1: Recommendations from HITPC and Proposed Requirements from CMS and ONC 2.1 CMS/ONC Proposed Care Plan Requirements: S&I LCC WG Comments As described below, the S&I LCC WG believes that: 1. While the CMS and ONC proposed rules begin to advance the interoperable exchange of care plan components at transition of care: a. All care plan components identified for information exchange need to be clearly defined. The rules do not define the following concepts: i. The components of a care plan ii. Problems iii. Instructions iv. Care team member b. Some identified care plan components need to be refined such as: i. “instructions” versus the broader concept of “interventions” ii. “team member” in the HIT PC calls out PCP and in the CMS rule describes “referring and receiving provider. However, there are many clinical disciplines that may serve as team members and could be involved in establishing and implementing a care plan c. d. Some key care plan components are not included (i.e. “interventions”) e. Proposed care plan requirements (i.e. inclusion of care plan, goals and instructions in a summary of care record at transitions of care) are insufficient to support the robust care planning process necessary for care planning across multiple providers and clinical disciplines and over time. . 2. While the S&I LCC WG and a broader team of members from the S&I Transitions of Care WG, HL7 Structured Documents WG and HL7 Patient Care WG, support the use of the HL7 Consolidated CDA standard, as described below further analysis is needed to assess: a. Whether/how the Consolidated CDA can support, or be modified to support, the requirements for interoperable exchange of the care plan and re-use of the care plan. b. [is there something else from the Doug memo that is needed here?] 2.1.1 Recommended Care Plan Components, Terms & Definitions Based on (i) discussions among the S&I POC HIT Squad; and (ii) an informal review of the literature for terms related to care plan [see Appendix ___], the S&I LCC WG believes the following components are needed to support the creation of care plans that will promote the timely initiation of care and service delivery to patients, particularly as these individuals transition across care settings and experience “shared care” with multiple care providers and clinicians. Care Plan Term/ Component Discussion General Definition of “Care Plan” Care Plan Proposed Component/Definition (footnote if appropriate) Next Steps From Susan’s Spreadsheet: A document that identifies the patient's needs and the ways of meeting them. A care plan is a dynamic document initiated at admission and subject to continuous reassessment and change. Typically a care plan includes: diagnoses (medical, nursing, etc.), orders, interventions, and outcomes. Care plans can be written for an individual patient, or be pre-printed or retrieved from a computer and then individualized. Care Plan “Problem” versus “Health Concern” Problem Health Concern The POC HIT Squad believe that care plans need to capture and address the broad array of “health concerns” such as: Acute and Chronic Medical Problems Concerns such as injury, illness, disease progression Risk factors such as age, family history, exposures/ lifestyles, environment, treatment side effects Care Plan “Decision Modifiers” Decision Modifiers From Bill’s spreadsheet: Superset of conditions and problems Note: The concept of “Health Concern” was explored by the HL7 Patient Care Committee. http://wiki.hl7.org/index.php?title=Health_Co ncern ? Care Plan Term/ Component Discussion Proposed Component/Definition (footnote if appropriate) Next Steps Care Plan “Interventions” versus “Patient Instructions” Interventions From Bill’s spreadsheet Superset of actions, instructions, and orders_______ Identify & evaluate candidate standards (e.g. Omaha, NIC, etc.) Instructions Care Plan “Goals” versus “Outcomes” Goals Outcome Team Member Team member Table 2: Definitions of Key Care Plan Terms and Components What is the relationship between table 2.1.1 and 2.1.2? 2.1.2 POC HIT Squad Analysis of Standards Needed to Support & Exchange Interoperable Care Plans Care Plan Component Care Plan Health Concern Decision Modifiers Other things… risk factors… Interventions Instructions Goals Outcome Team member Interoperable Exchange/ transmission of the Care Plan Consolidated CDA Analysis Comments No “care plan” document template. Care plan section level template. Not reflected in CCDA as a section [or data enty] level template. C-CDA reflects “problems.” However, [p/u language from Doug memo] Recommendations and Activities needed to assess the issue. Recommendation: Collaborate with HL7 SDWG and PC WG to modify the C-CDA to include a “Care Plan” document type. [will need to consider status of/impact on “care plan section level template.] Recommendation: 1. Collaborate with HL7 SDWG and PC WG to modify the C-CDA: a. to include “Health Concern” as a section-level/[data entry level] template that could be used for cares plans and other documents/sections in the CCDA. b. Describe the relationship between “Health Concern” and “problems” Table 3: Analysis of Standards Needed to Support & Exchange Interoperable Care Plans Care Plan Inputs Plan Concepts Governance Health Concerns Interventions Team Members Decision Modifiers Goals Outputs Care Plan Coordinator Roles and Responsibiliies Care Plan Process Standards Patient Instructions Symptoms (patient reported data) Monitoring and Expectancy Assessment findings Diagnostic and Prognostic Testing Medications International Classification of Functioning, Health and Disability Nursing Diagnoses (N3) Medical Problem List Treatment Plan Plan of Care Procedures Skilled Nursing and Rehabilitation Consultation Other Care Plan Standardized Roles Scope of Practice Standardized Instructions Interoperable Care Plan Patient Choice Prognosis Global Goals Advance Care Documents and Orders Desired Outcome Intervention Functional Status Clinical Practice Guildelines Physiologic Reserve Milestones Access to Care Duration Affordability Related Interventions Risks Adverse Event History Related Conditions 3 Care Plan Activities of S&I LCC WG 3.1 Home Health Plan of Care Use Case The S&I LCC WG, via work undertake by it’s Longitudinal Care Plan Sub-Workgroup (LCC LCP SWG), has focused efforts on identifying requirements to support the interoperable exchange of the initial care plan between the Home Health Agency (HHA) and the attending physicians. This use case focuses on a required component of the HHA workflow because…. In addition, care plan supports more comprehensive and on-going care planning and assessment of the patient. [once the care plan signed by the attending physician, the HHA may submit a claim for and payment from Medicare for covered services provided to Medicare beneficiaries.] Insert diagram of HHA care planning process The S&I LCP WG HHA care plan work focuses on the care plan requirements previously required by CMS [and extended/modified by VNS?]. In the past CMS required HHAs complete and obtain a physician signature authorizing the HHA PoC (formerly known as the CMS 485 form). The HHA care plan components that will be evaluated by SI are: [list] 3.2 S&I LCC WG Considerations for Longitudinal Care Plan BILL The Longitudinal Care Plan subworkgroup charter was to document the gaps to technology enabled of sharing care plans between health care entities. One major assumption was that there were common elements of a care plan process and model which could be extended across these entities. An ongoing environmental scan of care planning models revealed the following common clinical concepts: Problems, Interventions and Goals. Terminology and hierarchy of the concepts in the care plans was variable, however. It became immediately apparent that gaps not only impacted the ability to share care plans between organization, but more importantly, there was extensive mal-alignment of the care plan with clinical information streams and documentation systems and therefore the care delivery process itself was not well supported by current technology and standards. The subworkgroup has documented the inputs and outputs involved with the act of "care planning" which results in artifact(s) of the care plan. A list of high level functional requirements (data objects and data elements) for the care plan are defined. This list extends concepts previously identified requirements by S&I and HL7 Care plan concepts contained in MU stage 2 are being evaluated in the context of these functional requirements. In addition, critical components of a Care Plan not yet represented in the proposed rules are being identified. These gaps in information streams, semantics and care plan document architecture and the functional requirements will then be used to evaluate the current Consolidated CDA documents and data templates for their adequacy to communicate a complete care plan. 4 Next Steps 1. Validate LCC WG/ToC/Hl7 recommended functional requirements and standards assessment for I/O exchange of care plan, including extend care plan considerations to persons who are transitioned to and receive services in other LTPAC settings (e.g., IRFs, LTCHs, etc.) and receive LTSS. 2. Further assess the need for LCP as a matter of public policy and/or service delivery to patients, particularly those who suffer from multiple chronic illnesses, are medically complex, and have functional impairments. 3. If needed: a. validate and refine the LCC WG assessment of the components/functional requirements of a longitudinal care plan, b. identify the availability of and gaps in standards to support the I/O exchange of the LCP and the management and re-use of this document, and c. identify additional activities that are needed to advance this concept. 4. Identify vocabulary standards The activities described above will be undertaken, in part, by: 1. Extending the S&I LCC activities… 2. Convening a 2nd ONC roundtable to help validate assessments to date and need for and concepts in these “longitudinal Care Plan” 3. Publishing an RFI to solicit comments on functional requirements (and standards) needed for the I/O exchange of the longitudinal care plan.