Decreasing Patient Anxiety, Improving Access, and Decreasing
advertisement

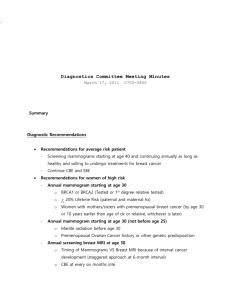
TITLE OF PROPOSED STUDY: Decreasing patient anxiety, improving access and decreasing disparities related to screening mammography and breast cancer diagnosis to include women of low socioeconomic class and lower educational levels. 1. Specific Aims: State the specific aims of this study. We will answer this research question:What is the impact of a new same day screen to diagnosis (SDSD) to include navigation services on anxiety, economic burden and patient safety compared to standard multiple day screen to diagnosis (MDSD) service? Specific Aim 1: Implement a SDSD service for women with abnormal screening mammograms. Specific Aim 2: Conduct a 2-group randomized control study to assess anxiety, economic burden and patient safety among participants. Specific Aim 3: Measure patient acceptance and sustainability of the new SDSD service compared to MDSD service . 2. Condition Burden and Impact: Briefly state the importance of the condition or problem in terms of prevalence and/or impact. Despite notable progress in the overall health of Americans in general, health disparities persist, with poorer outcomes experienced by vulnerable populations including racial and ethnic minorities, the poor and those with low educational attainment.(1) Approximately 1 in 8 women in the US will develop invasive breast cancer during their lifetime.(2) Delays in breast cancer diagnosis may lead to stage progression, treatment complications and cause poor clinical outcomes.(3) Timely access to diagnostic procedures allows women with breast cancer to avoid treatment delays. Studies have shown that minority women who face socioeconomic and other access-to-care barriers are less likely to survive breast cancer than other women.(4,5) Our own studies have found that Hispanic and other minority women experience disparities in timely diagnosis and treatment.(6-8) Low-income women face the challenge of understanding their diagnosis and navigating the complex structural barriers inherent in the U.S. health care system, all while dealing with the emotional and physical aspects of their disease.(6-9) Additional barriers to care include competing health, family, and work responsibilities, lack of transportation and child care, high cost and lack of insurance..(6-8).Language barriers, culturally specific health beliefs and a system which is both temporally and spatially fragmented frustrate and discourage patients. Patients may choose to discontinue the breast care they need. Although the majority of women lost to follow-up after an abnormal mammogram will eventually return to the system, they will most likely present with a more advanced stage of the disease. During the entire process, anxiety accelerates. (6-8) 3. Gap Analysis: Add a statement describing the evidence gap; be sure to include references, such as systematic review(s), guidelines, and other evidence. Implicit in the notion of patient centered care is responsiveness to patient needs, preferences and values. (5) Health care resources should be aligned according to the needs of the patient, including addressing barriers to cancer screening, timely diagnosis and treatment, and ensuring informed patient decision-making. Currently health care resources are poorly aligned with the needs of patients, particularly those who are poor or members of minority groups. (5, 10) Currently, breast cancer screening and diagnostic evaluations are performed in a similar manner across the United States, with women receiving a screening mammogram on a one day, the needed diagnostic evaluation at another visit and the biopsy at still a later date. (15-18) Biopsy results are usually conveyed within a week, by phone or by the referring provider. The process lingers for 20-25 days, often with a different provider at each step, generating high levels of anxiety (17). Low income and medically underserved women are more likely to experience longer delays and being lost to follow-up. With the advent of digital techniques, it is possible to provide same day screen to preliminary biopsy results (SDSD) for women with abnormal screening mammograms. A recent pilot quality process improvement project PRINCIPAL INVESTIGATOR (LAST, FIRST, MIDDLE): performed in our clinics demonstrates that this service is feasible. To overcome resistance to the new process, we must disseminate scientific information which proves that SDSD improves patient outcomes and is sustainable. 4. Study Design: Please provide a concise description of the study design including theoretical or conceptual framework and how it informs the design and variables being tested. Indicate whether the main (CER) question under study is to be addressed as a randomized trial (individual level or cluster), observational study (retrospective, prospective), quasi-experimental study, or other (please specify). We propose a 2 group randomized control study comparing the impact of SDSD versus MDSD (current standard) on patients’ anxiety, economic burden and safety. At service completion, both groups will receive an anxiety measurement assessment and a customer service/economic burden survey. We will also assess patient acceptance of the new service and process sustainability. We hypothesize that the intervention group will experience less anxiety and economic burden with fewer patients lost to follow-up and the process can be sustained. 5. Description of Participants and Participating Study Site(s): ): Describe the relevant demographic characteristics of the participants who are the target of the intervention, including how well they represent the target population, source of participants, and inclusion and exclusion criteria. Where the unit of randomization is a study site, rather than the participant, please describe representativeness of proposed participating sites. Our study population includes women with multiple disparities. ___% are 300% or more below the poverty level, ____ % are not English speaking. Patients under 21, incarcerated patients, patients who cannot consent themselves and pregnant patients will be excluded. Two sites will be used for the study: Cancer Therapy and Research Center and the Robert B. Green campus. The two sites combined perform about 19,000 screening mammograms, 10,500 diagnostic breast evaluations and 600 biopsies per year, diagnosing approximately 170 new cancers. 6. Outcomes: Describe the study outcomes, the key constructs to be measured, the validated measures to assess key constructs, and why the outcomes are important to patients, relevant to health systems and capable of changing practice. The outcomes of interest include: Patient’s Anxiety: measured using the anxiety subscale of the Hospital Anxiety and Depression Scale-HADS.11 The HADS is one of the most widely used measure of anxiety and depression in physical illness and has been extensively validated for cancer populations(12-14); Economic burden: measured by a survey of lost wages, time away from work, child care cost and parking/transportation cost; Patient safety (lost to follow-up): measured by reviewing medical records and missed appointments through the Radiology Information System; Patient acceptance: measured by patient satisfaction surveys Sustainability: measured by improved treatment outcomes due to a change in diagnostic practice. 7. Power Calculations: State the power of the proposed study to detect the hypothesized effect, including support for all assumptions, (e.g., type-1 error level, standard deviation in outcome measure, underlying event rate). Note power for important subgroups, if applicable. Clearly state and support all assumptions. PCORI Spring 2015 Cycle: Letter of Intent Template 1 PRINCIPAL INVESTIGATOR (LAST, FIRST, MIDDLE): 8. Hypothesized Effect Size for Intervention on Main Patient-Centered Outcome: State the hypothesized effect size and cite references to support that the effect size is both realistic and clinically meaningful. Effect size is documented to be realistic, based on published evidence, and meaningful to patients. 9. Sample Size: Provide the total sample size for the main CER analysis and the number per arm (N1, 2, 3, 4 . . .), as applicable. As a general guide, <50 per arm may be considered underpowered, unless the condition is rare. N (total) N1 N2 N3 10. Comparators: List the interventions being compared. 1. Same day screen to diagnosis (SDSD) service 2. Multiple day screen to diagnosis (MDSD) service 11.Description of Comparators: Describe each intervention listed above under “Comparators,” including: a) Evidence of the efficacy or effectiveness of each or statements about its acceptance in widespread practice despite having limited evidence of efficacy or effectiveness b) An estimate of frequency of use in clinical practice c) If usual care is a comparator, justification of its inclusion and a proposal to clearly describe and document its components 1. SDSD is a process we piloted at our center to address the anxiety, economic burden and safety issues related to the patient. Pilot data suggests we have positive influence on all these issues. It is rarely used in practice. 2. MDSD is the standard of care in breast imaging and diagnostic centers with approximately 95-98% of centers providing this level of care. (15-18) 12. Engagement: Briefly state how patients and stakeholders are involved in all aspects of the research and list specific organizations involved. Sessions were held with patients, advocacy group members and key patient care providers to determine the key issues and burdens patients face when going thru the breast screening and diagnostic evaluation. We have input from the Susan G. Komen, San Antonio Affiliate, Alamo Breast Cancer Foundation, SLEW Wellness Center and the CTRC/UHS patient navigator. We will meet on a quarterly basis. 13. Duration of Study: State duration of intervention and length of follow-up as they fit in to a 3-year project or up to 5 years. The study will continue for 3 years. The first 2.5 years will be the accrual period. The last 6 months will be used for data analysis and submission for publication. 14. Cost of Study: State whether the study is small (up to $1.5 million in total direct costs for up to 3 years) or large (up to $5 million in total direct cost for up to 5 years). PCORI Spring 2015 Cycle: Letter of Intent Template 2 PRINCIPAL INVESTIGATOR (LAST, FIRST, MIDDLE): Small study size with Direct cost at $1,482,341.00 15. “Real-Life” Applicability of Strategies: : State how the intervention will be delivered and received in real-life clinical settings and will provide practical information that can help patients and other stakeholders make informed decisions about their health care and health outcomes. On alternate days, patients will be recruited into the study. Controls will receive care as per standard in the community and the study patients will have same day service. Our pilot project has shown this is feasible. We will analyze and publish the study results. We will share the information with patients and providers. NOTE: This LOI Template is for screening purposes only. If you are invited to submit an application, different criteria are required and will be reviewed. References: 1. Agency for Healthcare Research and Quality (2008) National Healthcare Disparities Report, 2007. Agency for Healthcare Research and Quality, Rockville, MD. 2. American Cancer Society. (2015). Breast Cancer. http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-key-statistics 3. McLaughlin JM, Anderson RT, Ferketich AK, Seiber EE, Balkrishnan R, Paskett ED. (2012). Effect on survival of longer intervals between confirmed diagnosis and treatment initiation among low-income women with breast cancer. Journal of Clinical Oncology 30, 4493-4500. http://www.ncbi.nlm.nih.gov/pubmed/23169521 4. Ooi SL, Martinez ME, & Li CI. (2011). Disparities in breast cancer characteristics and outcomes by race/ethnicity. Breast Cancer Research and Treatment 127, 729-738. http://www.ncbi.nlm.nih.gov/pubmed/21076864 5. Institute of Medicine. (2001). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press. 6. Ramirez, A. G., Pérez-Stable, E.J., Penedo, F.J., Talavera, G.A., Carrillo, E., Fernandez, M.E., Holden, A.E., Muñoz, E., San Miguel, S., & Gallion, K.J. (2013). Navigating Latinas with breast screen abnormalities to diagnosis: The Six Cities Study. Cancer. 119, (7), 1298-1305. 7. Ramirez, A. G., Pérez-Stable, E.J., Talavera, J.A., Penedo, F.J., Carrillo, E., Fernandez, M.E., Muñoz, E., Long Parma, D., Holden, A.E.C. San Miguel de Majors, S. Nápoles, A., Castañeda, S.F., & Gallion, K.J. (2013). Time to definitive diagnosis of breast cancer in Latina and non-Hispanic white women: the Six Cities Study. SpringerPlus, 2, (1), 84. Epub. 8. Ramirez, A. G., Pérez-Stable, E.J., Penedo, F.J., Talavera, G.A., Carrillo, E., Fernandez, M.E., Holden, A.E., Muñoz, E., San Miguel, S., & Gallion, K.J. (2014). Reducing time-to-treatment in underserved Latinas with breast cancer: the Six Cities Study. Cancer 120(5), 752-760. PCORI Spring 2015 Cycle: Letter of Intent Template 3 PRINCIPAL INVESTIGATOR (LAST, FIRST, MIDDLE): 9. Holden, A., Ramirez, A., & Gallion, K. (2013). Depressive Symptoms in Latina Breast Cancer Survivors: A Barrier to Cancer Screening. Health Psychology 33(3), 242-248. 10. Fiscella K, Humiston S, Hendren S, et al. Eliminating disparities in cancer screening and follow-up of abnormal results: what will it take? J Health Care Poor Underserved. 2011;22:83-100. 11. Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 67(6), 361–370. 12. Luckett, T., Butow, P. N., King, M. T., Oguchi, M., Heading, G., Hackl, N. A., et al. (2010). A review and recommendations for optimal outcome measures of anxiety, depression and general distress in studies evaluating psychosocial interventions for English-speaking adults with heterogeneous cancer diagnoses. Supportive Care in Cancer, 18(10), 1241–1262. 13. Norton, S., Cosco, T., Doyle, F., Done, J., & Sacker, A. (2013). The Hospital Anxiety and Depression Scale: A meta confirmatory factor analysis. Journal of Psychosomatic Research, 74(1), 74–81. 14. Vodermaier, A., & Millman, R. D. (2011). Accuracy of the Hospital Anxiety and Depression Scale as a screening tool in cancer patients: A systematic review and meta-analysis. Supportive Care in Cancer, 19(12), 1899–1908. 15. Raucher, GH, et al. (2014). Beyond the mammography standards act: measuring the quality of breast cancer screening programs. Am J. Roentgenol, 202(1), 145-51. 16. Rosenberg, Robert D, et al. (2011). Timeliness of Follow-up after Abnormal Screening Mammogram: Variability of Facilities. Radiology, 261(2), 404-413. 17. Wernli, Karen J., et al. (2015). Timing of follow-up after abnormal Screening and Diagnostic Mammograms. Am J Manag Care, 17(2), 162-67. 18. Kutner, Susan E. (2011). Today’s Work Today in Breast Care, Improving Access to Biopsy. Presentation, 5/14/2011, Honolulu, HI PCORI Spring 2015 Cycle: Letter of Intent Template 4