chemo drugs 2 (Sarah) - U
advertisement

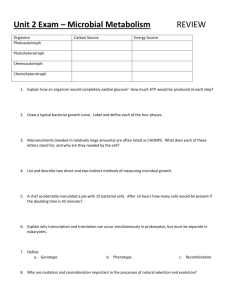
Class and Name MOA Clinical uses Adverse effects Antimetabolites Inhibition of DHFR leading to partial depletion of reduced folates Gestational carcinoma, hydatidiform mole, ALL (prevents meningeal leukemia & combo tx), br ca, epidermoid ca’s of head & neck, adv’d mycosis fungoides, lung ca (esp sq & sm cell), advance NHL N/V, photosensitivity, myelosuppression –IV (nadir 7 -10 d, recover by 14-20d) -renal : direct to renal tubular cells & intratubular precipitation of methotrexate and metabolites (high dose IV) -hepatic: ↑ed transaminase (oral, esp daily dose) -mucositis (3-7d): IV -CNS: (intrathecal, iv sometimes) 1. Acute chem. Arachnoiditis, arises imm after admin – severe HA, nuchal rigidity, vomiting, fever, and inflame cells in CSF 2. subacute: ~10%, usu 3-4th course, m common in those w/ active meningeal leukemia – motor paralysis, CN palsies, seizure, coma; cont’d intrathecal tx may ->death 3.chronic demyelinating encephalopathy: usu in kids mo-yrs after receiving intrathecal MTX -diarrhea diminish toxicity & counteract effects of impaired MTX elimination and of inadvertent overdosage of folic acid antagonists After high dose MTX tx in osteosarcoma & in adv’d colorectal ca Allergic sensitization, including anaphylactoid reactions and urticaria Met: liver Elim: urine(90%) & feces Inhibits dihydrofolate reductase and thymidine synthetase -solid tumors: malignant mesothelioma, breast, pancreatic, head & neck, non-sm cell lung, colon, gastric, cervical, bladder -myelosuppression (ANC nadir btwn 89.6 d w/ return to baseline 4.2-7.5 d later) -mucositis -GI toxicity Excreted 90% unchanged in urine 1. methotrexate (MTX) 2. Leukovorin (LV) 3. Premetrexed -admin folic acid & B12 Mechs of drug resistance & metabolism -defective transport common (ALL & osteosarcoma) -glutamic acid residue 45 -drug efflux pumps: multi resistant-asstd protein family (MRP -1,2,3, &4); 1 is primary route; overexp of efflux pump -↓ ability to form MTX polyglutamates Pyrimidine Antagonists 1. Azacitidine (5 –Aza) 2. Decitabine supplements 2 wks prior tx ca’s -skin rash/desquamatn(40%) -hepatotoxicity: reversible transaminasemia -anorexia -N/V (84%/58%) -infusion rxn: shivering Pyrimidine nucleoside analog of cydidine -hypomethylation of DNA & direct cytotoxicity on abn hematopoietic cells in BM MDS, CMML -direct incorporation into DNA and inhibition of DNA methyltransferase, causing hypomethylation of DNA and cellular differentiation or apoptosis MDS nonFDA: CMML Pro-drug of 5-FU; converted in tumor cell to 5-FU Met breast, met colon -as pass thru S phase, incorporates into cell & blocks polymerization of DNA by inhibiting DNA polymerase & leads to shortened DNA strands AML, ALL, CML, CNS leukemia, HD, NHL Myelosuppression (dose limiting toxicity), - IV: ↑ed serum Cr, reanl failure, renal tubular acidosis, hypokalemia, hepatic coma -subQ: N/V, pancytopenia, pyrexia, , diarrhea, fatigue, injection site erythema, constipation, ecchymosis Myelosuppression is dose limiting, fatigue, pyrexia, nausea, cough, petechiae, constipation, diarrhea, hyperglycemia -uncommon: A fib, cardiac arrest, HF, cerebreal hemorrhage, MI, intracranial hemorrhage, pneumonia, pulm edema Myelosup (lymphonenia in 94%); diarrhea, N/V, stomatitis, hand-foot syndrome (45%) – pain, redness, scaling of skin of palms/soles; faigue, anorexia, paraesthesia, HA, cardiotoxicity in 3% can be fatal – MI, angina, dysrythmias, arrest, failure, ECG changes Myelosuppression (14-21d), hepatic-jaundice and elevations in serum bilirubin, transaminases & alk phosphatase, alopecia, GI-diarrhea, anorexia, derm –marcopap rash, erythema, blistering/peeling of skin, esp on hands and feet), hand-ft syndrome 3. Capecitabine (oral 5-FU) 4. Cytarabine (Ara-C, Cytosine, Arabosinide, Arabinosylcytosin ) Met by liver and excreted in urine -> -High dose Ara-C toxicity: Cerebellar dysfxn (20%), usu w/in 2-8 days, accumulation of ara-U or ara-CTP causes nerve damage AND conjunctivitis/corneal toxicity (use steroid eye drops) 5. Flurorouracil (5-FU, 5fluorouracil) 6. Gemcitabine (difluorodeoxyCytidine, dFdC) Purine Antagonists 1. .Adenosine Analogs -general Analog of pyrimidine uracil -inhibits thymidylate synthase (TS) by FdUTP ->affects DNA synthesis Incorporation into cell DNA and RNA -incorporation into DNA strands, inhibiting replication and repair blocking nucleotide production -Inhibition of DNA repair & synthesis -Inhibition of RNA fxn -inhibiting synthesis of substrates needed for DNA synhthesis -cell-cycle specific for S phase Colorectal, gastric, pancreatic, breast, basal cell carcinoma nonFDA: liver, head & neck, ovarian, cervical -myelosuppression (7-14 d nadir w/ rapid recovery), possibility of febrile neutropenia - mucositis -diarrhea/nausea -skin: alopecia, maculopap rash of extremities -DPD deficiency: -> -cardiac: myocardial ischemia & rare, inherited disorder of angina in 2% pyrimidine degredation -CNS: somnolence & cerebellar d/t low/deficien DPD in ataxia in ~1% caucasion (~5%) and AA -ocular: conjunctivitis, lacrimation, (~.1%); pts; no evidence blepharitis, photophobia of fluorouracil -beware those w/ dihydrodegredation in these pts pryrimidine DH deficiency!- tx w/ 5--toxicities: diarrhea, FU can be life threatening for even stomatitis, partial deficiencies myelopsuppression, N/V, rectal bleeding, vol depletion, skin changes, neurologic! Met pancreatic, NSCLC Myelosuppression (anemia 68%, nonFDA: bladder, breast, leucopenia 62%, thrombocytopenia ovarian, malignant 24%) mesothelioma, NSCLC -N/V, Diarrhea, stomatitis, ↑es in serum transaminases, mild protein/hematuria ->can lead to irreversible renal failure (manifests as HUS), rash, fever/fluish sxs, dyspnea, peripheral edema Excreted in urine a. Fludarabine b. Cladribine a. 6-mercaptopurine (6-MP) -heme: myelosuppression (severe immunosuppression -> opp infections (OI’s) d/t ↓CD4’s -> herpes zoster, candida, PCP -CV: edema, chest pain, hypotension -fever (flu-like sxs in 25%) -derm: alopecia, rash Hariy cell leukemia, CLL, AML, NHL, Waldenstrom’s macroglobinemia Myelosuppression, CD4 & 8↓ 6 mo, OI’s, candida /aspergillosis (use px abx) -fever -rash -fatigue/HA -mild nausea Myelosuppression (esp T & B lymphocytes (esp CD4) – recovery prolonged & incomplete, fever & OI’s in 2nd and 3rd course) -dry skin, rash -fatigue, seizures -mild N/V -renal: tubular toxicity (↑ Sr CR) – use hydration Hairy cell leukemia, NHL, CLL, T-cell leukemia/lymphoma c. Pentostatin 2.Guanine Analogs (Thiopurines) CLL, low grade NHL, AML, Waldenstrom’s macroglobinemia, cutaneous T-cell lymphoma, BM transplant -inhibit de novo purine synthesis & purine interconversion rxns by falsely incorporating into RNA/DNA -cell specic for S phase Met in liver and excreted in urine -> CNS:peripheral neuropathy, blindness, coma, death -GI: diarrhea, N/V -pulm: pna, pulm hypersensitivity, interstitial pneumonitis -Results from decreased ability to form cytotoxic nuncleotide metabolites -resistant cells express either complete or partial deficiency of HGPRT (or altered affinity) ALL, CML, AML, NHL Pancytopenia -hepatic: jaundice, cholestasis, ascites, hepatic encephalopathy, ↑ liver enzymes -GI: N/V/D, abd pain -derm; necrosis, rash, HA ALL, AML, CML, NHL Myelosuppression (leucopenia, thrombocytopenia m com), ↑liver enzymes, VOD, jaundice, N/V/anrxa, stomatitis, severe diarrhea, rash/dermatitis, tumor lysis syndrome AML (blast crisis), sickle cell Myelosuppression, skin: rash, hyperpigmentation, pruritis, radiation recall b.6-thioguanine (6TG) Hydroxyurea S phase dep Enzyme that inhibits ribonucleotide reductase (nec for DNA synthesis) Microtubule Targeting Agents: 1. Vinca Alkyloids Naturally occurring nitrogenous base in periwinkle plant -inhibit microtubule assembly -rapidly/reversibly binds alternative sites on tubulin & disrupts microtubule fxn leading to metaphase arrest a. Vincristine 50% met in liver and 50% excreted unchanged in urine -Pleitropic or multidrug resistance (MDR) -> results in decreased drug accumulation & retention -alteration in α & β tubulins: leads to ↓ed drug binding or ↑ed resistance to microtubule disassembly ALL, HD, NHL, MM Testicular Ca, CLL, Aid’srelated Kaposi’s sarcoma, Ewing’s sarcoma, rhabdomyosarcoma, SCLC, medulloblastoma, cervical CA, CML -Neuro: peripheral neuropathy, parasthesia, ↓DTR’s, gait changes, pharyngeal/paratid pain (esp cristine/relbine) -adynamic ileus: mimics surgical abd -fatal ascending paralysis post intrathecal admin-> leads to resp failure/death b. Vinblastine Met testicular ca, bladder, prostate, HL, NHL, Kaposi’s sarcoma, breast ca, mycosis fungoides, choriocarcinoma, CML, cutaneous T-cell lymphoma, head & neck, lung, melanoma, neuroblastoma, ovarian c. Vinorelbine -GI: abd cramps, wt loss, N/V/D, oral ulcerations, paralytic ileus, int necrosis, anorexcia -mucositis, pharyngitis, stomatitis -constipation (esp vinorelbine) -heme: .vincristine: mild anemia, leucopenia, thrombocytp .vinblastine: myelosup. (esp neutropenia) .vinorelbine: neutropenia -derm: alopecia, photosentivity -CV: chest pain, htn, MI NSCLC, met br ca, hormone refractory prostate ca, cervical, ovarian 2. Taxanes a. Paclitaxel Promotes assembly of microtubules from tubulin diamers, and stabilizes microtubules by preventing depolymerization resulting in inhibition Abraxane: (alb bound paclitasel)-facilitates the admin of water insoluble contents Ovarian ca, br. Ca, NSCLC, Aids related Kaposi’s sarcoma, bladder, head & neck -hypersensitivity rxn (HSR) -neutropenia -derm: alopecia -onycholyosis, hand-ft/palm-plantar dysesthesia syndrome, urticaria, alopecia -fluid retention (↑ed cap permeability allows leakage of fluid) -peripheral neuropathy -transient myalgia, myopathy -cardiac: hypotension, bradycardia, Docetaxel more water soluble (more potent) than paclitaxel Hypersensitivity: major in 25% and minor in 40% ->bronchospasm, urticaria, hypotension, rash, flush -N/V, mucositis - arrhythmias -neurotoxicity Excreted in bile -met: p450 -resistance: same as vinca alkyloids b. Docetaxel -Epothalone A has similar 3. Epothilones a. Ixabepilone (Azaepothilone B) Breast ca, NSCLC, Prostate Ca, Gastric adenocarcinoma, head and neck Maj and minor HSR’s in 31% -D/N/V -erythematous, prurtic maculopap rash of forearms and hands in 75% Excreted in feces Met breast cancer -neutropenia, HSR’s, cardia (LV dysfxn or supraventric arrhythmia) -sensory neuropathy, CN palsy, ocular/visual changes, athralgia, myalgia, increased transaminases, N/V/A/D, abd pain, alopecia, rash Not as susceptible to resistance tubular polymerization as paclitaxel -Epothalone B more potenet than A or paclitaxel -binds β-tubulin subunit of microtulbules -promotes prolif and resists breakdown of mitotic spindles -binds multiple sites on microtubules G1 specific agents: 1. Asaparaginase hydrolyzes circulating Lasparagine to aspartic acid and ammonia resulting in inhibition of protein synthesis G2 Specific Agents: 1. Topoisomerase Ihibitors Topoisomerases are nuclear enzymes which make transient breaks in DNA allowing the cell to manipulate its topology •Functions: DNA replication, DNA transcription, Chromosomal segregation, DNA repair ALL ->-topoisomeraseI: acts on one strand of DNA, removes negative supercoils, no involvement in DNA replication, expression continuous during G2 phase of the cell cycle & in quiescent cells, ATP Met by liver; excreted in urine and feces HSR, ↓clotting factors (IX, XI, PC, PS, antithrombin III, fibrinogen; pancreatitis, neurologic toxicity, fever, chills, N/V -> Topoisomerase II: Acts on both strands of DNA, Removes positive supercoils Involved in DNA replication Expression increases during S phase of cylcle ~absent in quiescent cells ATP dependent -alterations in topoisomeras I -inadequate accumulation of drug in tumor -P-glycoproteins and MDR efflux pumps independent a. Camptothecin analogs (inhibit topoisomerase I) -Topotecan b. Epipodophyll otoxins (inhibit topoisomerase I) -Irinotecan c. Etoposide (VePeside, VP-16) -topoisomerase II inhibitor d. ANthracyclines -MOA: stabilizes cleavable complex where topoisom. I covalently bound to DNA at a single-stranded break site -conversion to lethal DNA damage follows when a DNA replication fork encounters these cleavable complexes Ovarian ca, SCLC -first converted by carbosylesterase to active metabolite SN-38, same mech as above Met colon ca topoisomerase II inhibitor -single strand breaks in DNAand inhibits topoisom II -late S phase/early G II -production of free radicals -disrupt membrane transport SCLC, testicular ca (refractory), ALL, AML, BMT, MM, MDS, lymphoma, gastric Myelosuppression (esp neutropenia), N/V, stomatitis, diarrhea, transient ↑s in liver enzymes, skin rash and alopecia Myelosuppression, neutropenic fever, diarrhea –acute cholinergic -> like sxs, D/N/V/A, chills, malaise, Can lead to dev of AML dizzy, visual disturbance, salivation, lacrimation, asx bradycardia, delayed-onset diarrhea, N/V, alopecia, fatigue, skin toxicity, increased liver transaminases Myelosuppression, N/V, alopecia, CHF, MI, stomatitis, 2˚ AML (<5yrs) pH conversion to active form; minimal liver metabolism –Excreted in urine –metabolized by the liver and intestinal mucosa –Excreted in feces S phase specific -inihibit topoisomerase II which leads to apoptosis -intercalation into DNA leading to inhibited synthesis Myelosuppression (can lead to AML) Neutropenia –GI toxicity: mucositis, diarrhea, delayed vomitting –Cardiotoxicity: •Acute: arrhythmias, pericarditis, myocarditis breast, soft tissue sarcomas, ovarian, NHL, HD, ovarian, 1. Doxorubicin ALL, AML (and a million other things) ALL, AML, 2. Daunorubicin Breast 3. Epirubici n ALL, AML 4. Idarubici n Breast 5. Mitroxan trone 6. Lipsomal Doxrbicin Slightly dif MOA, ↓ed free radical production, DNAreactive agent that intercalates into DNA thru hydrogen bonding causing cross links and strand breaks AML, ALL, Prostate Ca – hormone refractory phase,AML •Chronic: CHF, dilated cardiomyopathy –Red-orange urine discoloration –Radiation recall skin reaction, hand-foot syndrome *Dexrazoxane: -indicated for the reduction of cardiomyopathy asst’d w/ doxorubicin admin in women w/ met breast ca w/ high dose -may add to myelosuppression Presence of efflux pumps, Pglycoprotein and multipleresistance associated protein, which belongs to the ATP binding cassette family of transporters -pt mutations to binding site of DNA topoisomerase gen -increased inactivation of superoxide free radicals evades detection and destruction by the immune system –increases the time the drug is in the body Kaposi’s sarcoma, ovarian ca Bluish discoloration of sclera, urine, and finger nails; Less cardiotoxicity and N/V than, doxorubicin, HSR, Hand/foot syndrome –majority of the drug stays inside the liposome while in the blood (at least 90%) Cell Cyle Specific Drugs: 1. Platinums Cell cycle nonspecific -form DNA intrastrand adducts as opposed to DNA interstrand cross links HSR Altered cell accumulation of drug d/t impaired influx or enhanced efflux -cytosolic inactivation of drug -increased DNA repair -altered apoptotic process: drug induced apoptosis may be altered in cells that have MMR defects ->results in enhanced tumor cell survival and ↑ed resistance -widely distributed thru body and excreted in urine a. Cisplatin b. Carboplatin carboplatin induces same adduct formation as cispllatin, but must use 10x higher concentration cervical, esophageal, gastric, head/neck, lung, testicular, ovarian, bladder, breast, NHL Breast, lung, ovarian, NHL, bladder, testicular, head/neck Peripheral neuropathy, nephrotoxicity, tinnitus, delayed N/V, myelosuppression Anemia > thrombocytopenia, delayed N/V c. Oxaloplatin 2. Alkylating Agents Colorectal, ovarian, gastric -Alkylator attatches to alkyl groups to DNA bases resulting in the DNA being fragmented by repair enzymes preventing DNA synthesis and RNA transcription -Crosslinks w/ DNA resulting in inhibition of DNA synthesis Increased risk of 2˚malignancies Nitrogen mustard Breast, ovarian, NHL, sarcomas, endometrial, CLL Nitrogen mustard Nitrogen mustard Germ cell tumors, sarcomas, lymphoma, lung MM Nitrogen mustard CLL, HD, NHL, MM Uricaria, myelosup, pulm fibrosis, neurotoxicity Nitrosurea Brain tumors, HD, NHL Myelosup, pulm fibrosis, N/V, renal and hepatotoxicity Alkyl sulfonates BM transplant Myelosuppression, N/V, hepatotox, VOD, electrolyte abn’s, interstitial pneumonitis a. Cyclphosphamide b. Ifosphamide c. Melphalan d. Chlorambucil e. Carmustine f. Busulfan Acute-neuropathy (parasthesia, dsysthesia, of hands, ft, throat), chronic, cumulative neurotoxicity, N/V Myelosuppression(risk of MDS), hemorrhagic cycstitis, SIADH, hyperpigmentation, delayed vomiting , Myelosuppresion(risk of MDS) ,delayed N/V, dysuria, neurotox, SIADH, hemorrhagic cystitis Myelosup, N/V/D, mucositis, HSR 3. Non classic alkylating agent Antitumor Abx 1. Bleomycin 2. Mitomycin non-classice alkylating agent –Methylation of guanine residues in DNA which inhibit DNA, RNA, and protein synthesis Leukopenia, thrombocytopenia –N/V, anorexia –Headache, and dizziness –Elevated LFTs (40%) –Skin: rash, itching, photosensitive –Increased incidence of PCP (prophylactic treatment with Bactrim) From fungus -activation by oxidized iron to form oxygen free radicals resulting in DNA breaks Testicular, HD subacute and chronic pulmonary fibrosis, mucositis, skin (erythema/ hyperpig), HSR, vascul events: MI/ CVA/ Raynauds Intracell met; excreted in urine Antitumor antibiotic – isolated from Streptomyces caespitosus Anal cancer & gastiric ca Leucopenia, N/V, mucositis, HUS, interstitial pneumonitis, HSR Met by liver, spleen, kidney, heart; excreted in bile Apoptosis of APL cells –Degradation of the fusion protein PML/RAR-a Acute promyelocytic leukemia CV: Prolonged QT interval –GI: N/V/D/C –HA, myalgias, and bone pain –Leukocytosis (50% of pts) –neuropathy, tremors, insomnia –cough, sob, pleural effusions –Electrolyte abnormalities induces maturation of promyelocytes to myelocyte; thus decreasing proliferation APL Vitamin A toxicity symptoms: HA, fever, bone pain, nausea, vomiting, sweating, dry skin, mucositis, rash –Cross-link DNA resulting in inhibition of synthesis –Inhibits transcription by targeting RNA polymerase 3. Arsenic Trioxide 4. Trentinoin (ALLtransretinoic acid) –abdominal pain –Neuro: dizziness, confusion, depression –Increasing leukocyte count Hormonal Agents: 1. Tamoxifen 2. Aromatase Inhibitors -Anastrozole, Letrozole, etc 3. Fulvestrant Completely binds ER, inhibiting transcriptional processes -SERM: selective E receptor modulator Premenopausal breast ca pts Menopausal sxs, vaginal bleeds, peripheral edema, DVT/PE, endometrial hyperplasia/ca (2%) Inactivates aromatase and blocks the conversion of adrenal androgens to estrogn Post menopausal br ca Hot flashes, arthralgias, HA, flu-like sxs ER antagonits and downreg ER expression Met br ca Asthenia, hot flashes, flu-like sxs, HA Br/prostate ca Hot flashes, impotence, decreased libido, tumor flare – increasing bone pain, urinary retention, back pain Prostate ca Hot flashes, decreased libido, gynecomastia, myalgias, hepatotoxicity 4. LHRH Agonists -Leuprolide, Goserelin 5. Anti-Androgens -bicalutimide, nilutamide, flutamide Binds androgen receptor and inhibits androgen uptake Strong inhibitors of CYP2D6 SSRI’s: Paxil>Prozac>Zoloft>>Effexor *monoclonal Ab’s(traztusumab): HSR *Gleevec: Imatinib *procarbazine: an alkylating agent used for HL (part of MOPP) inhibits monamine oxidase so avoid cheese, wine, smoked meat) food and drug interactions *MOPP and ABVD (tx’s for HL): can lead to MDS *ABVD: tx for HL: Adriamycin (doxorubicin), bleomycin, vinblastine and dacarbazine *MOPP for HL: nitrogen mustard(cyclophosphamide), vincristine, procarbazine, prednisone *R-CHOP: tx for NHL: Rituximab+ cyclophosphamide, hydroxydaunorubicin (doxorubicin), Oncovin (vincristine), and prednisone/prednisolone Common acute toxicities: 1. Myelosupression: leucopenia, thrombocytopenia, and anemia (lowest portion (nadir) is usu 7-10 d) 2. Febrile Neutropenia: a. Neutropenia: <0.5 *10^9 cell/L and <1 *10^9 cells/L w/ predicted decrease in 48 hr b. Fever: >101 F (38.3C), and sustained tem >100 F (38 C) c. Infection risk correlates w/ depth and duration of neutropenia 3. N/V: stimulation of chemoreceptor trigger zone (CTZ) in medulla; stimulation excites dopaminergic paths which converge on adjacent emetic center a. Other paths also converge on this center including cortical and peripheral cholinergic neurons and vestibular serotonin and histaminergic neurons 4. Chemotherapy induced diarrhea: a. GI epithelial lining replace Q 3-5 d b. Toxicity to epith cells leads to inflame and secretory diarrhea c. Chemo most implicated: i. 5-FU, methotrexate, cytarabine, HD chemo ii. Irinotecan causes dose limiting diarrhea d. Early onset: cholinergic-mediate e. Late-onset: resistant to antidiarrheal tx and may be life threatening