S- CC-“I keep having these bruises appear on my legs and arms for
advertisement

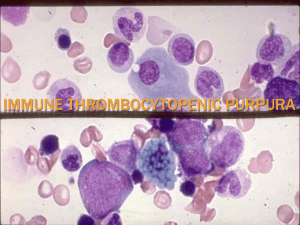
S- CC-“I keep having these bruises appear on my legs and arms for the last two weeks, and when I go to bed with a bruise and I wake up, the bruise is bigger than when I went to bed. I also have a rash on my legs. I have not had any injury to cause these bruises. The rash on my legs started before the bruises started to appear, about three weeks ago.” Patient denies any fatigue, changes in appetite, weight gain or loss, night sweats, changes in bowel or bladder habits, n/v/d/c/, she did not bruise easily prior to the onset of the above symptoms, she has had no changes in her menstrual periods, no hematuria, hematachezia, or hemataemesis, she denies recent illness, remainder of review of systems negative for any positive findings. PMH- allergic rhinitis Family History- Mom states that she is not aware of any bleeding disorders in her family history. Social Hx- Patient lives with parents, is a student, is a non smoker, no tobacco use, no drug use, no etoh use. Surgical Hx- right knee arthroscopy Medications- none current Allergies-nkda Vitals- BP- 98/72 HR- 88 RR-12, Temp – 98.8 General-13 year old Caucasian female, appropriate affect not toxic appearing Skin- pink, warm and dry, she has a petechial rash noted bilateral on both of her lower legs, non blanching with compression, she has multiple contusions of various sizes to both of her lower arms and to her upper and lower legs most appear deep purple in color, no sign of overlying skin trauma. HEENTHead-normocephalic, atraumatic, no suboccipital lymphadenopathy Eyes- pupils perla, conjunctiva pink, neck- no cervical lymphadenopathy, , thyroid palpated-no nodules palpable lungs CTA bilaterally all fields, no labored breathing, equal breath sounds cardiac exam- heart rate regular, no murmurs, rubs, or gallops noted abdomen- Round and non-distended with no scars or striae. No abdominal tenderness to palpation. Liver and spleen not palpable, normoactive tympanic bowel sounds x 4 quadrants, no abdominal bruits noted. Neuro- Mental status: Awake, alert, oriented to person, place, and time. No confusion, anxiety, or agitation noted. Cranial Nerves: II, III in tact, PERLA, + consensual movement, +accommodation, Cranial Nerves IV, and VI: EOM intact, Remaining Cranial Nerves: CN I not assessed. CN V and CN VII – XII grossly intact. Motor System: Muscle strength 5/5 in all extremities bilaterally. Gait steady w/o ataxia. Upper and lower motor reflexes grossly intact, Babinski not assessed, pronator drift not assessed. A- 1)Idiopathic Throbocytopenia 2) Thrombocytopenia secondary to viral suppression 3) Thrombocytopenia secondary to a leukemia, or aplastic anemia 4) Bleeding Disorder- Von Willebrand Disease, hemophilia C 5) Henoch-Schonlein purpura P- Patient given a lab slip and asked to report as soon as possible to have blood drawn for the following tests:- CBC, PT, PTT, INR, Sed Rate Patient was instructed on the signs of internal bleeding to include darkening of her stool, (black tar stools) or bright red blood per rectum, vomiting of blood or coffee ground material, weakness, lightheadedness, shortness of breath, blood in the urine, severe joint pain, if she were to experience any of these symptoms she is to return to the office immediately or report to the emergency room. Patient was instructed not to engage in any contact sports. We will follow up with her pending completion of her labs. Kelly L. Murray PA-S 08/27/2012 Addendum- patient’s blood work returned on the following day and her platelet count was 8000, Dr. Welmon advised the family to take the patient to Hershey Medical Center Emergency Room. Some viral infections can cause low platelet count by affecting the bone marrow, for example, •parvovirus, •rubella, •mumps, •varicella (chickenpox), •hepatitis C, •Epstein-Barr virus (EBV), and •HIV. Aplastic anemia (agranulocytosis) is the terminology for bone marrow failure leading to low platelet count usually associated with anemia (low red cell count) and leukopenia or leucopenia (low white cell count). Common causes of aplastic anemia include: •infections (parvovirus, HIV); •some medications [chloramphenicol, gold, phenytoin (Dilantin), valproic acid (Depakene, Depakote, Depakote ER, Depacon); ITP- Idiopathic thrombocytopenic purpura (ITP), also called immune thrombocytopenic purpura, is a blood-clotting disorder that can lead to easy or excessive bruising and bleeding. ITP results from unusually low levels of platelets — the cells that help your blood clot. Idiopathic thrombocytopenic purpura affects both children and adults. Children often develop idiopathic thrombocytopenic purpura after a viral infection and usually recover fully without treatment. In adults, however, the disorder is often chronic. Treatment of idiopathic thrombocytopenic purpura depends on your symptoms and platelet count. If you don't have signs of bleeding and your platelet count isn't too low, treatment for idiopathic thrombocytopenic purpura usually isn't necessary. More serious cases may be treated with medications or, in critical situations, with surgery. Von Willebrand Disease- The most common inherited bleeding disorder. The cause of von Willebrand disease is a hereditary defect in the gene that controls von Willebrand factor, a protein that plays a key role in your blood clotting process. When von Willebrand factor is scarce — or not functioning properly because of structural abnormalities — small blood cells called platelets cannot stick together properly, nor can they attach themselves normally to the blood vessel walls when an injury has occurred. The result is interference with the clotting process, and uncontrolled bleeding may persist. Von Willebrand factor carries an additional substance, called factor VIII, that helps stimulate clotting. Many people with von Willebrand disease also have low levels of factor VIII. Haemophilia C- Haemophilia C is a mild form of haemophilia affecting both sexes. However, it predominantly occurs in Jews of Ashkenazi descent. It is the fourth most common coagulation disorder after von Willebrand's disease and haemophilia A and B.[1] In the USA it is thought to affect 1 in 100,000 of the adult population, making it 10% as common as haemophilia A.[2] It is caused by a deficiency of coagulation factor XI and is distinguished from haemophilia A and B by the fact it does not lead to bleeding into the joints. Furthermore, it has autosomal inheritance, since the gene for factor XI is located on chromosome 4 (close to the prekallikrein gene); and it is not completely recessive, individuals who are heterozygous also show increased bleeding.[2] Many mutations exist, and the bleeding risk is not always influenced by the severity of the deficiency. Treatment is usually not necessary, except in relation to operations, leading to many of those having the condition not being aware of it. Henoch Schoelin Pupura- Henoch-Schonlein is caused by an abnormal response of the immune system. It is unclear why this occurs. The syndrome is usually seen in children, but it may affect people of any age. It is more common in boys than in girls. Many people with Henoch-Schonlein purpura had an upper respiratory illness in the weeks before. Signs and Symptoms include-•Abdominal pain, Joint pain, Purple spots on the skin (purpura), usually over the buttocks, lower legs, and elbows, Bloody stools, Hives or angioedema, Nausea •Diarrhea, Painful menstruation,Vomiting