Eyelids Function
advertisement
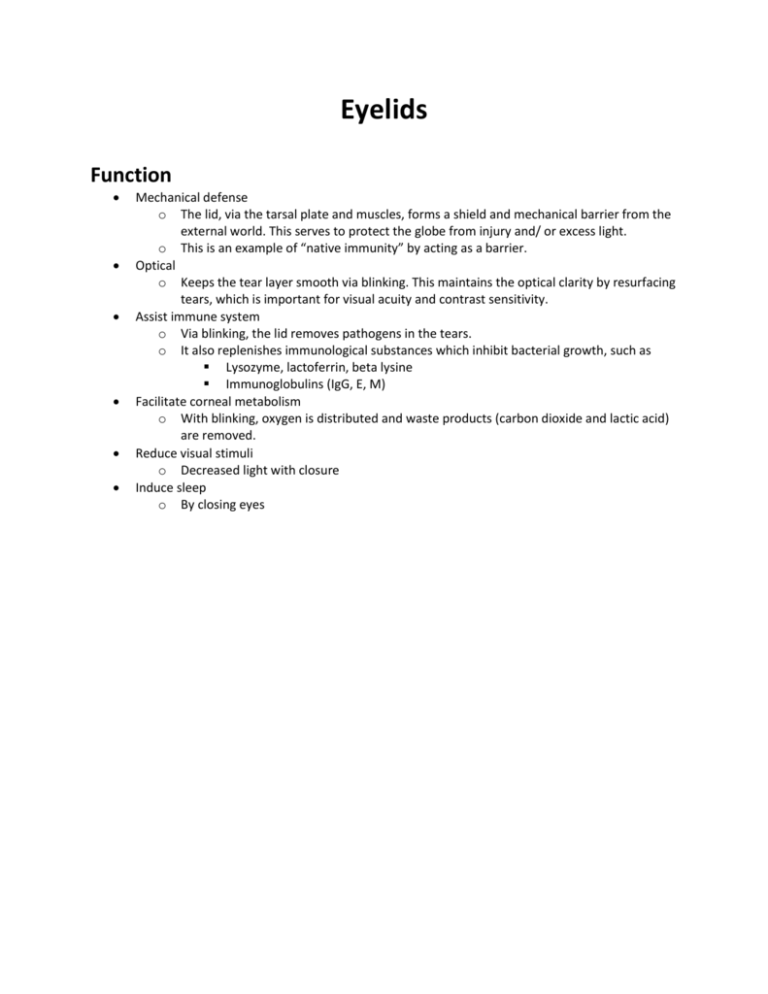
Eyelids Function Mechanical defense o The lid, via the tarsal plate and muscles, forms a shield and mechanical barrier from the external world. This serves to protect the globe from injury and/ or excess light. o This is an example of “native immunity” by acting as a barrier. Optical o Keeps the tear layer smooth via blinking. This maintains the optical clarity by resurfacing tears, which is important for visual acuity and contrast sensitivity. Assist immune system o Via blinking, the lid removes pathogens in the tears. o It also replenishes immunological substances which inhibit bacterial growth, such as Lysozyme, lactoferrin, beta lysine Immunoglobulins (IgG, E, M) Facilitate corneal metabolism o With blinking, oxygen is distributed and waste products (carbon dioxide and lactic acid) are removed. Reduce visual stimuli o Decreased light with closure Induce sleep o By closing eyes Anatomy General The lids are composed of two muscular membranous folds of skin that oppose the orbit. o One superior and one inferior. o The superior lid is larger and more mobile. There are two lamellas of the lids. o The anterior lamella is what is seen when looking at a patient. o The posterior lamella is located against the globe. It is only seen with inversion. o The transition of the two faces is called the Gray’s Line. This is seen on slit lamp. o Marx’s Line This is a line of squamous cells, extending along the entire length of the upper and lower lid margin and over the puncta, parallel to the lid margin. Marx’s line stains clearly with lissamine green. o The two lamellas can then be further divided into 5 structural planes Skin and subcutaneous fascia Eyelid protectors Orbicularis oculi Corrugators supercilii Procerus Orbital Septum and Fat The septum is the connective tissue immediately posterior to the orbicularis muscle that keeps the orbital content from herniating. With time and with chronic rubbing of the eyes, the septum weakens and allows herniation of orbital fat, which gives the appearance of “puffiness” and “bags” on the lower and upper eyelids. Fatty compartments o Three on lower eyelid (medial, central, and temporal) o Two on upper eyelid (medial and central. Temporal is replaced by lacrimal gland) Reatractors of the eyelids Levator muscle with its aponeurosis Muller’s muscle Capsulopalpebral fascia Inferior tarsal muscle Tarsi and conjunctiva Tarsal plate is the backbone of the eyelid. There are also two borders. o One border is adherent, which is continuous with the face. o The free margin is moveable. o Eyelid Crease This is formed by the extensions of the levator aponeurosis toward the skin. Although most Caucasians have an eyelid crease, about 50% of Asians do not have one. Lid Margin Position o The lid position of the lids is important for the health of the eyes. They must be firmly against the globe with blinks. o Normal upper lid Crosses cornea at 10 and 2 o’clock. Maximally under normal conditions covers about 1-2mm of cornea o Normal lower lid Grazes inferior limbus Covers 1/2mm of inferior cornea maximum o Apposition of lids and globe results from Tarsal plates Muscle of Riolan Lateral and medial palpebral ligaments Tissues The anterior surface is covered with skin o This is the site of the thinnest skin in the body. o Here it is a very loose, stretchy skin, allowing for considerable expansion of lid contents. o Recurrent edema and aging can cause loss of elasticity of the skin. o 10x more clinically sensitive to allergens than elsewhere in the body. Areolar tissue o Soft, loose, spongy connective tissue o Aerated, therefore lots of room for growth and easily distended. This is why eyelids swell with alcohol, allergies, kidney problems, no sleep, etc. o No cartilage is present. Tarsal Plate o Fibrous “skeleton” of lids o o Give shape and firmness to eyelids Gives the lid its “D-shape” “S shaped lid” refers to a lid mimicking a ptosis. It is caused by a mass within the lid, such as neurofibroma, hordeolum, chalazion. This is not a true ptosis since it is purely mechanical. Meibomian glands located deep in tarsal plates Structure Anterior Free Border o This contains eyelashes (modified cilia) that will be discussed later. They serve as protection since the base is well innervated and can trigger a blink reflex. Medial eyelid o Canthus This is the medial angle where the superior and inferior lids meet. It is significant for tear drainage. o Caruncle This is the mound of epithelial tissue. It is surrounded by a fold of tissue which is vestigial remnant of a third eyelid called the plica semilunaris conjunctiva. o Puncta These are the openings in the superior and inferior medial eyelids in which tears drain out. o Lacus Lacrimalis This is the collection of tears at the medial canthus. Ligaments o Septum orbitale Connects the tarsal plate to the bone, serving as a barrier to the back of the orbit keeping infections out of the orbit. o Lateral Palpebral Ligament This attaches the lateral ligaments from the canthus to the lateral orbital tubercle. o Medial Palpebral Ligament This ligament splits and attaches to the lateral wall of the lacrimal sac. This helps in tear pumping. Interpalpebral Fissure- space between eyelids Normal dimensions o 27-30mm long o 8-11mm wide o The two eyes should be equal Difference between palpebral apertures >1mm is abnormal. o No difference between men and women. o Typically do not see the sclera above and below the iris (12mm) o The position of the globe determines the fissure size. Aging changes o Circular in infants because of incomplete development Narrower in elderly due to decreased elasticity in fascia (ptosis) Pathophysiology o Von Graefe’s sign This is a lid lag. It is an inability of the upper eyelid to follow the downward movement of the globe. It results from retraction of the upper lid due to excessive sympathetic stimulation of Mueller’s muscle. o Collier’s Sign This is a tucked lid or extreme upper lid retraction. It may be caused by increased tonus of the levator resulting from a lesion of the IIIrd cranial nerve at the posterior commisure. Midbrain: interstitial nucleus of Cahal and nucleus of dark Scheiwitz. It is not a result of thyroid disease. o Pseudo Von graefe’s Sign This is also not thyroid orbitopathy. It occurs after recovery from a IIIrd cranial nerve paralysis. The fibers that were supposed to go to the LPS now innervate the MR and vice versa. With straight ahead gaze there is a ptosis on the side of the palsy (unilateral with primary gaze). In adducted gaze, the ptosis disappears. Glands of the Eyelids Meibomian Glands o These are the largest glands in the eyelids. o They are modified sebaceous glands. o Shape: long and skinny from free to adherent margins. o Visible only with inverted lids o Central canal is closed at the top Orifice is at the lid margin o Offshoots of central call called acini o Secretion- sebum (oily)- rich in fats and cholesterol Can be done with fingertips Function: contributes to the oil layer on the tears, retarding evaporation Lubricated lid ends so they do not stick 2-3 dozen in upper lid and 2 dozen in lower lid Only 6-8 glands produce lipid at one time, and that number of glands producing expressible lipid in the lower eyelid is correlated with dry eye symptoms. o Provide oily layer of tears o Secrete oil layer which acts as a barrier preventing spillover of tears onto lids. o The interactive force of an eyelid blink causes meibum to be excreted onto the posterior lid margin. This oil protects the eyelids from maceration and creates a seal when the eyes are closed, along with aiding the tears. Gland of Zeis o Type- sebaceous gland o Location- hair shaft- keeps hair soft o Function- lubricates cilia Gland of Moll o Hairshaft o Sweat gland? Function unknown Arrested in development Secretions of the Lids Major secretions from Meibomian Glands- Oil (Meibum) o This is the lipid produced by the meibomian glands (holocrine sebaceous glands) o Normal meibum appears as a clear, yellow free flowing liquid oil. However, intrinsic chemical changes of external action of bacterial lipases may oxidize the meibum or create free fatty acids. This change in lipid profile lowers the solubility characateristics and the lipid melting point, resulting in solidification, possible plug formation and problems with congestion or obstruction of the gland. o 20-30 glands in each lid o Oriented perpendicular to lid margin o Each gland has one central duct on the lid margin with areas of oily tissue adjacent to the duct (acini) Opened and closed due to the Muscle of Riolan. Released with blinked. o The oil is the top layer of the tear film. Accessory oil glands Glands of Zeiss and Moll o Accessory lacrimal glands Glands of Krause and Wolfring Secrete part of aqueous later of tears (5%) Blood vessels Arteries o Ophthalmic artery branches o Lacrimal artery branches o Empties into the veins of the forehead and temple. This is general, not specific. Muscles Levator (LPS) o Functions Raises upper eyelid Works with orbicularis in both involuntary blinking and forced lid closure. o Innervated by CN III o Starts at superior part of orbital apex and attaches to the front of the superior tarsal plate o Dysfunction of levator causes ptosis (3-5mm) Mechanical ptosis: heavy lid, usually from lid mass (chalazion)- due to gravity Myogenic ptosis: age-related or inherited levator deterioration. Change in muscularture, redistribution of fat, skin laxity. Neurogenic ptosis: due to CN III lesion causing poor levator function Congenital. Mueller’s Muscle o Functions Maintains tonus of elevated upper lid. Maintains tonus of opened lower lid o Innervated by sympathetic nervous system. Tonus changes with DFE. o Originates on underside of levator and attaches to upper border of superior tarsal plate. o Dysfunction of Mueller’s muscle slight ptosis (1-3mm), inverse ptosis. Orbicularis o Functions Closes lids Involuntary regular blinking Forced voluntary blinking Maintains apposition of lacrimal drainage apparatus (lacrimal puncta) against globe. o Innervated by cranial nerve VII, which also innervates muscles of cheeks and mouth. o Muscle is elliptically shaped. Attached to nasal and temporal edges of orbit by medial and lateral palpebral ligaments. “Palpebral portion” in lid only; responsible for involuntary blinking. “Orbital portion” in forehead, temples, and cheeks; responsible for forced lid closure. o Dysfunction of orbicularis Lesion of CN VII causes paresis or paralysis of orbicularis and also some facial muscles. Bell’s palsy o Very common. Unilateral loss of tonus Lagophthalmus0 eye remains open 2-3mm Loss of tonus of orbicularis and its ligaments allows puncta to fall away with resulting epiphora. Entropion resulting from forced lid closure; due to reduced tonus of lower orbicularis with inability to return lower lid margin to its normal position. Muscle of Riolan o Function Keeps the lid margin against the globe When open, it closes the opening of the meibomian glands Lymphatics Lymphatics in posterior lid drain the conjunctiva and tarsal glands. Lymphatics in anterior lid drain the skin and the associated skin structures. Lateral hald of eyelids lymphatics drain into the pre-auricular lymph node. Medial half of eyelids lymphatics drain into the submandibular lymph nodes. Nerves Motor Supply o Orbicularis supplied by the CN VII o Levator supplied by CN III Sensory Supply o From first two divisions of trigeminal (CN V) Ophthalmic division of trigeminal (V1) Branches to frontal, nasociliary, and lacrimal nerves. Maxillary division of trigeminal (V2) o o o o Upper lid mainly supplied by supraorbital nerve, part of frontal division, one of three divisions of V1. Medial side of the upper lid assited by: Supratrochlear, part of the frontal division (one of three divisions of V1). Infratrochlear, part of the nasociliary division (one of three divisions of V1). Lateral side of the upper lid assisted by lacrimal nerve, one of three divisions of V1. Lower lid supplied by infraorbital, one of the two divisions of V2. Indigenous Flora of the Eyelids Bacteria o Cultured from normal eyes Species % of Patients Harboring S. epidermidis 37 S. aureus 17 Diphtheroids 1 Combination of above 25 Misc. organisms in combination with above 9 Total 99 o Most common anaerobe = proprionibacterium acnes Non-bacterial flora o Pityrosporon ovale (orbiculare) Yeast No definitive pathogenic effect is known o Demodex folliculorum and D. brevis (arthropods) D. folliculorum in eyelash follicles D. brevis in sebaceous glands o Herpes simplex virus and HIV periodically excreted in tears without being associated with any disease process. Both die very quickly when exposed to air. Accessories Eyelashes o Derived from hair follicles at lid margin o First line of defense Highly sensitive sensors Produce reflex blinks of touched via nerve plexus at base of each lash. o Two rows on the upper and lower lids Upper lid- 100-150 lashes Project out and up. Lower lid- 50-75 lashes Project out and down o A single lash grows for about two months and falls out after 3-5 months Grows from typical hair follicle and eyelashes a typical hair Blepharitis- most common. Bacteria growing at base. o Glands located near lash follicle Glands of Moll (sweat) Glands of Zeis (sebaceous) These lubricate the eye, but site of a lot of infection and home of mites and lice. Physiology Movement Eyelid Elevation o Levator palpebrae superioris Innervated by III cranial nerve Inserts into the tarsal plate and also to dermal plate. Complete ptosis is due to LPS Origin: sphenoid bone at orbital apex. Insertion: into skin of upper eyelid. o Muller’s muscle- sympathetic innervations O: LP I: tarsal plate 2-4mm of eyelid elevation Partial ptosis due to MM A sympathetic lesion causes Horner’s Syndrome and a partial ptosis Anhydrosis- inability to swear and miosis. o Frontalis muscle- VII cranial nerve Only involved with extreme upward gaze. Eyelid Closing o Orbicularis Oculi A circular muscle surrounding the lids extending from the lids to the skull. Two portions Palpebral- on lids o More sensitive to stimuli, producing rapid eye closure. Orbital- on orbit o Distinguished base on excitability- palpebral portion has a lower threshold for excitation. Innervations: Cranial Nerve VII Exits the skull via stylomastoid foramen If nerve swells, it is cut off, causing Bell’s Palsy o Unilateral. All muscles on one side droop. Eyes cannot be closed. o Treatment: steroids reduce the swelling and lots of artificial tears. Frowning o Corrugators supercilii In orbicularis oculi VII cranial nerve Protects globe (pulls brow out) Yoked muscles o All of above o Obeys Haring’s Law of equal innervations Deals with innervations sent to two sides of body. Same neural stimulation to each. Says that fissure width should be the same on each side. o Sherrington’s Law of Reciprocal Innervation Deals with antagonists. If one is active, the other is inhibited. o Muscle actions Lid Synkinesis with eye Movement o Important that this be recognized on normal patients- can be quite confusing when evaluating patients with suspected lid-gaze dyskinesis. o Normal lid-gaze synkinesis 50% of abducting eyes- widen palpebral fissure 15% of adducting eyes- widen palpebral fissure o Abnormal- lid-gaze dyskinesis Duane’s retraction syndrome Parkinson’s disease- lid retraction on downgaze (pseudo von Graefe sign) Aberrant regeneration of CN III- lid retraction on downgaze. True von Graefe sign is lid lag on downgaze in Grave’s disease. Lid Reflexes Blinks are conscious, unconscious, and reflex Afferent Pathways o Trigeminal (V crainial nerve)- corneal and facial reflexes o Optic (II cranial nerve)- dazzle, glare and menace reflexes o Auditory (VIII cranial nerve)- auditory reflex Corneal reflex o Touch cornea ophthalmic division of trigeminal somatosensory cortex in the postcentral gyrus midbrain and pons (motor nuclei) inhibits the LPS and excites the orbicularis and lacrimal gland. The exact anatomical pathways are not well-known o CL patients adapt to this reflex- become desensitized (good and bad) o Last reflex lost under general anesthesia- how an anaesthesiologist checks o First reflex lost with cerebellar pontine angle tumor Passes on brainstem affecting CN III and VII o Reflex latency about 160msec- time damage can occur. Facial Reflex o Tap near orbit ophthalmic or maximllary division of the trigeminal midbrain pons inhibit LPS and excites the orbicularis. o Normal patients can withhold this reflex o Gage level of development in infants Before tw months they blink. After 3-4 they stop. o Patients with parkinsons disease cannot. This is called Meyerson’s sign. Dazzle Reflex o Bright light optic nerve LGN visual cortex somatosensory cortex in the postcentral gyrus superior colliculus brainstem inhibit the LPS and excites the orbicularis. o Remains in decorticate animals, thus is also a subcortical pathway. No anatomical connection between the retina and superior coliculus. Menace Reflex o Approach of foreign object optic nerve cortical association area (area of recognition) post-central gyrus brainstem inhibit LPS and excite the orbicularis Glare Reflex o Glare optic nerve LGN striate cortex post-central gyrus brainstem inhibits the LPS and excites the orbicularis Auditory Reflex o Loud noise auditory nerve pons inhibit levator and excite orbicularis Blinking Purpose o Allows LPS to relax o Creates tears o Allows the retina to relax (retinal metabolism greatest in dark) Blinking occurs at regular intervals (approximately 12-15 times per minute) o This is about once every 5 seconds. It iis specific and constant with each individual. o Affected by Excitation level Excitation leads to increased blinking Ocular irritation Increased irritation leads to increased blinking Concentration level Increased concentration and staring leads to decreased blinking Studies o Doane created a new setup to study blinks with mirrors, etc. Said he was monitoring VA so their blink rates were more normal. Results Eyelids closed due to only the upper eyelid. The lids close like a zipper, starting laterally and closing in a medial direction. Dynamics of eyelid motion o Top eyelid comes down (not the bottom up) Visual effects of blinking o Eyelid about 2 log units NDF which decreased the retinal illumination 100x. o Blink suppression You do not see the effect of the lid closing due to neural signals. Eyelid a low spatial frequency and high temporal frequency (fast) magnocellular So this is suppressed. Just luminance into, not color. Occurs in the LGN. Parvocellular not suppressed, because high sptial frequency. o Saccade Suppression Clinical Evaluation of Lid Position and Function Clinical o Lid evaluation is easily, quickly merged into the external eye evaluations, starts upon meeting the patient. Scan for gross abnormalities. o Closer inspection can be obtained by use of the penlight- generally do not need significant magnification to evaluation the lids (generally no magnification is adequate). o Clinical evaluation- questions to be asked. Is the palpebral aperture height normal? Are the lids in normal position? If not in normal position, which is abnormal? Is ptosis or retraction present? Is lid function normal, i.e., lid retraction and closure? Lid shape, color, skin abnormalities, etc.- other structural abnormalities? Clinical Procedures to Evaluate Lid and Function of Lids o Palpebral height measurement PD ruler, through widest point, upper margin to lower margin Do not let the patient squint. o Lid Eversion General Information Indications for lid eversion o Suspected foreign bodies o “Lost” CL o Anterior segment infections o Prior to contact lens fitting o Evaluation for GPC o Routine baseline lid eversion also recommended Single vs. double eversion o Single eversion reveals the superior palpebral conjucntiva between the superior edge of the tarsal plate and the lid margin o Double eversion reveals the conjunctiva between the edge of the tarsal plate and the superior fornix o o Procedures Single lid eversion o The upper lashes are grasped and pulled away from the globe o Pressure is then applied on the upper superior surface of the lid with finger or cotton-tipped applicator while the patient looks down o The lid is everted over the edge of the tarsus o Eversion can be maintained using light pressure with the thumb pinning the lashes against the bony orbit o To return lid to a normal position, pull out the lashes and move downward Double lid eversion o The upper lashes are grasped and pulled away from the globe o A Desmarred retractor is placed against the lid above the tarsal plate with the handle pointing toward the clinican and the lip facing slightly downward (a bent paperclip can also be used) o The lid is folded back over the lip of the retractor o The retractor handle is rocked back to expose a view of the superior fornix. Don’t raise the retractor o Tilting the patient’s head back and viewing from a slightly inferior angle enhances the view of the fornix area o Use a stand lamp or transilluminator for better illumination o Some foreign bodies may be flushed away from the eye with saline or eye rinse. Evaluation of orbicularis function (CN VII) Undications: suspected CN VII damage, most dry eye patients Passive lid closure Forced lid closure Evaluate orbicularis function and evaluate Bell’s phenomenon Have patient look down, grasp lids with thumb of each hand. Patient should forcefully attempt to close lids Watch for o Asymmetry in strength of response o Symmetric weal response o Normal Bell’s phenomenon Up and out is typical response 50-85% have up and out Some patients have no Bell’s, or other variant Conjugate deviation to left or right may indicate postchiasmal mass Bell’s occurs eve in double elevator palsy- should be present. Evaluation of LPS function Technique Patient looks down (no LPS tonus) to up (maximal tonus). The difference in lip position is LPS function. Measure the excursion of superior lid with PD ruler Be sure to neutralize action of frontalis. Normal LPS function is approximately 15mm, good function approximately 8mm, poor<4. With poor orbicularis function, lagophthalmos is likely Pathophysiology Congenital Anomalies of Eyelid Form, Position, Function Epicanthal Folds (Epicanthus) Background o Congenital structural anomaly where a vertical fold of tissue continuous with the medial upper lid margin continues downward and conceals the medial canthus (ddx from inverse epicanthus). o Very common in Asians of all ages. o Very common in Caucasian infants, probably related to flat bridge. As bridge develops, epicanthal fold remiss. Significance o Often will cause pseudostrabismus appearance- esotropia o Common complaint of “eye turn inward” by parent o Common referral from pediatrician o Can be accompanied by congenital ptosis or epiblepharon- be sure there are no other congenital anomalies Differetntial diagnosis from true esophoria o Pinch skin medially at bridge of nose and observe o Compare andgle kappa to Hirschberg o Cover test, motilities o Evaluate monocular acuities if possible (could evaluate reaction to occlusion of each eye). This is to rule out strabismic amblyopia. Management o o o o Reassure parents (if you are certain that there is no strabismus or amblyopia) Advise of wise decision to rule out strabismus Advise of cause and nature, demonstrate epicanthus Send consultation letter to pediatrician for wise referral Full evaluation of the child’s visual function to ascertain equal visual acuity at early age. If pseudostrabismus and unsure, re-evaluate child in 1-3 months or obtain consultation with a doctor who has a special interest in children’s vision, i.e., OD, pediatric ophthalmologist. Coloboma of Lid Background o Very, very uncommon (rare) developmental anomaly o Some people call trauma-related partial excisions-colobomas- they are not truly coloboma. Significance o Congenital anomaly- rule out other congenital anomalies such as limbal dermoids, cranial dystoses, facial anomalies. o If large, then eye is not adequately covered during lid closure resulting in dessication and scarring. This is due to the lack of lid resurfacing. No pre-corneal tear film. Epithelial dessication. Basement membrane and stromal damage. o Non-hereditary, may be bilateral. o Usual location: upper lid in 90% of cases (unlike iris, lens, retina, choroid, ONH colobomas) junction of medial 1/3 of eyelid with middle 1/3. Appearance o Notch or cleft in lid margin (may have associated notch in brow) o Rounded borders with no lashes or meibomian glands Management o Evaluate foro t her congenital abnormalities o If small and without evidence of epithelial dessication (and no cosmetic complaint) reassure and explain. o If epithelial dessication Lacrilube qhs and tears prn o If large (approximately 3/) with large degree of corneal exposure, surgical management ASAP (oculoplastic specialist) strongly advised to prevent corneal scarring and secondary vision loss. Use Lacrilube until surgery to prevent corneal dessication Blepharophimosis Background o AD o Congenital anomaly; smaller than normal palpebral fissure width (height also reduced so that “eyes look small”. o Normal palpebral aperture width Adult average 30mm; 26-35mm range Child 25-28mm Blepharophimosis 20-22mm o Very uncommon Significance o Little significance by itself but as with other congenital anomalies tends to be accompanied by multiple congenital defects o Often triad of blepharophimosis, ptosis, epicanthus inversus Management o Watch out for blepharophimosis-ptosis-epicanthal inversus syndrome; significance is the ptosis. Can cause amblyopia anopsia )note difference from regular epicanthus) o Look for other congenital anomalies telecanthus and ectropian o Usually needs surgery Cryptophthalmos Lids not separated Euryblepharon Congenitally wide palpebral aperture No treatment necessary Telecanthus Large distance between medical canthi No treatment necessary Hyperteleorism Widely spaced orbits Usually accompanies the congential anomalies of branium formation (AD) craniofacial dystoses (such as Crouzon’s = broad forehead, wide skull, hyperteleorism, shallow orbits exposure keratitis, high palate, etc.) exophthalmos, divergent strabismus, optic atrophy, exotropia. Distichiasis Congenital anomaly (AD) characterized by absence of meibomian glands which have an extra row of lashes (3 total) at their location Rare, usually familial Lashes tend to turn in to touch the globe (trichiasis) Acquired form of distichiasis exists where a hair follicle forms within or adjacent to the meibomian gland. Can be caused by Stevens-Johnson syndrome, pemphigus, chemical burns. Tends to cause severe trichiasis. Tristichiasis Very rare Three rows of lashes Normal meibomian glands Mongloid Slant Common in Asians Also occurs in Down’s syndrome (trisomy 21) Antimongoloid slant o Lateral canthus lower than medial canthus Goldenhar’s Syndrome Oculoauriculovertebral dysplasia Congenital Ptosis Onset at birth o Watch for congenital anomalies In patient beyond 1 or 2 years of age a ptosis will generally be acquired, however, congenital ptosis should be considered and ruled out. o History o Superior lid sulcus is absent If there is a sulcus, it is acquired. o Old photos Differential diagnosis is very important since the congenital form is not usually accompanied by ongoing neurological disease (exception is neonatal myastyhenia gravis) Significance of congenital ptosis o Occlusion amblyopia, aka deprivation amblyopia o If significant degree of ptosis, get surgical consult to prevent occlusion amblyopia (pediatric ophthalmology consult) Types of congenital ptosis o Autosomal dominant Approximately 70% are AD Check family members Also look for other congenital anomalies if obstructing pupil significantly pediatric ophthalmology consult for surgical correction of ptosis o SR palst with LPS palsy Double Palsy/ Double Elevator problem Isolated SR palsy congenital is very, very rare. Look for vertical tropia in primary position with ptosis Also has a problem looking up. o Paradoxical CN III innervations Congenital Marcus Gunn jaw winking = ptosis accompanied by retraction during stimulation of ipsilateral pterygoid muscle. Amblyopia secondary to ptosis in 20% of these cases. This is due to an anomalous connection between the jaw and the LPS. Other anomalies Duane’s Retraction Syndome o Abduction palsy and with forced abduction eyelids open. o With adduction, lids close o Absence of abducens nucleus in pons Brown’s Syndrome o Swelling of SO tendon o With adduction, it is hard to open eyes o Decreased adduction and elevation Management: surgery for ptosis Acquired pseudo von Graefe sign (lid lag) Try is related to thyroid eye disease o Congenital Horner’s syndrome Look for heterochormia irides (suggests onset prior to age 2) Due to decreased innervations Triad: ptosis, change in pupil size, decreased pigmentation due to decreased sympathetic innervation o Birth trauma Not common at all o Neonatal myasthenia gravis Also uncommon Tips in diagnosing congenital ptosis o History (may be reliable) o Old untouched photos (most parents have lots of baby pictures) o Superior lid sulcus absent o Lid lag (slight) in downgaze due to inelasticity of the lid Eyelid and pupil should drop at the same time. Lag = lid moves slower Management aspects o If significant obstruction of pupil and/or apparent reduced acuity or dislike for fixation with the eye then consult with pediatric ophthalmologist is strongly advised. Ptosis must be eliminated to prevent occlusion amblyopia. o Pediatric neurology (or ophthalmology) consult if congenital Horner’s or suggestion myasthenia gravis. Epiblepharon Looks like entropion. It is secondary to forming and pushing the lashes into the eye Generally grows out of it. Treat with artificial tears Acquired Anomalies of Eyelid Form and Position Ankyloblepharon Adhesions between upper and lower eyelids along the lid margin Results from significant mucocutaneous disease, i.e., ocular pemphigoid or as a congenital anomaly (autoimmune) Usually at outer canthus (external ankyloblepharon). Can be inner canthus (internal) Causes pseudostrabismus Treatment: symptoms with cyclosporine and or steroids. Symblepharon Adhesion of the palpebral tarsal conjunctiva to the bulbar conjunctiva resulting generally fron significant inflammatory disease, Stevens-Johnson syndrome, pemphigoid, alkali burn- due to autoimmune disease of mucocutaneous junction Occurs as tarsal conjunctiva and bulbar conjunctiva heal. Prevention is easier than treatment bid to qid breaking of adhesions with glass rod. Immunosuppressant drugs: prednisone/ cyclopsporin Vitiligo Patchy depigmentation of the skin Bilateral, starts at about 20 years olf AD Progressive More noticeable if darker pigmented. In ocular disease, skin of eyelids affected Usually accompanied by depigmentation of lashes poliosis Alopecia depgmentation of hair, tends to accompany these, i.e. poliosis, vitiligo Entropion Background o Condition where the eyelid margin turns inward toward the globe- more common in lower lid Significance o Can result in trichiasis, but not necessarily. Can lead to blindness With blinking, changing gaze the lashes scratch the cornea Can cause infection, ulcer, etc. Types of entropion o Congenital entropion Usually other developmetal anomalies Cause is usually deformity in tarsal plate development causing entropion Management is surgical reformation of tarsal plate Epiblepharon-horizontal lid skin fold physically pushing lashes toward globe (trichiasis). Management: surgical excision of excess skin. o Cictricial entropion Cicatrix = scar Cicatricial entropion caused by scar on tarsal conjunctiva with contraction of scar tissue resulting in tractional entropion Usually cause is inflammation of tarsal conjunctiva such as trachoma Other causes Chemical injuries Lacerations Surgical procedures o Spastic entropion Caused by excessive contraction of palpebral portion of orbicularis (or very rarely atrophy of the lid retractors) Most common cause is blepharospasm due to ocular irritation, injury, inflammation (conjunctivitis, keratitis, etc) Treat with muscle relaxants. o Atonic (involutional, senile) entropion This is a change in the muscle tone. Common in lower lid, not in upper lid. Occurs in elderly due to age-related lid changes Lower border of lower tarsal plate (in inferior lid) rotates outward and superior border rotates upward due to Elongation (stretching) of lid structures laxity of tarsal plate and orbital septum Lower lid retractors (capsulopalpebral head of inferior rectus and inferior Muellers muscle) Atrophy of orbital fat with age enophthalmos Orbicularis spasm (possibly?) Signs and Symptoms o Trichaisis causes mechanical damage which can cause Discomfort, FBS, irritation, tearing Corneal epithelial defects secondary corneal infections, ulcers, damage and scarring in anterior stroma Vision loss can result from entropion with secondary trichiasis Management of entropion o Careful evaluation of anterior segment to determine cause of entropion Rule out ongoing anterior segment disease; foreign body (evert lids and inspect very carefully) to rule out a cause of spastic entropion Rule out scar in palpebral conjunctiva (cictricial entropion) Evaluate laxity of the lid Pull lid out. Entropion should resume with blink. o Management is most effective if cause can be found and eliminated. Manage lid disease- trachoma Epilation of lashes if symptomatic, temporary treatment for trichiasis only. Does not treat the entropion. Lashes will grow back and trichiasis will recur in a few weeks. If trichiasis is prese nt with significant epithelial defects, broad spectrum antibiotic such as gentamycin or polysporin (gtt and ung) as indicated to prevent keratitis Surgical management most successful for atonic entropion If surgery is refused by patient, could consider electrolysis to prevent trichiasis (not treat entropion). Also helpful if >1/3 of lashes are touching the globe Bland ophthalmic ointment is helpful Bandage CL also viable Ectropion Background o Lid margin turned outward away from globe such that lid margin is not in contact with globe o Inferior tarsal conjunctiva is exposed, possibly inferior cornea o Usually lower lid, usually in elderly (atonic form of ectropion) Significance o Dessication (keratinization of palpebral conjunctiva) of conjunctiva, cornea discomfort and tearing, infection o Lacrimal puncta not in opposition to globe epiphora o Patient may complain of an eye that waters all the time. Also increased watering due to reflex of dry eye irritation Types of ectropion o Cicatricial ectropion Scarring on skin of lid Can also occur in active dermatitis of lid Past trauma (laceration, burn) of skin o Paralytic ectropion Post trauma (injury, burn) or surgery CN VII palsy (Bell’s palsy) o Involutional (atonic, senile) This is the most common. It is bilateral Laxity of lid tissue in lower lid Gravity pulls the lid away from the globe Signs and Symptoms o Dessication of lower conjunctiva and cornea o Irritation, dry eye symptoms o Epiphora- watery eyes. Tears falling on face. Excess tearing is just aqueous. Not quality. o Widely opening mouth Cicatricial- worse Involutional- no change o Lid lax, puncta not in apposition to the globe. Evaluation of ectropion o Symptoms- epiphora o Gross observation o Pull lid away from globe slow or no return Management o Goal is to prevent discomfort, tearing, secondary keratinization and/or infection o Prevent dessication of conjunctiva and discomfrt by use of lubricant Artificial tears (qih or qid recommended)- never prn Bland ophthalmic ointments qhs o Possible EWCL to protect the cornea- serves as a reservoir for moisture o Broad spectrum antibiotic if recurrent infection such as blepharitis, conjunctivitis or keratitis o Tape lid at medial canthus to tighten it (with durapore tape) o Surgical treatment- best for age-related Floppy Eyelid Syndrome Triad of obesity, easily everted “floppy” upper eyelids and an associated papillary conjunctivitis Patients may suffer from obstructive sleep apnea that results in hypoxia from snoring and obstruction of the upper airway when they sleep on their back. Because of this, these patients will often sleep on their side with their face pressing into a pillow, everting an already lax upper eyelid and causing mechanical inflammation and irritation to the conjunctival surface. The upper eyelid is the primary lid involved and is rubbery, floppy and easily everted when the lid is mechanically elevated. Eyelash ptosis o The eyelashes point downward and curl toward the cornea. Most common slit lamp finding is punctuate epithelial keratopathy, with keratoconus being the second most common finding. Seen more in overweight patients, mens, those with sleep apnea Complain of chronic irritation Can evert lid with fingers Treat with lid hygiene and change sleeping positions Conservative treatment o Bland topical ointment for lubrication and wearing a plastic or metal eye shield at night. o Surgery of the involved eyelid in chronic nonresponding cases involves the eyelid horizontal tightening techniques such as a full thickness pentagonal wedge resection or a lateral canthal strengthening procedure. Lax Eyelid Syndrome o A variant of FES o This is thought to be much more prevalent o Similar characteristics, such as lid hyperlaxity and ocular irritation, but it does not include the other findings of obesity, easily inverted tarsus and papillary conjunctivitis. o This can be associated with obstructive sleep apnea as well. Eyelid Imbrication Syndrome o This is a rare cause of congenital eyelid malposition. It may be caused by inborn laxity of the upper medial and lateral canthal tendons that are tightened during the postnatal period. Blepharoptosis Most common connotation of ptosis upper lid droops downward/ Numerous causes Inverse ptosis- lower lid up due generally to Horner’s Syndrome Retraction Disorders of Orbicularis Function Lagophthlmos Background o Inability to completely close the lids. Remain open 2-5mm Significance o Usually results in exposure of the globe causing epithelial dessication; c/o dry eye, scratchy eye, possible secondary infection and/or corneal ulcers. Sterile ulcers can result. Common causes/classification o Paralytic of orbicularis (CN VII palsy)- Bell’s palsy o Orbital Corneal apex more anterior than normal, ex. Keratoconus Differential diagnosis includes Globe displaced forward (retrobulbar mass, thyroid disease) Larger than normal axial length (high myope) Shallow orbit (rare) and normal sized eye o Neurogenic Stimulation of retractors (Mueller’s muscle) Hyperthyroidism (Grave’s disease) is most common cause Mechanical and neurogenic o Mechanical Scarring Active lid disease o Physiologic or nocturnal lagophthalmos Symptomsinclude burning and irritated eyes, especially in the morning. Signs and symptoms of lagopthalmos o During sleep lids not in apposition tear film evaporation- epithelial dessication o Symptoms of dry, scratchy, irritated eye upon awakening o Look for punctuate epitheliopathy across inferior cornea- this may not be present or may be positioned elsewhere. o Check for Bell’s phenomenon (although this is probably unrelated to position of globe during sleep) o Check positive lid closure, may need to recline patient o Ask spouse if patient sleeps with eyes open o Check whether blink is complete. Check blink rate o Evaluate for anterior segment diseases, especially blepharitis Management o Mild symptomatic lagophthalmos Artificial tears (q1h to qid recommended) Increased frequency should require decreased preservatives. Can induce medicamentosa, increased toxicity Bland ophthalmic oithment qhs if needed (Lacrilube) o Moderate Artificial tears, ophthalmic lubricants qhs Tape from cheek to brow/forehead while pulling lower lid up. Moisture chamber (Saran wrap sealed with tape- Transpore surgical tape or Dermocel) For more extreme cases o Use broad spectrum antibiotics if significant corneal epithelial dessication or damage (to prevent secondary infection) o Surgery (tarsorrhapy) This is not permanent o Surgical thread to sew top and bottom lids Patient can open and close it like shoelaces. Must have regular follow-up to rule out infection or serious drying; every 3 months or more frequently. Blepharospasm Background o Involuntary contraction of orbicularis- scrunches eyes tight. o Generally bilateral and symmetric, though onset may be unilateral o Older individuals, late 40s, females > males Innate psychological/neurological problems? o Severity progresses over 6 months to 3 yearrs, then it diminishes. o Does not occur during sleep o Fatigue and stress may increase intensity o Unknown cause, possibly due to chemical imbalance and/or misfiring of neurons of basal ganglia. Takes a lot of energy Signs and symptoms of blepharospasm o Involuntary lid closure o Facial muscles (jaw, tongue, lower face, mouth) o May be so severe as to cause secondary tempero-mandibular joint syndrome (TMJ) o Various sensory “tricks” may suppress the severity of the contractions Commonest is placing a finger at the lateral margin of the orbit and slight massage. Others: coughing, yawning, talking, humming, or singing o Differential diagnosis very complicated Ocular disease (local irritation, inflammatory process, or foreign body) Check for anterior segment problems Myokymia- lid twitch. Unilateral. Sporadic. Tardive dyskinesia caused by antipsychotic medications (Prolixin, Haldol)- induce tremors Various neurological disorders- MG, MS Functional (hysterical) Treatment of blepharospasm o Treat any anterior segment disease first o Counseling since patient is quite self-conscious. o Counseling for depression since many activities of daily life and work are interrupted. o Medications interfering with nerve conduction are variably, but not consistently, successful (antidepressants) o Botulin A toxin injections (Botox) Interferes with neural transmission Relief of symptoms averages three months Typical side effects Ptosis Subcutaneous hemorrhage at injection site Dry eyes Double vision Exposure keratitis Side effects resolve as toxin wears off o o Surgery Myectomy and/or partial neurectomy Myectomy removes squeeze muscles in upper lid, eyebrows, forehead, and base of nose Neurectomy consists of resection and removal of small facial nerve branches of innervating orbicularis Referral to national support groups and organizations for individuals with blepharospams. These patients are usually suicidal Blepharoclonus Background o Exaggerated reflex blinking characterized by increased blink rate or length of lid closure time Causes o Often no cause found (psychological?) o Commonly in children 5-10 years old with no apparent cause, but parents are distressed- this is the most common presentation Evaluation o Workup is the same as for blepharospasm- rule out anterior segment disease, irritation, foreign body, etc. complete eye exam. Management o Reassurance- self limited disorder o Consult with neurologist if desired o Numerous surgical procedures to interrupt CN VII have been tried. Myokymia Background o Eyelid tic or twitch o Mild to moderate faciculations of orbicularis o Multiple causes Fatigue, lack of sleep Stress, anxiety, tension Anterior segment irritation Light dazzle Anemia, nutritional deficiency Excessive use of tobacco or alcohol Antocholinesterases used therapeutically ( physostigmine, neostigmine, echothiophate) Also causes punctual stenosis, causing myokymia Rare: MS, MG, trigeminal neuralgia Signs and symptoms o Patient aware of annoying twitch Unilateral More often lower lid o Examiner generally sees nothing wrong Treatment o Reassurance Rest, good diet/hydration o Rule out irritation, infection, inflammation o Consultation with family MD or psychologist to evaluate stress, tension, or neurologist if accompanying neurological signs present o Pharmacological treatment Topical antihistamine drops, q4h in affected eye Antazoline Pheniramine Levocabastine (Livostin) Oral antiemetic (Rx) is an alternative. Not the first choice Promethazine (Phenergan) 12.5-25mg qd-tid Tripelennamine (PBZ-SR) 75mg, qid Stubborn cases may warrant oral quinine 200-300mg, qd-tid; Contranindicated in pregnant women, since increases risk of abortion. Disorders of Eyelashes Trichiasis Background o Lashes touch globe Causes o Numerous causes including any cause of entropion, growths on lid margin, lid trauma, scarring of conjunctiva (trachoma, Stevens-Johnson syndrome)- autoimmune disease o Blepharitis is most common cause o Could be congenital, ex. Asians have short, sharp lashes Signs and Symptoms o Discomfort or pain, FBS, injection o Chronic tearing due to FBS o May traumatize the epithelium Corneal epithelial defects- infections, ulcers Damage and scarring of conjunctiva or cornea o Can cause vision loss due to corneal scarring Evaluation o Find the underlying cause of the trichiasis if possible Blepharitis is a common underlying cause o Careful slit lamp evaluation for both trichiasis and epithelial damage o Use fluorescein- check for staining; epithelial damage (tracks) Management o Epilate in-turning lashes Forceps or epilation tweezers (disposable) Soak tools in zephiran chloride solution (1:3000) with rust tablets added, if not disposable Can anesthetize the lid. o o o o o o This is not as necessary Proparacaine is acceptable Have the patient look in the opposite direction. This moves the cornea out of the way. Firmly grasp last at its base and pluck as close to the lid as possible. Do not clip lashes. This sharpens the edge. No antibiotics are required. Patients should not do this themselves. Lashes grow back Children: 2-4 weeks Adults: 4-8 weeks Cauterization of follicles generally gives poor results, because this damages the meibomian glands. Electrolysis destroys the last follicles. This is successful, but it is quite painful. If >1/3 of lashes are turned in, surgery is warranted rather than electrolysis Cryosurgery- freezing Decreased pain and decreased problems with management Argon laser photocoagulation Kills the follicles Regular use of ocular lubricants q1h to qid Prophylactic broad spectrum antibiotic coverage (bacitracin, polysporin, or gentamicin) Poliosis Whitening of lashes o Unilateral/bilateral, top/bottom/both Usually due to staph blepharitis if isolated o Can also be due to aging and inflammation. Look for related signs of inflammation Vitiligo is not due to staph If both poliosis and vitiligo, evaluate internal ocular health (c/o uveitis) o If negative, get dermatology consult. Treatment: none. Get lids healthy. Use mascara. Madarosis Background o Lash loss Causes o Very common cause is staph blepharitis o Also consider trichotellomania (neurotic pulling of lashes) Treat with use of mascara. It is harder to pull out and prevents picking. o Rule out systemic conditions )meds, hair loss elsewhere) o Scarring Evaluation o Look for any evidence of staph blepharitis o Rule out anterior segment disease of any kind (especially staph) Management o Treat blepharitis if present (lid scrubs, etc) o Photodocument to monitor therapy Ingrown Cilia Background o Eyelash growth into the epidermis of the lid Significance o Can be detected against globe (trichiasis)- may have FBS Evaluation o Look for more than a single ingrown cilia o Look for cause, lid trauma and scarring Management o Cut lash follicle with a sterile needle o Remove distal portion of lash o Epilate remainder of lash o Prophylaxis with antibiotic Age-Related Acquired Lid Anomalies Dermatochalasis Background o Redundancy of skin of the upper lid such that it drapes downward over lid margin. May look like ptosis- hold the redundant skin flap up. Pull the lids up at the lateral angles. If equal and grazing cornea at IO and 2, then it is dermatochalasis o Middle aged to elderly patients; bilateral o May be familial tendency o May have herniation of orbital fat thorough the orbital septum causing puffy, “swollen” appearance Evaluation o Usually quite easy to notice and diagnose o Watch for true ptosis and for lid edema Management o If no trichiasis and no field loss, the problem is cosmetic only- reassure the patient It is a natural process o If trichiasis, treat it. Consider surgery- cryo, electrolysis, etc. o If field loss and desire to obtain cosmetic improvement, do a careful formal visual field evaluation with and without lids held to document functional vision defect (10 degree difference in VF loss). Insurance needs this in most cases to allow a claim for blepharoplasty. o o Do this on two separate days, since it is long. Surgery- (blepharoplastry) remember VF necessary with and without lid held to obtain insurance funding. Referral to oculoplastic specialist or cosmetic surgeon Blepharochalasis Background o Younger to middle aged patient with baggy lids secondary to recurrent swelling of lids due to recurrent inflammation or edema (systemic, allergic, etc. o These recurrences of edema result in stretching of periorbital skin, loss of elasticity o Superior lid drapes over lid margin in many cases o May mimic ptosis. Be sure to rule out true ptosis. Note that a ptosis (not of neurogenic origin) can result from damage to the levator aponeurosis. May be in some cases with familial tendency. Evaluation o Same as dermatochalasis o Rule out active cause, i.e., lid mass, edema, inflammation o Rule out ptosis o Look for underlying cause- recurrent edema due to allergy, high BP, kidney disease, cardiac disease. Those that reduce circulation Management o Treat any active cause o Cool compressed during swelling may help to decrease o Steroids usually not helpful o Consult with physician may help to rule out cardiac or renal diseases if suspected o If cosmetically displeasing to patient- VFs and referral t plastic surgeon particularly oculoplastics specialist for blepharoplasty o May need medical consult to determine cause of recurrent edema, i.e. rule out cardiac, renal causes and angioneurotic edema Herniation of Orbital Fat Background o As orbital septum atrophies with age, orbital fat herniates through small dehistences resulting in a soft mass usually located in upper lid medially. It is moveable. Dehistences are cracks or breaks in the tissue lining. o May get referrals to evaluate “tumor” o Occurs in elderly (secondary to weakening of orbital septum- involutional change) and middle aged o Presents as localized (inner canthus) soft, spongy mass within lid, anterior to tarsal plate The skin is smooth Evaluation o Generally easily differentiated from lid or orbital growth (or lid edema) o Pressure to globe results in further herniation of orbital fat in front of the septum. Management o Reassure patient o Cosmetic surgery, if desired o Excision of orbital fat plus blepharoplasty for dermatochalasis if present. Benign Tumors of the Lid Epithelial Origin Papilloma o o o Background A common benign, overgrowth of the epidermal portion of the skin of the eyelid (mainly the squamous epithelium). It is very localized. Can have a vascular core. It is not superficial. There is no ulceration. Benign growths but varied appearance. Vary in color and form Malignancies may look like these but are generally clinically differentiated on appearance May be caused by virus (if so, called verruca); more common in young Can have numerous presentations; can be pigmented, variety of colors Domed, organized Benign when it has hair growing out of it. Types Non-viral Usually in elderly/kids? Viral Verruca- more in adults Verruca is a form of papilloma o Verruca plana- flat top o Verruca vulgaris- angular, raised, broad stalk o Verruca digitala- narrow stalk, cauliflower-like Signs and Sypmtoms Usually asymptomatic Growth o o Viral- fairly quick Non-viral- slow Colors Various colors Surface usually rough (keratinized epithelium) but may be smooth, not eroded, ulcerated. Can be slowly growing, have vascular core, do not usually erode in center. Usually near lid margins at mucocutaneous junction Vascular core- cant see Evaluation Rule out neoplastic growth, if possible, by looking for the following: Look for rapid growth, color change If on lid margin, no cilia at the location Bleeding highly unlikely unless papilloma is traumatized Vascularization- not present on surface of papilloma Surface is often rough but not eroded or ulcerated. Papilloma can occasionally outgrow blood supply resulting in keratinization or necrosis erosion, ulceration. Management Generally no treatment indicated, reassure Cosmetic treatment only if desired (excision) Can produce local lash misdirection and resultant trichiasis Easily excised with scissors if pedunculated. If large or flat, refer for surgical excision. Refer to dermatologist or ophthalmologist if highly suspicious or take photos and foolow up in one month. If new lesion, carefully evaluate for evidence of malignant characteristics; photograph and follow-up in 1-3 months. Note ABCDEs Excision techniques Scissors/scalpel technique o Scissors or scalpel o If base is small, clean area with alcohol wipe o Anesthesize with topical proparacaine for >1 minute o Grasp top with forceps and lift o Cut base with scalpel or scissors o Curved scissors are best o Apply pressure for bleeding o Cover with polysporin ung o Follow up in one day Chemical technique o Clean area with alcohol wipe o Topical anesthetic o Surround papilloma with petroleum jelly o Apply bichloroacetic acid to wooden tip of cotton swab and apply to lesion. o o o o Should turn lesion white immediately, later darkens, scab falls off in about one week. Advise the patient not to rub RTC 1, 3, 5, 7, days If uncomfortable with this, refer out. Verruca (Wart) Background o A papilloma in which papilloma inclusion bodies have been seen in the epithelial cells. Possibly all papillomas are viral in origin- caused by the human papilloma (wart) virus o Viral papillomas tend to occur in children and young adults. o Transmission by direct or indirect contact and autoinoculation. Management o Spontaneous regression is likely- reassure and wait. o Treat any associated conjunctivitis or keratitis with goal to prevent secondary bacterial infection o Excisional biopsy can be performed but can be followed by the spointaneous appearance of multiple viral papilloma o Cryotherapy should accompany excision if viral etiology suspected so it does not grow back Cutaneous Horn or Tag Background o Form of papilloma probably, although may be keratinized Management o Easily excised (see management of papilloma) o May be a precursor to cancer Seborrheic Keratosis Background o Benign, epithelial growth common in middle aged to older (some in children) o Common on trunk, head and back o Can occur on eyebrow and lids (rarer) o Sharply defined, slightly elevated, brown, plastered on lesions, brownish color- like a “brown plaque” on the skin- easily diagnosed o Important point looks like it is tacked on or stuck onto surface of skin. Little invasion into epidermis, none into dermis Significance o Not pre-malignant (actinic keratosis is) Management o Excision if desired o Easily removed for cosmetic reasons By dermatologist, etc because the base is too long Keratoacanthoma Background o Pseudocarcinomatous hyperplasia- benign growth o Exposed usually hairy regions (such as head, face) of skin- also on lids o Middle aged or older, usually 50-70 o Usually Caucasian o Grows rapidly 2-6 weeks then involutes in a few months or year Can ulcerate, fills with keratin, thgen keratin out and hollows o Maximal size usually 1-2cm o Appearance Raised lesion initially- dome-shaped nodule with central core like molluscum contagiosum Has central umbilicated apical region (composed of keratin) in a craterlike excavation. Has elevated rolled borders. Mimics squamous cell carcinoma and molluscum comtagiosum Grows rapidly to 1-2cm with pore expanded to display keratin filled crater Growth stops, keratin plug is discharged leaving a pit. Mimics SCC. o Document and photograph Significance o Spontaneously regresses by involution but very often mistaken for squamous cell. Because of this appearance, usually excised during phase of involutional regression. Management o Reassure o Photograph if unsure and close follow-up o Excision if cosmetically desired Excision should be strongly considered because Most patients prefer not to wait for regression because of the poor cosmesis of these growths BCC and SCC can (rarely) occur along the edges Excision and biopsy (all excised material should be biopsied) is recommended because of resemblance to SCC and BCC. Recurrence Recurrence after excision is rare so if recurrence occurs, it was almost definitely BCC or SCC, not keratoacanthoma Actinic Keratosis Bowen Disease Lentigo Maligna A premalignant Melanocytic Lesions Spreads laterally (not invasive) Requires biopsy Cystic Lesions Epidermal Inclusion Cyst White No transillumination Dermoid Background o Choriostomas, not neoplasms This is normal tissue in the wrong spot o Choriostoma arises during development from location of the lesion o Dermoids are congenital, developmental anomalies o Probably groups of surface ectodermal cells entrapped during development along lines of embryonic closure. Appearance o Tend to be cystic in nature- “dermoid cyst” o Usually superior temporal in location; usually adherent to periosteum of orbit. o Skin slides over surface easily. o Can induce prescription change and in change in lid closure Evaluation o If dermoid is noted look for other congenital anomalies o Goldenhar’s syndrome- dermoids on surface of globe often accompanied by lid coloboma and appendages on ears, nubs especially near the tragus. Management o Can be removes if desired for cosmetic reasons Sebaceous Gland Cysts Background o Cysts in the glands of Zeis (along lid margin) and/or in larger sebaceous glands (near eyebrows) o “Pimples” o Very common o Many possible locations: scalp, face, ears, back, axillary regions Types o Comedo (blackhead) Keratin plaque in follicle o Milia (whitehead) Small whitish, slight elevated, cyst of the pilosebaceous gland On skin of lid, usually in groups Appearance o Painless, benign, slow progression o Firm, rubbery, rounded, often moveable, yellowish or whitish in color o Depth Superficial (epithelial)- tend to be smaller <10mm Subcutaneous (epidermal)- tend to be large <20mm Management o Reassure, benign but can be removed for cosmetic reasons o Excision of superficial cysts- technique Only deal with if near or on the eye. Clean area with alcohol wipe Apply topical anesthetic for about one minute (proparacaine) Incise with 18-27 gauge needle Express contents Apply pressure for bleeding Cover with polysporin ung Followup in one day o Surgical excision for larger, deeper cysts Sudoriferous Cysts Background o Elevated rounded lesions caused by blockage of the gland of Moll (sweat gland) o Common Appearance o May be <2mm in diameter o Localized at lid margin o Usually painless o Usually causes no problems o Cystic nature apparent in indirect/proximal illumination Appears to glow or illuminate Management o Reassurance, benign o Can be excised easily-technique Clean area with alcohol wipe Anesthetize surface for one minute Lance with 18-27 gauge needle Express material Cover with Polysporin ung Follow up in 1 day Syringoma Enlarged apocrine sweat gland. Discrete 1-2mm white nodules Can be removed but remains can enlarge. Common and benign Apocrine Hidrocystoma Normally at canthus Cysts Transilluminate Benign Treat with excision Trichoepithelioma Tumor of hair follicle Mimics BCC Can recur Benign Melanotic Lesions Nevus (Freckle) Background o These are beauty marks. They can be found anywhere on the body. o Overgrowth of melanin-containing cells in skin o Can change with time and remain benign, however change always suggests malignancy o Flat, brownish, well defined borders Types of nevi o Junctional nevi On two surfaces? Flat or only slightly elevated Smooth surface Uniform light to medium brown Symmetrical borders Rarely become malignant o Compound nevi Deeper in the skin. Incorporates different layers of cells Somewhat elevated, more so with age Flesh colored or brown Smooth or warty surface (rubbery) Symmetric, uniformly round or oval o Dermal nevi Raised, dome-shaped. “Pick at it” Brown or black, lighter with age Smooth or warty surface May have telangiectatic vessles on surface Exposed and prone to trauma from clothing o Guidelines for recognition of normal nevi Asymmetrical: symmetric, matching halves if “folded” together; round or oval. Borders: regular, usually quite distinct Color: uniform within lesion, varies from very light brown to black Elevation: fairly flat Remain uniform in size, shape, and color o Kissing nevus Nevus seen on both upper and lower lid at same spot Due to embryology Evaluation o Careful history to document onset and progression o If any doubt, photodocument and follow very closely or better yet get dermatology consult Management o Photograph carefully o Re-evaluate based on degree of suspicion With a suspicious lesion, see every month. If not, 3mo, 6mo, or 1yr. o Only biopsy can definitely rule out melanoma. Any change demands a biopsy. o Refer to dermatologist if its on the body. Refer to oculosurgeon if on the face. Melanosis Oculi (Ocular Melanosis) Background o Increased pigment in uveal tract, sclera o Congenital (within 6 months) o Differentiate from acquired (possibly malignant) melanosis Rule out melanoma, glaucoma Types o Congenital melanosis oculi Increased pigmentation in choroid, iris, ciliary body, sclera, episclera Due to increased number of melanocytes o Nevus of Ota (oculodermal melanosis) Also have increased melanocytes in skin around the eye Can develop malingnant melanoma o Characteristics of these Increased pigment in sclera and episclera Increased pigment in iris Increased pigmet in fundus (choroid) Increased pigment in skin. Management o Evaluate for uveal tract melanomas o Follow up yearly Developmental Vascular Lesions These are benign blood lesions due to dilation. Capillary Hemangioma (Strawberry Mark) Background o Congenital or presenting very shortly after birth 1/3 present at birth Virtually all within 6 months o Very common (most common hemangioma) 1/200 live births Appearance/ Progression o Anomalous knot of blood vessels o Superficial o Can be around face and eyes. o Can enlarge with time o Variable course can increase in size (dilated/ disarray) o Usually spontaneously regress completely (most regression by age 5) o o Produce flat reddish or pink lobulated lesion in skin Color can change when cenous return- straining, crying, lifting (Valsalva maneuvers) can cause redder appearance. Should blanch Types o Capillary- most common Flat, superficial Congenital, early onset o Cavernous Deeper, raised slightly Later onset o “Spider” angioma Not congenital Central core with “spreading effect” Tiny and tolerable o Racemose Grape-like vessel clusters- on retina o “Port wine stain” Hemangioma on one side of face In Sturge-Weber syndrome Conjunctiva/episclera has pink cast Evaluation o SLE Uveal tract. Blood vessels in the angle. Glaucoma? o Slight pressure- easily blanches, rules out nevus, melanoma Digitally for 5 seconds o Look for other congenital anomalies Management o Photodocumentation helpful o Re-evaluate 3-6 months o Refer to dermatologist if cosmetically unappealing to patient (laser therapy is quite effective), however, remember they usually regress spointaneously, but not after adolescence. o If present after adolescence, recommend dermatology referral. Nevus of Ota Oculodermal melanocytosis Xanthelasma Background o Common, slowly progressive skin growth o Develops in 4th and 5th decades o Variable connection with blood lipid abnormalities Manifestation of a genetic dyslipidemia Type IIa: elevated LDL, total cholesterol Types IIb: elevated LDL, elevated VLDL, elevated total cholesterol 50% of patients with xantheslasma have “normal total cholesterol” but LDL is abnormally high, HDL is extremely low. Longevity studies show that xanthelasma with or without hypercholesterolemia is a risk for atherosclerosis-induced mortality Check cardiovascular history o Deposited fat and cholesterol Appearance o Elevated yellowish discoloration of skin. Opaque and matte o Seen bilaterally on medial aspect of upper lid o Plaque-like with a slightly granulated surface o Asymptomatic, benign, of cosmetic concern. Evaluation o Check for arcus o Evaluate patient for other evidence of hyperlipidemia (corneal arcus, cholesterol emboli in retinal arterioles) and evidence of concomitant vascular disease HTN and DM o Also look for obesity o Careful medical history for underlying vascular disease o Careful family history for family history of vascular disease Treatment of xanthelasma o Will not disappear with decreased cholesterol o Reassurance that lesion is benign and non-cancerous o Cousel patient on potential risk of possible underlying systemic disorder o Referral for removal only for cosmetic reasons Surgery Electrocoagulation Chemical cauterization (Bichloracetic acid) o Blood workup to rule out hyperlipidemias, cirrhosis, arteriosclerosis Lipid panel (triglycerides, HDL, LDL, total cholesterol) Blood glucose CBC Malignant Neoplasms of the Lid Basal Cell Carcinoma (BCC) Background o Most common malignat neoplasm of the lids (about 90% of all) o Much more common than SCC o Slowly growing lesion, takes months to double in size. o Usually in area of chronic exposure to sun- lid is not really common compared to other areas of exposed skin. Profile of most susceptible to BCC o Elderly (about 80% >50 yo); average age 60-65 o Usually male (due to more likely long-term chronic outdoor work than females) o Usually light complexion o Red and blond hair have significantly higher risk o Albinos increased risk (rare in Blacks and Asians) o Higher incidence in areas of previous trauma, burns, physical trauma, or x-ray exposure. o Controversial link to irritation caused by spectacles (nosepads) o Chance of second BCC within 5 years is 45% Location of BCC o Lower lid most common (60% of all BCC located on the lids) o Medial canthus; upper lid Appearance o Starts as small translucent, waxy, grayish-white nodule o Classically the center slowly ulcerates with an increase in size- tends to have darkened, ulcerated center (“rodent ulcer”) o Borders tend to be smooth, pearly white with fine telangiectatic vessels. o May have ulcerated center with time o 4 types Nodular (common) Superficial (back and trunk) Sclerosing waxy yellow “scar tissue,” indistinct borders Multicentric type Symptoms o “lump” or “growth” that “doesn’t go away” or “does not heal.” Chances are that it will have been there for a long time. Average 4 years, so long duration does not indicate benign nature. These are slow growing. o Slow increases in size o Does not usually metastasize o If metasiasis occurs (unlikely) it will be the regional lymph node first- palpate preauricular and submandibular nodes for swelling and tenderness Key points in evaluation o History Long term growth on lid (usually lower lid) that wont go away; looks like it is bleeding. Wont heal, etc. History of previous damage to area History of other growths (60% of lid BCC accompanied by another BCC elsewhere) o Gross observation, palpation of lesion. Photograph o Palpation of regional lymph nodes (though it spreads by direct extension, not metasis) Can still cause death by spreading through sinuses and meninges. o Careful SLE o Look for other BCCs If single BCC has occurred, 20% chance of a second within 1 year; after 2 BCCs have occurred 40 % chance of another <1 year. On trunk or back BCC may appear as an erythematous plaque. Management o If in medial canthal region, consider consultation with oculoplastics specialist ASAPmore likely to directly extend intracranially without apparent nature when grossly observing the lesion. o Unsure of suspicious lesion Refer to ophthalmologist (and dermatologist) for biopsy o o Consider dermatology referral- they are much more effective at picking up the other BCCs elsewhere. Surgery excision by Moh’s technique, reconstruction by oculoplastic surgeon, Radiation; cryo, conventional surgery also effective. Legal aspects If patient refuses biopsy- again recommend it and document in charts. Document potential outcome if untreated. Worst case blindness and/or death (rare) o Death due to extension into sinuses. At least take photos and close follow-up every 3 month If apparent growth, referral o Ophthalmology o Dermatology Post-op management Careful q3-6 months follow up by dermatologists for regrowth (recurrence rate 10%) and other BCC OD should carefully evaluate any patient with history of BCC Long term management Annual exams Squamous Cell Carcinoma (SCC) Background o Much, much less common than BCC. Only accounts for 5-9% of malignancy of lids. o Much more rapid growth and can metastasize. Spreads by local invasion and extension into regional nodes. So you need to act very quickly. Need biopsy. Profile of susceptible individual o Elderly, average age of diagnosis about 70yo o Much exposure to sun o Exposure to irritants, chemicals or trauma- radiation, sunlight, thermal burns, chronic heat and/or irritations, organic hydrocarbons o Fair skinned mist susceptible. Location o No typical location, less on lids more on lips (30%) o Often arises from existing actinic keratosis or de novo o Can arise from cutaneous horn o Any areas of trauma Appearance o Various appearance- none is classic for SCC o Can be raised nodule; flat crusty area; flat scaly area; ulcerated bleeding lesion, thickened margins o Can be very keratotic with build up of keratin into a curaneous horn o Numerous benign growths look like it (particularly keratoacanthoma) o Differental diagnosis BCC Actinic keratosis- sandpaper lesions Keratoacanthoma- keratin crater lesions Seborrheic keratosis- mushroom plaque-like lesions Sebaceous gland tumor Management o If SCC is suspected, must refer for excisional biopsy (only definitive method). Refer now and assure compliance. o Clinical evaluation is at best only ~50% correct for diagnosis of SCC- excisional biopsy is only definitive test for SCC and SCC has many appearance so great deal of suspicion is needed to detect early. o Surgical management Excisional biopsy if positive for SCC- Moh’s technique- further excision of borders unil free. Excision until there is no more SCC seen. Normal tissue needs to be seen. Used with chemo/radiation, etc. o Referral- immediate Dermatology Oculoplastics specialist Make sure you keep following up. o Follow up after surgery Recurrence rate of previously excised lesion is higher than BCC (which is very low 10%)- must carefully follow after surgery for recurrence. o Medicolegal aspects- if patient refuses referral Carefully explain it may be cancer, can be treated, must get opinion ASAP Explain potential risk, blindness and or death Make the appointment yourself, hand information (written) to patient Send registered letter to patient and doctor Document your counseling (and information given to patient) in the chart Send registered, return receipt requested letter if does not keep appointment Send second if needed Need to know consequences (LOV, death) Malignant Melanoma Background o Most malignant skin tumor (70% of all deaths due to skin cancer) o Rarely on lids o High rate of metastasis compared to other malignancies o Can metastasize in early stages o Early detection and treatment is critical o Dramatic increase in the past few years o Much less frequent than BCC and SCC but much greater mortality rate Profile of susceptible patient o Those with high amount of sun exposure o Classically elderly, but greatly increasing numbers of middle aged or young get these o Those with fair skin, burn easily o Red hair 3x the risk due to fair skin o Family history important Types o Hutchinson’s Freckle/ Lentigo Malignant Melanoma Hutchinson freckle is a precursor- flat, roughly circular skin discoloration About 5% of all melanomas Large >3cm, flat Usually in elderly Tan to dark brown to black Slowly progressive lesion- darker, larger, more elevated Usually in sun-damaged skin of elderly Least aggressive melanoma; local excision usually successful o Superficial Spreading Melanoma Most common of all melanomas- 70% of all melanomas Flat to slightly elevated Arises from pre-existing nevus Irregular borders; sharply defined borders May have light halo Regression of tumor in one area gives notched appearance Has a pre-existing lesion, starts superficial then after 1-7 years- good prognosis if removed while superficial. o Nodular Malignant Usually in elderly About 15% of all melanomas in US Often from uninvolved area- no pre-existing lesion Elevated, dark colored, sharply demarcated Dark brown, red brown, red black Possibly misdiagnosed as blood blister, hemangioma Metastasizes early- poor prognosis Most important factor is change over time. If patient complains of change in nevus looking growth get a dermatology consult now. Adenocarcinoma of Meibomian Gland Background o Adenocarcinoma of meibomian glands (a sebaceous gland carcinoma in meibomian gland) o Very rare o Arises from meibomian glands o Very invasive and can rapidly invade the orbit o Also likely to metastasize as much as 1/3 have metastasis to orbit Management/ Recognition o Can mimic chalazion (BCC) o An enlarging chalazion- refer for excision- biopsy o Recurrent chalazion- refer for excision biopsy. Considerations for recognition of malignant growths Fair skin patients, patients who easily burn Patients with excessive sun exposure due to job, recreation, etc. Middle aged and elderly Patient history of skin cancer Family history of skin cancer History of malignancies elsewhere Rapid growth of lesion (growth of what has been a quiescent lesion) Ulceration of center of lesion/ erosion at the margins of lesion Bleeding from lesion which has not been traumatized Pain/ irritation at site of lesion Recurrent inflammations or irritation at the site Unpredictable changes/ irregular changes Bacterial Infection and Inflammation Hordeolum Background o Acute staphylococcal infection of the various glands of the lid margin o Type of hordeolum External More superficial glands which are anterior to tarsal plate- gland of Moll or gland of Zeiss and associated follicle Leaves no problems Seen with manipulation of lids Arises quickly Internal Meibomian gland is infected by staph Arises over time (1 week) Resolves 7-10 days More involved (tarsal plate)- can cause lasting problems o By far the most common cause is staph (pyogenic, suppurative) Pus formation is common o Predisposing factors Staphylococcal or mixed blepharitis Meibomitis Poor lid hygiene Poor diet (increased fats, oil, alcohol) Poor general health Stress, fatigue Diabetes (because it disrupts the immune system) Chronic illness or immunological compromise Medication (Antibiotics/ antidepressants) External Hordeolum o Background Commonly called a stye by patients Very common lid disease o Etiology Staph inflammation of glands associated with hair follicles of lid margins gland of Zeiss or Moll o o o Very often there is concurrent staph blepharitis, blepharoconjunctivitis or keratitis Clinical presentation Signs Will present with signs of acute inflammation: redness, heat, pain, swelling, etc. Purulence will develop quickly producing local yellowish point o Looks like a white/yellow head Symptoms Localized redness, painful area on lid margin which will “present” in a short period of time. This pointing area is basically an abscess- localized inflammatory debris with much pus The abscess will generally drain in <1 week, hot compresses speed this Adjacent follicles may become involved Onset is fairly fast, about 1-3 days o Leaves quickly too (no residual problems) o Severity = 2 Clinical Evaluation Usually easily differentiated from growths and other infections by its localized nature of acute inflammation. External- “points out.” Palpate the lid to determine localized nature (and sensitivity) Carefully evaluate for other forms of staph anterior segment disease and treat these concomitantly. Differentiation of external from internal is important Watch for developmet of preseptal cellulitis- very uncommon Check lid for diffuse inflammation, check regional lymph nodes carefully and follow up every 3 days or less. 30% chance of preseptal cellulitis with internal hordeolum, 2-3 days later. Much less risk with external hordeolum. Preseptal cellulitis may occasionally occur with staph bleph. Management Warm compresses are primary therapy for all hordeola Increase blood flow to area Increase enzyme activity and resolution of hordeola 5-10 minutes; minimally qid or more frequently o Increase frequency means the faster it will go away. o Heat kills bacteria o Dilation of blood vessels brings increased white blood cells Small hot water bottle, heat comfort, warm hard-boiled eggs, wet washcloth heated in microwave oven. Soak cotton balls in water. Topical antibiotics Ineffective in directly affecting an hordeolum Antibiotic ointment to reduce spread of microbes o More for external than internal hordeola o Bacitracin or erythromycin ung, bid to qid for 10 days. ¼ inch This works well for G+ and is inexpensive. Erythromycin, a macrolide, po gt, or ung. o This is more for external hordeola Antibiotic drops for conjuncitivitis o Accompanying bacterial conjunctivitis o Secondary conjunctivitis from pus drainage o Gentamicin gtt qid, norfloxacin or tobramycin gtt qid x 10 day o More for internal than external hordeola Value is more prophylactic than directly theraqeutic o Prevents secondary infection. Oral antibiotics Radical treatment uses oral antibiotics for all internal horedola; conservative use would be for hordeola resistant to standard therapy (not external), Must use preseptal cellulitis Dicloxacillin 250mg, po, qid (penicillinase-resistant penicillin; most specific for staph) x 10dy o Pus/ Staph can be resistant Erythromycin 250-500mg po, qid, or EES 400-800mg, qid x10dy Tetracycline 250-500mg, po, qid (tetracycline best when used early in process, within first two days of symptoms; much less effect if hordeolum is moderate to large in size) x 10day. Very inexpensive and readily available. Range of doses depend on patient’s age, weight, and severity of condition; use 7-10 days (10 days preferred) Unlikely to be used for an external hordeolum. Time framework Externals resolve in less than one week Internals resolve in 7-10days or sooner Use topical antibiotics for at least one week Consider oral antibiotics or culture and sensitivity if not resolving or patient is not compliant Use oral antibiotics for 7-10days. Treatment of underlying concomitant staphylococcal blepharitis Strong likelihood that staphylococcal activity is present No standard lid hygiene until hordeola resolved Use appropriate antibiotic ointments, after the hordeolum is resolved Lid hygiene (after hordeolum resolved) daily or every other day for prophylaxis Antibiotic ointment qhs first five days of each month Modify lid hygiene if meibomitis present or unresolved hordeolum becomes a chalazion “Drastic” measures- not recommended Epilate lash to start drainage channel (for external hordeola) Loosen dried plug at involved meibomian gland orifice (if present) with spud, begin drainage with gentle pressure (for internal hordeola) Use stab incision cautiously for internal hordeola (try other therapies first) Internal hordeolum o Background Etiology: staph infection of meibomian glands accompanied by blockage of the gland. Longer to develop (3-5days) and resolve o Evaluation: as for external hordeolum Evert lid- circumscribed tender, red elevation; may see purulent exudates o Progression to preseptal cellulitis Watch very carefully for preseptal cellulitis Palpation- diffuse tenderness Observation- diffuse redness Nodes- tender, palpable Symptoms o Tons of pain o Large amount of heat o More diffuse/ global o Within the area of the glasses. o Can leave lasting problems o Severity 5-6 About 30% chance of preseptal cellulitis Tends to be more slowly progressive, onset over 3-5days. Resolves longer o Management aspects Use warm soaks/hot compresses as much as possible- typically effective (at least qid) Topical antibiotics do not penetrate the meibomians, though are useful for blepharitis If resistant, use oral antibiotics (see above) Rarely need surgical intervention to drain; incision may cause preseptal cellulitis Treat concomitant blepharitis or other staph related or seborrhea related disorders. RTC 48 hours; if worse, culture and sensitivity to rule out preseptal o Resolution Slower than external, usually 7-10days. Chalazia Background o Classically, a chronic inflammation of meibomian gland; may involve gland of Zeis also (?) “Sterile,” classically unrelated to microbial activity; synonym for classic/sterile” chalazion is “primary chalazion.” Here there is no infection. Chalazia related etiologically to Primary meibomitis Rosacea Previous internal hordeolum, without total resolution (synonym is “secondary chalazion”) Lump of lipid retained in meibomian gland Too large to be consumed by macrophages Encircled by leukocytes and walled off by fibroblasts Also known as lipogranulomatous lump o Various sites of involvement in the meibomian gland Remains contained within the tarsus Breaks through tarsus Breaks through posteriorly (internal, meibomian gland) Breaks through anteriorly (external, gland of Zeiss) Marginal chalazion: small, near lid margin; not deep enough or large enough to promote tissue reaction. Clinical Presentation, Signs and Symptoms o Slowly growing mass Early stage: firm, moveable pellet under skin Without obvious lid swelling Not identified unless lid is palpated Later stage: visible lid swelling, without erythema o Upper lid involved more than lower lid o More frequent in adults than in children o Symptoms are fairly mild No pain, unless from unresolved internal hordeolum Some discomfort or pressure on globe. Cosmetic disfigurement, so they want it removed. Visual distortion due to lid mass (astigmatism) Not red, hot, painful, because it is not an infection o Appearance of lid and palpebral conjunctiva Early stage: without visible lid swelling Sac-like swelling on palpebral conjunctiva Soft, fluid-filled, boggy Later stage: firm, palpable mass Yellow tissue mass protruding through tarsus Large mass with overlying normal or hyperemic conjunctiva o If chalazion is the result of an unresolved internal hordeolum, may have more pain than usual. Treatment o Standard regimen of Warm compresses as frequently as possible Digital massage (after warm compresses) of the lump as much as possible o Saline soak regimen Cotton balls soaked in warm saline ½ teaspoon sale to 1 quart water Soak for 10 minutes at least bid Follow by digital massage. This holds heat longer and has an antiseptic property o Try either regimen for 2 weeks If improiving, maintain for another two weeks to hopeful resolution If not improving, consider steroid injection or surgery o o o o o o Rule of 6s <6mo, do warm compresses 6mo, steroid injection >6mo, or >6mm, do surgery Antibiotics are variable. This is not an infection, only give with a concomitant condition Little or no microbial activity in chalazion Tetracycline for underlying primary meibomitis and/or rosacea Tetracycline can often clear an unresolved hordeolum which remain inflamed while progressing into a chalazion or a chalazion (formerly a hordeolum) which becomes reinfected (1-2gm/day, 3-4 weeks) Intralesional steroid injections Right into the lesion. Q2wk 2-3x Triamcinolone (Kenalog) 10mg/ml, diluted to 5mg/ml Inject up to 0.3ml into lesion; average about 0.15ml Use 25-27 gauge tuberculin syringe, 5/8” needle Steroid suppresses both chemotaxis of inflammatory cells (swelling) and fibrotic cells (hardness) Works best when chalazion is “young” (<6 months) Should be tried on large or hard chalazia Indicated when chalazion is near lacrimal ducts Aqueous preparation better than crystalline suspension since risks of hypopigmentation and skin atrophy are reduced. Inject trans-conjunctivally rather than trans-dermally. With no resolution, go to surgery Surgery If 1-2 months of warm soaks or 2-4 weeks of injections are unsuccessful, perform surgery Surgical removal of palpebral conjunctival side Surgical remocal from external lid side Multiple recurrent chalazia at the same location are highly suspicious for meibomian gland carcinoma; must obtain consultation for excisional biopsy. Future management Identify and manage dermatologic conditions Rosacea Sebborheic dermatitis Control primary meibomitis Chalazion Removal Chalazion Therapy- Noninvasive Options o Do nothing- 25% success rate o Warm compresses, lid massage o Topical antibiotics o Systemic antibiotics Chalazion Therapy- Invasive Options o Intralesional steroid injection Procedure Anesthetic injection first o o o Lidocaine 2% Along with epinephrine because it vasoconstricts to maintain it at that site. Side effect of increased heart rate, etc. 0.1-0.2ml of triamcinolone acetonide 10mg/dl (Kenalog-10), shake well, because it is a suspension Fine needle 25-28 gauge Inject into lesion (capsule) F/U in 2-4 weeks 2nd injection if no reduction Effectiveness About 60% cure on 1st injection About 80% after 2nd injections Therefore, doctors prefer surgery, because it is 100%. Incision and curettage- 67800 Patient education Discuss nature of chalazion Discuss all treatment options Discuss risks of option selected o Failure to remove complete chalazion o Infection- preseptal cellulitis o Scar formation/ contraction- entropion, deformed lid Minimize with vertical cut and cut on side of conjunctiva o Risks of meds Topical anesthetic Allergy, dermatitis, tissue necrosis Toxicity: drowsiness, dizzy, nausea, tingling Lidocaine/ epi and subconjunctival intralesion Epinephrine (in injectable anesthetics) o Cardiovascular risks increased heart rate and blood pressure hypertensive crisis, cardiac arrest Steroids can cause depigmentation Patient preparation Patient reclined Prepare syringe: lidocaine/ epi o Around and in lesion Instill 2 drops tetracaine or proparacaine Inject ½ - 1ml of lidocaine/ epi subcutaneous via 28-29 gauge needles Chalazion Incision Apply chalazion clamp with the chalazion centered Tighten clamp to stabilize and achieve hemostasis and the flip Use #11 blade Make incsision in conjunctiva parallel to the orientation of the meibomian glands Stop >2mm frin lid margin Do not approach lid margin or puncta o Use curette to sweep all granulomatous material out through incision Blot with sterile q-tips Cauterize bleeders Immediate Post-procedure care Apply broad spectrum antibiotic ung, prophylactic Reapply ung qhs and remove patch Non-aspirin analgesics (possibly vicodin, etc) Advise follow-up in one day Advise patch removal tomorrow am at latest, then reinstill antibiotic ung One day follow-up Most important- ensure no evidence of cellulitis, treat with oral antibiotic if so. Which option to select? Doctor’s personal preference May consider steroid injection if Patient preference Small (<8mm) diameter lesion Close to lid margin, puncta, or lacrimal drainage system Newer, softer chalazion Patient is child Cutting is generally better, but increased healing time. Don’t use incision or steroid if Hot lid- acute inflammation o Probably not a chalazion. o Can cause infection to spread, causing orbital cellulitis Preseptal Cellulitis Background o Inflammation of lid structures anterior to the orbital septum (anterior to the orbital rim) o Same symptoms of internal hordeolum, but magnified o Caused by Facial infection: sinusitis, dental infection, soft tissue infection (H. flu in kids, Staph in adults) Blunt or penetrating trauma to lids (Strep) Eyelid infections (Staph) Internal hordeola: 30% chance Acute staphylococcal blepharitis Sinusitis is the most common cause of preseptal cellulitis o Limited to preseptal area by anatomical barriers o Common microbies H. flu in kids (likeliest, but not in every case) Staph and Strep in adults are likeliest microbes Signs and Symptoms o Diffuse, painful swelling of lid tissue, but no proptosis o Pain and tenderness may radiate past the orbital rim o o o o Pre-auricular (and submandibular) lymph nodes may be tender Vision usually affected EOMs normal in preseptal cellulitis; eye movements not painful; no diplopia Addociated findings Hordeolum is a focal point of increased tenderness Scaling, SPK suggested staphylococcal blepharitis History of trauma History of other infections (sinusitis, etc) Ache in sinusitis Ethmoiditis: retrobulbar ache or orbital ache Frontal sinus: headache Maxillary sinus: ache in cheeke or teeth o Orbital cellulitis: differential Here the whole upper lid is swollen Risk of permanent vision loss (optic nerve) Risk of loss of life if infection gets into the cavernous sinus and meninges Preseptal cellulitis can worsen into orbital cellulitis if inadequately treated Causes of orbital cellulitis Sinusitis (most common cause in kids) Ethmoidal wall fracture or other trauma Dental surgery Bacterial infection elsewhere (such as preseptal cellulitis) Most common organisms involved in orbital cellulitis (as with preseptal cellulitis) o H flu is #1 in kids o Strep and Staph in adults Multiple signs in orbital cellulitis Early diagnostic sign: conjunctival hyperemia and chemosis (moderate to severe); these frequently preceded proptosis and diplopia External ophthalmoplegia o Restricted EMOs with H-test Optic never edema and eschemia, with variable/ mild VA loss o Positive APD Pain on eye movement Diplopia Lid edema, erythema, possible proptosis More often unilateral Elevated WBC count to fight the infection General malaise: fever, chills, vomiting (patient really feels sick) Emergent referral for treatment which involves hospitalization, culture and sensitivity; medications may include ampicillin, IV chloramphenicol, fluoroquinolones, cephalosporins. Treatment o Oral antibiotics for 10-14 days If likely caused by staphylococci Dicloxacillin 250mg, po, qid Cephalexin or cephradine, 250mg, po, qid o o o Erythromycin 500mg, po, qid or EES 800mg, po, qid (penicillin-allergic) Amoxicillin, clavulanic acid (Augmentin) is excellent, but very expensive o 250mg, po, tid o Can get generic May use lower doses with kids (talk to pediatrician) If likely caused by Streptococci Penicillin G 125-250mg, po, qid First generation cephalosporin: cephalexin (Keflex) or cephradine, 250mg, po, qid Amoxicillin 250mg, po, tid or ampicillin 250mg, po, qid If likely caused by H flu Amoxicillin 250mg, po, tid or ampicillin 250mg, po, qid (amoxicillin now preferred drug over ampiciliin) Amoxicillin and calvulanic acid (Augmentin) 250mg, po, tid (great medicine, but expensive) Second generation cephalosporin, Cefaclor (Ceclor) 250mg, po, tid or cefuroxime axetil (Ceftin) 250mg, po, bid (also great, but also expensive) Range of doses depends on patient’s age and weight Warm compresses as much as possible Prophylactic gentamicin or norfloxacin drops qid and/or Polysporin ung, bid Follow-up In 1-2 days condition should not be worsening If no better in 3-4 days, get culture and sensitivity STAT and consider orbital cellulitis Impetigo Background o Skin infection by staphylocco or group A streptococci (staph is the likeliest cause, group A strep less common) o More frequent in newborns and children than in adults. Worsened by poor hygiene Very contagious among children o Occurs in warm weather (typically summer) Signs and Symptoms o Exposed areas are most affected Face, arms and neck May involve eyelids secondarily o Pathogenesis Lesion begins as a macule (flat red skin spot) Develops into a vesicle or pustule Lesions rupture, then ooze Organism on skin with scratching, it penetrates Fevers, because it elicits immune response Involves lymph nodes o May have regional lymphadenopathy o Lesions do not scar o Two types Bullous: larger blistered areas with or without superficial crusts; caused by Staph Vesicular: smaller vessibles, typically with honey-colored crusts; caused by Staph and/or Strep Treatment o Topical therapy Used alone, this is not enough. Older, more traditional therapy Lesions must be debided to expose bacteria, otherwise topical antibiotics are ineffective. Regimen Soak with Burow’s solution for 20 minutes, bid to qid. This is an antiseptic and astringent Burow’s solution (aluminum sulfate, calcium acetate) available in Domeboro Powder Packets (OTC); one packet to one pint of water is 1:40, two packets gives 1:20 concentration Soaking softens crust and has astringent action; skin appearance improves after soaking. Follow soaking with gentle debridement of crusting with a wash cloth Chlorhexidene solution to further cleane area (Hibiclens solution, 4 or 8 oz, Rx) aka Heavyclens o This can sting After dying, apply topical antibiotic ointment (Polysporin or erythromycin) without covering bandage. o This would incubate the bacteria. Contagious: do not share washcloth with the family New drug: mupirocin (Bactroban) 2% ung; used tid; effective against both Staph and group A Strep; by Rx only; effectively replaces all older topical antibiotics o Systemic therapy This is required Cephalosporin: Cephalexin (Keflex) 250mg, po, qid or Cefaclor (Ceclor) 250mg, po, tid; should cober both group A Strep and Staph Dicloxacillin, 125-250mg, po, qid x10 days (Staph) Penicillin V, 250mg, po, tid-qid x10days (Strep) Erythromycin 250mg, po, qid or EES 400mg, po, qid x 10day (for PCN-allergic patients) More effective than topical therapy Blepharitis There are two forms: Meibomian Gland Dysfunction and Anterior Blepharitis. One form is rarely independent from the other. These are also associated with dry eye syndrome. The reduced lubricity of a thinned or mucindeficient tear is unable to buffer the ocular surface from the shear forces of the blink. This causes abnormal sloughing of the epithelial cells as well as ocular surface irritation and inflammation. Staphylococcal Blepharitis Background o Staphylococcal organisms are ubiquitous. They never go away. Staph epidermidis frequent in blepharitis Staph aureus less frequent than Staph epidermidis Staph saprophyticus very infrequent in blepharitis o Staphylococci are colonized on lid margins Episodes erupt when environment changes Illness (acute or chornic) Medications (antibiotics and steroids) Poor hygiene and nutrition Staphylococci blepharitis is usually chronic. It never goes away completely Due to ubiquitous nature of Staph Waxing and waning presentations Permanent structural changes due to chronic damage by staphylococcal exotoxins Sudden exacerbations, awakening with painful lids, trauma, URI, otitis media (ear infection) Signs and Symptoms o Crusts (pathognemonic) that strongly suggest staphylococcal exotoxin activity Ulcerative (synonyms: rosettes, collarettes) Round, hard, yellow Firmly bound down at base of lashes Ulceration underneath when crust removed Fibrinous (synonyms: brittle, “impaled cornflake”) Represent fibrin exuded from damaged tissue Scale starts at base of lash, then grows with it away from lid margins (lash in the middle) Often called “squamous,” though “swuamous” means scaling, which is common to both seborrheic and staphylococcal processes o Lid characteristics Erythema Diffuse redness along lid margin from acute inflammation Chronic neovascularization on margin Deeper permanently engorged vessels Puffy from fluid accumulation Tender to palpation Acute changes due to hypersensitivity o Keratitis Due to pooling to exotoxins in tear lake SPK in inferior third of cornea Also due to lipases breaking lipids into surface-active free fatty acids and from poor blinking Long-term: marginal infiltrates, ulceration, pannus o Permanent structural changes All changes due to exotoxins damaging tissue Madarosis (missing lashes) Poliosis (white lashes) due to inflammation Tylosis (thickening) Trichiasis (misdirected lashes) Lid neovascularization Glomerular fronds of vessels at margins Deeper vessels causing a pink “cast” Possible excoriation at external canthi Tissue breaks down o Hypersensitivity reactions to staphylococcal exotoxins Phylectenule Beefy hyperemic conjunctiva adjacent to corneal involvement Marginal corneal infiltrates o Staphylococcal crusting can be mixed with other presentations of blepharitis Crusting may be predominantly staphylococcal May be mixed with seborrheic types Scurf Foamy, greasy scales May be present simultaneously with meibomitis o Symptoms multiple symptoms, varying on severity of staphylococcal activity and damage to tissue FBS, grittiness Stinging, burning, irritation Pain Tender lids Possible itching Frequent hordeola Variable depending on time of day Bimodal- two points of the day that affects the patients the most. Worse upon awakening o Buildup of crusts during sleep o Exotoxin-caused SPK during sleep. Worse at end of day o Dry eye symptoms o Increasingly poor TBUT Treatment o In practical terms, “staph blepharitis” is rarely a purely microbial condition but is a combination of sebborheic (greasy) processes with microbes. Treatment begins with assessment of both the immune/ hypersensitivity process (not well understood presently) as well as the microbial process (staph, exotoxins, free fatty acids). Assess the severity of the immune process by the degree of pain, tenderness, redness, and swelling (all signs of inflammation) Assess the severity of the microbial process by the amount of ulceration, crusting, permanent structural damage, and FFA activity (keratitis). o With the patient in the chair, remove as much of the scaling as possible with wet or dry q-tip, tweezers, or epilating forceps (you can do it better than the patient can). Some o o o will additionally locally treat the lids with a strong antibiotic one time only (i.e., Ciloxan or other quinolone drops on a q-tip). This is not mainstreams. It is more esoteric. Steroids These are used with antibiotics. They calm the inflammation so you can use lid scrubs. Only use in those with extreme pain. Necessary with moderate to severe immune processes Necessary to reduce significant erythema Necessary to reduce pain and tenderness Useful to promote subsequent successful lid hygiene Blephamide (also Metimyd, etc): sulfacetamide 10% with varying concentrations of prednisolone acetate Cortisporin Big guns: Pred-G, Tobradex, Maxitrol (use these with a severe immune reaction and/or the need to use aminoglycosides in case of resistance). Never use long-term Beware of hoarding for later use Apply ointment on q-tip or finger to lid margins, bid-tid, to reduce pain and redness; use no longer than 7 days to avoid tapering and risk of rebound. Lid inflammation is very responsive to steroids, even the “weaker” ones. Lid hygiene These are most important Remove crusts which harbor and shield bacteria Remove extra grease which enhances bacterial growth and FFA production Soak lids first with warm washclothe Softens and loosens crusts Speeds blood supply Hygiene “recipes” Varying concentrations of baby shampoo to water 50:50 on q-tip 1:10 or more dilute for washcloth, cotton ball, or cotton pad Prepared lid cleaners (Eye-scrub, etc) Remove crusts as much as possible before applying using any antibiotic ointment Use hygiene gently but thoroughly if lids are tender Antibiotic ointments for staphylococcal blepharitis Ointments preferred over drops in lid disease To suffocate the bacteria Bacitracin Excellent antibiotic against staphylococci Quite non-toxic Little hypersensitivity or resistance Available in oiuntment only Forms available o Polysporin (bacitracin and polymixin B) o Bacitracin oiuntment (generic) o Neosporin ointment (baciracin, polymixin B, neomycin) o o Erythromycin Good antibiotic against staphylococci Ointment only for topical ocular use Little toxicity to tissue or hypersensitivity reactions Staphylococci unfortunately becoming increasingly resistant Sulfacetamide Considerable resistance of staphylococci, particularly in chronic conditions Poor choice Widely used o Plain or combined with prednisolone Only use with a steroid. Ineffective alone o Risk of overuse, with further resistance of staphylococci Aminoglycosides Neomycin o Risk of delayed hypersensitivity reaction (about 5%) o Risk of cross-resistance to stronger aminoglycosides with overuse of neomycin o Increasing resistance of staphylococci to neomycin o Simply not a good choice for blepharitis Gentamicin o Very good against staphylococci at present o May be necessary to use gentamicin if condition is severe enough or if culture and sensitivity indicate o Should never be used long-term Tobramycin o Very good against staphylococci o Must primarily reserve it for keratitis, due to its effectiveness against Pseudomonas aeruginosa Antibiotic ointment regimens At least bid (one of the two applications should be qhs) When blepharitis is quiet and controlled, use alternating ointments (bacitracin and erythromycin) the first five nights, qhs, of each month. Keep lid hygiene incorporated in their day. AzaSite (Inspire) Azithromycin 1% This is a topical drop that is good for patients who may have less inflammation of the ocular/lid surface, but obviously abnormal lipid secretion. A gel-forming and lipophilic. Remains on the ocular surface longer than conventional drops Anti-inflammatory effect Effective in reducing inflammation and modifying lipid production. Once a day between 14-28 days. Sig: one drop after lid hygiene at bedtime and rub the solution into their lashes for 2-4 weeks. Oral antibiotics for staphylococcal blepharitis o o o Valuable when Blepharitis seems unusually severe Patient is unable to comply with ointment and lid hygiene procedures Patient has a systemic illness Usually not the first choice of treatment Appear to inhibitbacterial lipase production. This reduces the free fatty acids, which helps to lessen inflammation and symptoms of irritation. They also inhibit keratinization of the meibomian glands. Dicloxacillin 1gram/day, 4 divided doses, x7-10 days Should be quite effective for antimicrobial action Tetracycline 1-2grams/day, 4 divided doses, x7-10 days Watch contraindications for tetracycline o Kids under 12 years of age o Pregnant or lactating females o Known hypersensitivity to tetracyclines o Dietary restrictions May be more effective against FFA activity than against microbes directly. Doxycycline 20-50mg bid for a 2 month course. Minocycline 50mg once a day Erythromycin Base, estolate, or stearate: 1-2 grams/day, 4 divided doses, x7-10days Ethylsuccinate 400-800mg, qid (at least GI irritation) For kids under 12 or penicillin-allergic patients Doses of oral antibiotics depens on patient’s age, weight, and severity of condition (1 vs. 2 grams per day) If considering using oral antibiotics, consider sulture and sensitivity testing (best oral or topical to use) and choose least irritating oral antibiotic Testosterone 3% cream, bid To treat any hormone imbalances Omega-3 Fatty Acid Supplementations/ Flaxseed Disrupts inflammatory channels (cytokines) Encourages the production of anti-inflammatory prostaglandins and modifies the composition of meibomian lipids. 1-2 grams/ day 4g a day prescription (Lovaza, GSK) Initial aggressive treatment is mandatory Lifetime condition with lifetime treatment and management; daily or every other day lid hygiene without let-up; alternate antibiotic ointments (bacitracin, erythromycin) first five nights of every month, qhs. Permanent lid structural changes are deleterious Poor corneal resurfacing from irregular lid Reduced TBUT from exotoxins, bacterial lipases, and poor blinking Chornic reservoir of staphylococci o Flare-ups of blepharitis o Flare-ups of conjunctivitis o Possible horedola Marginal corneal infiltrates o Risk of marginal ulcerations o Peripheral corneal scarring, pannus Patient education critical Must manage concurrent seborrheic blepharitis and meibomitis Considerable failure of therapy due to chronicity, patient frustration, and premature discontinuation of therapy Seborrheic Blepharitis Background o Seborrhea is a disorder of sebaceous gland function Overproduction of secretion Disorder of retention of secretion Unknown etiology o Seborrhea (excess oil production) results in Dermatologic conditions Rosacea Seborrheic dermatitis Seborrhea sicca (dandruff) Acne juvenitis (vulgaris) Ocular conditions Seborrheic blepharitis Meibomian gland dysfunction Ocular rosacea o Frequent occurrence of seborrheic blepharitis with dermatologic conditions Seborrheic dermatitis Rosacea Uncertain connection with acne juvenilis o Frequency of presentation Increased frequency in older patients Likely since rosacea and seborrheic dermatitis are common in older patients Not limited to older patients May occur more often in patients with Poor nutrition Poor hygiene Seen in a wide variety of patients o May overlap with other types of blepharitis Staphylococcal blepharitis Meibomian gland dysfunction May be present by itself without overlap Signs and Symptoms o Scaling patterns in seborrheic blepharitis Greasy scales Foamy-looking Irregularly shaped At bases of lashes or spiraling around lash Scurf Called “dandruff-like scales” Probably derived from scalp dandruff Confused with fibrinous scales in appearance o Staphylococcal scales are impaed on lash o Scurf simply stick to greasy lashes o Lid margin involvement Simple seborrheic blepharitis has little effect Lid margin hyperemia due to Neovascularization from chronic staphylococci Markedly inflamed meibomian glands Ocular rosacea (marginal telangiectasias) Lid swelling to Staphylococcal involvement o Short term: edema, hypersensitivity o Long term: tylosis Meibomian gland involvement o Inspissations of secretion o Inflammation surrounding orifices In summary, changes in lid margins are primarily due to either staphylococcal and/or meibomian gland disorders, not to simple seborrheic processes. o Symptoms depend on other concurrent processes Degree of staphylococcal involvement Irritation, stinging, burning Keratitis Tear film disruption from exotoxins and bacterial lipases Lid edema and tenderness Degree of meibomian gland dysfunction Disruption of normal tear film (dry eyes) Stinging, burning, itching, FBS Degree of seborrheic scaling Scurf frequently asymptomatic Mild scaling frequently asymptomatic o Moderate to heavy scaling asymptomatic or symptomatic o Complaints of “mattering” in the morning o Complaints of removing crusts in the morning o Never “glued together” in the morning Treatment o Primary consideration: evaluate any staphylococcal involvement If staphylococci are inadequately managed, consistent risk of exacerbations and chronic damage. Must evaluate degree of staphylococcal involvement by Symptoms suggesting staphylococcal activity o o o o Crusts suggesting staphylococcal activity Structural changes from chronic staphylococci If staphylococci are active, must have aggressive treatment of blepharitis Secondary consideration: rule out dermatosses Examine area other than eyelids Facial blush areas Nose Scalp Retroauricular area Seek dermatologic consultation Dermatologic management of dermatoses concurrent with ocular management Seborrheic dermatitis (shampoos) Rosacea (tetracycline, Metro-Gel) Seborrhea sicca (shampoos) Tertiary consideration: rule out meibomian gland dysfunction May overlap with seborrheic belpharitis Manage with lid massage, etc. Lid hygiene critical for seborrheic blepharitis, bid Warm soak initially to soften and loosen crusts Very dilute baby shampoo solution Ten drops in a juice glass of water Possibly use 50:50 dilution on cotton tipped applicator if patient has the necessary dexterity. Solution on o Washcloth folded into quarters o Wascloth wrapped around index finger o Cotton ball or cotton make-up removal pads Must judge manual dexterity and understanding of patient Regimen of lid hygiene At least once daily, better in the morning when overnight build-up is the heaviest. Preferable twice a day I-Scrub, OCuSOFT, and OcuClenz solutions Very hypoallergenic and gentle Special gauze pads with less abrasion Manufacturers claim significant toxic of baby shampoo solutions compared to theirs Quite costly High cost may be either prohibitive or could promote better compliance. Thorough diagnoses alter treatment plans Staphylococci present simultaneously with sebborheic blepharitis Steroid/ antibiotic ointment only if needed Lid hygiene and antibiotic ointment Culture and sensitivity if warranted Meibomian gland dysfunction occurring simultaneously with sebborheic blepharitis o Lid hygiene Gland expression and lid massage Dermatoses occurring simultaneously with seborrheic blepharitis Dermatologic diagnosis andmanagement Lid hygiene Management “simple” when the seborrheic blepharitis is uncomplicated. Management more complex and multifaceted when seborrheic blepharitis is complicated by staphylococci or dermatoses If treatment is not working, consider non-compliance and need for culture and sensitivity testing. Chronic condition Staphylococci are ubiquitous; must control long-term to avoid exacerbations and to prevent permanent damage. If uncomplicated seborrheic condition, hygiene can be done on a maintenance basis for prophytlaxis Considerable failure of therapy due to no cure, patient frustration, and noncompliance. Meibomian Gland Dysfunction/ Meibomitis Background o Called “posterior blepharitis” Involvement posterior to gray line May co-exits with anterior blepharitis Wide range of presentations and symptomology Significant build-up of fatty esters Some suggestions that condition is exacerbated or caused by diet (elevated cholesterol) Focal drop out or atrophy of the meibomian glands leads to lid margin edge changes, which include dimpling, rounding and change in contour. o Most common form of lid margin disease. 40% of routine eye care patients 50% of contact lens wearers o Anatomy and normal function Pilossebaceous glands Normal secretion should be Clear or very minimally cloudy Consistency of motor oil Normal amount of secretion Maintains stability of tear film Too much causes unstable tear film Too little allows aqueous evaporation o Mechanism of dysfunction Cells slough off from epithelium lining tubule Masses of cells form an obstructive mass over the glands As secretion stagnates, it Initially is cloudy while remaining liquid Later becomes creaky Finally becomes cheesy As tubule and orifice become stenotic, flow is minimized and becomes filamentary o Three types of Meibomitis Meibomian seborrhea Mild, Stage 1 o Often missed. Must push on lids to see secretions. Secondary meibomitis Moderate, Stage 2 Primary mibomitis Severe, Stage 3 o A cystic problem. Nothing expressed. o As dysfunction worsens, discharge becomes abnormal Increased secretion (mildest form) Increasing cloudiness Creamy Cheesy Filamentary Non-existent Signs and Symptoms o Meibomian seborrhea Name means “excessoil oil from miebomian glands Easiest to overlook inless glands expressed Signs Frothing of tear film at outer canthi Papillary conjunctivisit Bulbar conjunctival hyperemia Retention custs and concretions Excessive secretion from glands TBUT variable; may be reduced Gland orifices and lid tissue are normal Oil slick in tear film. The Marx line can become scalloped and irregular. Soapy-looking bubbles. The saponification occurs when excess lipid secretions react with protein in the tears Meibography o Done via transillumination. o Useful for evaluating meibomian gland morphology and density o A common technique is to visualize the central 10 glands on each lower lid, counting the how many are present and how many have “dropped out,” meaning they aren’t visible and aren’t functioning. o The more glands that have dropped out, the less able the lid is to secrete lipids adequately enough to maintain tear film stability. Symptoms o o Extreme range from asymptomcatic to very severe: symptoms frequently overwhelm signs. Hyperemia (“my eyes are always red”) Stinging, burning, non-specific irritation Stabbing pain (“stuck with a needle”) Photophobia Mimics of dry eye symptoms (FBS, etc) Dried oil at canthi upon awakening Secondary Meibomitis Increasing stagnation of secretion Inflammation existing concurrently with stagnation Spotty, scattered involvement of abnormal glands Signs Gland orifice swollen and inflamed o Increased cloudy and change in viscosity Pouting of orifice due to retained plug of dried secretion (“inspissations”) Area of obstruction may be enlarged with pinpoint swelling of lid (“serration”) Retention cysts and concretions Papillary conjunctivitis Bulbar hyperemia Meibomian glands visible in tarsus TBUT likely reduced Symptoms Range of symptoms similar to meibomian seborrhea (severe to none) Irritation, stinging, burning, stabbing Dry eye symptoms mimicked Red eyes Photophobia Primary Meibomitis Most severe variety of meibomian gland dysfunction Strong association with dermatological conditions Rosacea Seborrheic dermatitis Frequent chalazia- due to decreased resistance Signs Significant pouting oforifices by plugs Inflammation surrounding gland orifice Focal swelling of lid margin Significant stagnation of secretion o Creamy secretion o Cheesy secretion (caseated) o Filamentary secretion (threadlike) o Secretion non-existent Some glands no longer functional o Cystic, no release of secretion o Lid margin dimples in area of cystic gland Bulbar hyperemia Papillary conjunctivitis Retention cysts and concretions Meibomian glands easily visible through tarsus Symptoms Frequent chalazia Possible frequent hordeola Dry eye symptoms o FBS o Grittiness, etc Chronically red eyes Chronically red lid margins Irritation, stinging, burning, stabbing Blurry vision due to tear film disruptions Treatment o Best clinical approach is to treat early for 6-12 weeks and repeat the ocular surface examination to determine whether dry eye remains after the lid disease is resolved. o Evaluate any overlap of staphylococcal blepharitis Do all that is necessary to manage and control the staphylococcal activity Lid hygiene Topical and/or oral antibiotics Culture and sensitivity o Evaluate any overlap of seborrheic blepharitis Do all that is necessary to manage and control the seborrheic condition Lid hygiene o Consider any co-existing dermatologic conditions and co-manage with dermatologist if present; management of the skin condition often improves the ocular condtition Rosacea Seborrheic dermatitis o Manage meibomian gland dysfunction Warm soak mandatory for significant stagnation This opens the pores and melts the core. Heating the lids about 9 degrees F significantly increases meibomian oil production. 2-10 minutes. Can apply wet washcloth towards the end of a hot shower. Make it a part of the daily routine. Critical for primary meibomitis Helpful for secondary meibomitis Melts and softens high melting point waxes Can use microwave heated sock full of uncooked rice, a boiled egg wrapped in a washcloth or commercially available eyelid warming devices. Digital massage of lid margin to express glands In office, performed by the doctor At home, performed by the patient o Patients draw their index finger across the length of the eyelids 10-15 times in one sitting adfter they have cleaned the lid margins. o Extend finger and apply light pressure. Roll the finger upward on the lower lid two times while in upgaze, then roll the finger downward on the upper lid two times while in downgaze. Can use artificial tears to wash away debris. Standard lid hygiene usually massages lids sufficiently; must do warm soak before either massage without soap or scrubbing with soap. Baby shampoo Remember to rinse Overzealous scrubbing can exacerbate lid inflammation, create microabrasions in the dermis and strip the skin of its natural protective oils (sebum), making it susceptible to bacterial infiltration. Consider oral tetracycline Kills bacteria, but depletes oil Ocular rosacea likely, though difficult to diagnose definitively Standard dose is 1gram/day, 4 divided doses, qid, x3 weeks or more Careful, slow tapering to maintenance dose of 250mg per day or every other day Course of therapy is 4-6 weeks. 3 week minimum o Increased usage can cause gynecologic problems o Do not use if <18 years old Artificial tears Maintain normal tear film Improve comfort, reduce stinging, etc. Use regularly, regardless of how eye feels. Combination kits These are available that contain doxycycline, lid cleaning foams or colutions and lid warming devices. Cleeravue- M (Stone Bridge) o Minocycline hydrochloride tablets o With sterilid- a foaming cleanser Cyclosporine A 0.05% (Restasis, Allergan) An immunomodulator that inhibits T-lymphocyte activation and proliferation and subsequently interfers with cytokine induction. Chronic condition No cure, management only Lifelong condition Careful patient education Frequent failure of therapy due to poor compliance, patient frustration with exacerbations, no magic cure, and with premature discontinuation of regimen. Hypersensitivity Reactions Associated with Staphylococcal Blepharitis Background o Staphylococcal exotoxins may cause hypersensitivity reactions Allergic response of conjunctiva and cornea to chornic exotoxin release Phylectenules Marginal corneal infiltrates Allergy responses occur usually over days and weeks, rather than hours Phylectenules o Cell-mediated allergic response to conjunctiva and/or cornea to staphylococcal exotoxins, tuberculosis, or GI parasites Nodular eruption of leukocyte infiltration Locations of phylectenules Conjunctiva Limbus On cornea (least common location) o DDx: ask about a chornic cough or URI o See section in conjunctiva for signs, symptomolgy, and treatment of phylectenules Marginal Corneal Infiltrates o Neutrophils (polys) chemotactically drawn into cornea from limbal circulation, in response to staphylococcal exotoxins acting as antigens At inferior limbus, near lid margin Tear film bathes cornea with exotoxins Corneal staining is frequently seen in the area, typically inferior third of the cornea o See section in cornea for signs, symptomolgy, and treatment of marginal corneal infiltrates. Angular Blepharitis Background o Two causative organisms Moraxella lacunata Staph aureus or epidermidis (more common) o Various manifestations of moraxella organisms Angular blepharitis Follicular conjunctivitis Corneal ulcer o Moraxella is “epidemic” in institutional settings Angular blepharitis in dehabilitated, elderly, institutionalized patients (alcoholics, etc) Follicular conjunctivitis in school settings (previous name “orphanage conjunctivitis”) o Tear film remains in lateral aspect housing bacteria Signs o Eczematoid reaction (characteristic of angular blepharitis) at lateral canthi o Maceration (breakdown of tissue due to continued exposure to moisture)- skin cracks o Red lid margins at outer canthi o Lask scaling typical of staphylococcal or seborrheic blepharitis is not specific for angular blepharitis o Epiphora from senile ectropion may exacerbate the maceration. Symptoms o Chronic lid irritation o Possible itching o Skin repeatedly drying out, scaling, then cracking open Treatment o Differential diagnosis between Moraxella and staphylococcal infecvtions Institutional setting suggests Moraxella Impossible to establish identity of microbe without culture o Antibiotic ointment to involved area, bid to qid For Staph, use bacitracin or erythromycin For Moraxella, use sulfacetamide, neomycin, erythromycin, or polymixin B If identity of microbe not clear, use bacitracin and polymixin B (Polysporin) o Zinc sulfate solution, bid to qid Available in Vasoclear A, Cleareyes ACR, Visine AC or in Zincfrin drops Apply with cotton tipped applicator Astringent action reduces maceration o Culture and sensitivity testing if both antibiotic ointments and zinc drops are ineffective o Moraxella are uncommon, staphylococci are uncommon Empiric therapy: use zinc drops and Polysporin ointment, bid to qid If therapy is unsuccessful, obtain culture Check compliance with therapy regimen Blepharitis Associated with Dermatologic Conditions Background o Association of blepharitides with dermatoses Seborrheic dermatitis firmly associated with seborrheic blepharitis, variable with meibomitis Rosacea firmly assoctaed with primary meibomitis and variable with seborrheic belpharitis Seborrhea sicca (dandruff) has a variable association with seborrheic blepharitis Acne juvenilis has variable associations with all types of blepharitis and meibomitis o Some dermatoses have parallel pathophysiological processes which occur in various blepharitides Sloughing of epithelial cells Seborrheic dermatitis, acne juvenilis Secondary and primary meibomitis Adherence of epithelial cells in obstructive mass Acne juvenilis Secondary and primary meibomitis Overproduction of sebaceous material Acne juvenilis and rosacea Seborrheic blepharitis and all varieties of meibomitis Bacterial proliferation in excessively oily environment Only in acne juvenilis Variable association with blepharitides o Bacteria proliferate in oily environment; resistance drops, with flare-up of staphylococcal or mixed blepharitis o Stagnant meibomian glands from a reservoir for bacteria; reduced resistance allows hordeola to develop Acne Juvenilis o Four concurrent pathophysioloical processes Keratinization and adherence of epithelial cells Excess lipid production in sebaceous glands Bacterial proliferation of propionibacterium acnes Hormonal imbalance of androgens to estrogens o Pathogenesis Epithelial cells keratinize, formina a self-adhering obstructive mass in the follicle Open comedo or blackhead Closed comedo or white head Comedo obstructs sebum outflow from the follicle; initial stage called obstructive acne. Lipid production continues in spite of obstruction P. acnes’ proteases begin inflammatory reaction of pustule; second stage called inflammatory acne As inflammation becomes chronic and involves deeper tissue, pitting and scarring occurs; final stage called cystic acne o Treatment After keratinization of follicular duct wall Keratolytic agents (peeling agents) increase rate of cell turnover, with reduced adhesion of cells and reduced comedo formation Peeling agents o Resorcinol (Clearasil) o Sulfur, salicyclic acid *Fostex) o Benzoyl peroxide (5 and 10% gels) o Tretinoin (Retin-A) Modify bacterial population Topical antibiotics have poor penetration Oral antibiotics o Tetracycline or erythromycin, 250mg bid to qid (or EES 400mg, bid to qid) o Doxycycline or minocycline 50-100mg bid Specific for P. acnes, also reduce lipases Tetracycline potentially able to reduce sebum production Treatments of choice Obstructive acne: peelin agents (Retin-A) Inflammatory acne: oral antibiotics Cystic acne: isotretinoin (Accutane) o Correlation of acne juvenilis with blepharitis Oily skin may allow proliferation of staphylococci since excess oil and free fatty acids can reduce resistance of skin and alter normal flora. Extra oil production may relate to production of greasy crusts seen in seborrheic blepharitis However, poor correlation at present between acne juvenilis and all varieties of blepharitis Seborrheic Dermatitis Background o Chronic inflammatory skin condition o Generally a benign condition o Quite common; very often asymptomatic o Uncertain etiology and pathophysiology No proven microbial activity Stress may exacerbate scaling and itching Signs and symptoms o Typical locations Primary site: scalp Secondary, less frequently involved areas Forehead at margin of hairline Eyebrows Nasal folds Retroauricular area Presternal area (chest) o Greasy, yellow scales, surrounded by erythema o Epithelium sloughs off, so skin looks irritated o Generally asymptomatic, though might have itching. Treatment o Goals of treatment Remove scaling Reduce oiliness Emilinate redness Control itching when present o Shampoos that reduce formation of keratinized cells Selenium sulfide Selsun blue (OTC), head and shoulders Selsun 2.5% and Exsel 2.5% (both rx) Zinc pyrithione X-Seb and Zincon (OTC) Coal tar T-Gel (OTC) Tegrin (OTC), X-Seb T Zetar (OTC) Shampoo twice weekly o Reduce significant erythema and itching with topical steroid Hydrocortisone is frequently used All OTCs are 0.5% and 1.0% concentration Rx preparations are 0.5%, 1%, and 2.5% Lotion is best for scalp (least oily) Use cream or ointment on othe areas with glabrous (smooth, non-hairy) skin OTC hydrocortisone available in Caldecort, Dermolate, Cortaid, Lanacort, Dermarest Dri Cort, or generics o Seborrhea sicca (dandruff) is scaling without erythema; shampoo once or twice weekly o Patient education Chronic, common condition May be exacerbated by stress Avoid steroid abuse, either OTC or Rx. Correlation of seborrheic dermatitis with blepharitis o Seborrheic lash scaling seen inpatients with seborrhea sicca or seborrheic dermatitis o Uncertain correlation of seborrheic dermatitis with meibomian gland dysfunction. Rosacea Background o Affects 14 million Americans, 1 in 20 adults in US exhibits dermatologic features of rosacea. 60% experience associated ocular rosacea. (2008) o This is an overproduction of oil o Presents primarily on face o Doesn’t occur in African-americans, Asians, or latinos. o More common in fair-skinned individuals o 4th to 7th decades of life. o Females affected 2-3 times more often than males o But more severe in men o Seen more in cheeks in women and nose in men o Different from acne juvenilis since limited mostly to face; rosacea does not involve chest or back o Flushing and rhinophyma, specific for rosacea, are not seen in acne juvenilis o P. acnes and other microbes not active in rosacea o Comedos in acne juvenilis, not specific for rosacea o Extremes of temperature (hot or cold), hot beverages, and exertion increase vasodilation and facial flushing in rosacea o Presents as facial rosacea, ocular rosacea, or oculo-facial rosacea (study in 1953) Facial rosacea presents in 55% Ocular rosacea (severe, specific, classic) presents first in 20% Ocular and facial rosacea present simultaneously in 25% Much greater overlap with milder forms of ocular and facial rosacea. o Facial rosacea about 2x more grequent in women than in men, though men are afflicted with more severe presentations than women. o Ocular rosacea incidence equal between the sexes. o This is a clinical diagnosis. No laboratory testing or pathology specimens required. o Differential diagnosis Acne vulgaris, contact dermatitis, seborrheic dermatitis, eczema, sarcoidosis, lupus, perioral dermatitis and drug-induced photosensitivity. Prerosacea o Flushing o May develop erythema, a persistent midfacial redness. o Nose, chin, cheeks, and central forehead may all be affected. Facial Rosacea o Areas involved Blush areas of face (cheeks primarily) Also nose, chin and forehead Superficial tenangiectasias o Mild variety- Erythematotelangiectactic rosacea “telangiectasia stage” Simple redness, “ruddy complexion” Red glow Fine blood vessels on the skin surface. Blood vessel dilatation and telangiectatic changes Face blushes and flushes easily o Moderate variety- Papulopustular rosacea “popular-pustular stage” Acne stage Skin bumps, pimples and plaques Single or multiple lesions, waxes and wanes Papules perhaps more common o Severe variety- Phymatous rosacea “glandular hyperplastic stage” Phymas and tissue hyperplasia Overgrowth of sebaceous and connective tissue of nose (rhinophyma) W.C. Fields nose Ocular Rosacea o Etiology Inflammation from Staphylococcus exotoxins Ocular signs are secondary to the inflammatory skin condition o Multiple ocular presentations Never the only diagnosis Almost all presentations are non-specific Lid manifestations very common Tear film disturbances very common Conjunctival presentations less common Corneal manifestations uncommon to rare Anterior uveitis very uncommon o Lid manifestations of ocular rosacea Chronic blepharitis (similar to staphylococcal type) Meibomitis (frequently primary meibomitis Telangiectactic vessels on lid margins Chalazia and hordeoli o Tear film manifestations of ocular rosacea Frothing Quick TBUT Dry eye and FBS o Conjunctival manifestations of ocular rosacea (in decreasing order of frequency), per Catania “Dry eye” conjunctivitis Tearing and serous discharge with conjunctivitis Prominent limbal arcades (telangiectasias) 360 degree superficial circumcorneal flush Nodules (gray, vascularized) near limbus, self-limiting o Corneal manifestations of ocular rosacea (in decreasing order of frequency and increasing order of specificity) Peripheral SPK Pannus, superficial, about 1-2mm over limbus Neovascularization (360 degree anterior stromal) Epithelial edema (peripheral, diffuse) Microcysts (peripheral and diffuse) Peripheral EBMD changes (map-dot-fingerprint), not in typical central location Ill-defined SEIs (peripheral) Peripheral (to diffuse) anterior stromal infiltration and hazing, often triangular in shape when near limbus. Peripheral corneal thinning o Ocular rosacea changes do not occur synchronously with facial rosacea changes. Underdiagnosing of Ocular Rosacea o Easily missed since the doctor fails to examine the whole face of the patient o No laboratory or histopathological tests o Facial lesions need not be severe for rosacea to be present; mild presentations can be dismissed when their recognition would assist in diagnosing oculo-facial rosacea in a patient with non-specific ocular findings (blepharitis, meibomitis) o No definitive criteria exist at present for ocular rosacea Browning and Proia suggested a weighted scale for diagnosis (Surv. Ophthal 1986; 31: 145-158) Clinical Signs or Symptom Rhinophyma Pustules Papules Facial Telangiectasia Facial Erythema Corneal New Vessels Corneal Scarring or Thinning Recurrent Chalazia Recurrent Hordeola Blepharitis Conjunctivitis Meibomian Gland Dysfunction Short TBUT Iritis Burning or Tearing Facial Flushing Clinical Suspicion Tentative Diagnosis Probably Diagnosis Certain Diagnosis Points 20 9 9 8 8 3 3 2 2 1 1 1 1 1 1 1 6-10 points 11-19 points 20 or more points 20 or more points with concurring opinion of dermatologist. Treatment o Depends on both the subtype(s) and present stage/ severity of the condition o Treat facial rosacea similarly to acne juvenilis o o o o Peeling agents to enhance turnover of skin and restore normal skin Tetracycline (Primary Therapy) Decreases bacterial lipase 250mg, qid, up to 9 weeks o Little longer than meibomitis Slowly taper down to 250mg qd or qod Doxycycline is excellent alternate therapy o 100mg bid x6wk followed by qd for 2-4 weeks o Bid dose, improved compliance Action may be anti-inflammatory, with reduction of FFAs Short course of therapy: 250 mg, po, tid for three weeks; then 250mg, po, qd x 3 weeks Isotretinoin (Accutane) under FDA investigation for rosacea, no approved. Metro-Gel (topical metronidazole)- an antifungal Antimicrobial, anti-inflammatory, and immunosuppressant properties Oral and topical Effective for inflammatory lesions, not telangiectasias. Treatment of ocular rosacea Treat chalazia, hordeola, meibomitis, and blepharitis with standard regimens Artificial tears on a regular basis, qid or more frequently Mild steroid for peripheral keratitis (topical) 0.12% prednisolone acetate, bid Too strong a concentration will lead to corneal melting and perforation Oral therapy (tetracycline) oftem improves ocular manifestation Longterm therapy Periostat (doxycycline hyclate) 20mg either qd or bid. Oracea (doxycycline monohydrate) Treat inflammatory rosacea in adults First drug to be approved for papulopustular rosacea only. 30 mg of immediate-release medication and 10mg ofdelayed-release medication in one capsule. Good anti-inflammatory only, not antibiotic. So no resistance develops. Surgery A pulsed-dye laser for erythematotelangiectatic rosacea may be effective in reducing redness and telangiectasia. Surgical ablation, electrocaurtery and CO2 laser (to remove hypertrophied tissue and reshape the nose) therapy are also available. Patient education Chronic condition which is treatable. Avoid extremes of temperature (hot and cold), hot beverages and circumstances which increase vasodilation and facial flushing. Viral Infection and Inflammation Molluscum Contagiosum Background o Pox virus which can cause epithelial lid growths due to inflammation of the skin of the lid o Usually children, can occur in adults o Mildly contagious- can be picked up by manipulation of the core of the lesion o Grows over a 1-2 month period after inoculation Clinical presentation o Symptoms Lid growth(s) Follicular conjunctivitis (probably toxic), “red eye” Corneal epithelial disruption (probably toxic) “scratchy eye”- diffuse or marginal epithelial disruption Can be conjunctival lesions “lump on eye” o Signs In groups/ small Looks smooth with core Anywhere on face Lid growth is a small grey-white nodule with central light colored (usually) core which can be removed Lesion may be filled with a cheesy material Slowly grows over 3 months to 2 year period. Can have discharge which produces ocular irritation (follicular conjunctivitis) Will often resolve spontaneously But rule out SCC first Central core is emitted before resolution Evaluate carefully and rule out BCC or SCC May also mimic keratoacanthoma but keratoacanthoma is larger, more quickly progressive There is no bleeding or ulceration Treatment o Treatment of the corneal or conjunctival effects involves treatment of the lid growths o Treatment of lid growths Referral for surgical excision If appears like BCC< SCC, needs excisional biopsy Can remove the central core (which contain viral material) Clean surface with alcohol wipes Loosen core with sharp instrument such as spud Squeeze out contents Re-clean May have to be repeated on multiple occasions before remission of lesion occurs o Can be a progressive disease in immunosuppressed patients so notification of treating physician is essential Varicella- Chicken Pox Blepharitis Background o Varicella zoster virus infection Chicken pox in non-immune host (usually child) Zoster in immune host (usually adult) o Highly contagious, spread by droplet infection Signs and Symptoms o Initially have fever, malaise, myalgia o Skin rash Maculopapular rash is initial presentation Everywhere, vs impetigo which is on exposed areas. Lesions later turn into vesicles or pustules With clear fluid. Cloudy or expressed. Crusts form in 2-4 days Rash has a duration of 2-3 weeks Scars o Locations: thorax, scalp, face, mucous membranes o Itching is most common symptom o May have lid vesicles and conjunctivitis Usually no conjunctviisit or keratitis unless it is very close to the eye. o More serious, but less common, ocular manifestations Phylectenule on lids, conjunctiva, limbus Excavated ulcers on lids SPK, shallow corneal ulcer o Madarosis if pox is on lid. o Very contagious. Do not be around for 3 weeks if you have never had it. Treatment o Supportive therapy for skin rash using drying, cooling dermatologic preparations Calamine lotion Burow’s solution, 1:40 or 1:20 70% isopropyl alcohol Might hurt Pramoxine in Aveeno Anti-itch cream or lotion (praxomine, calamine, camphor); Caladryl (pramoxine, calamine); Caladryl Clear Lotion (pramoxine, zinc acetate) o Prophylactic topical antibiotic ointment on lesions o Oral antihistamine to reduce itching Chlorpheniramine maleate 4mg, po, qid Diphenhydramine 25mg, po, tid to qid Antihistamines in children’s doses are much lower than adult doses Allerest Children’s Chewable (1mg of chlorpheniramine maleate) Triaminic Chewable (0.5mg of chlorpheniramine maleate) Adult doses are not FDA approved for pediatric use; talk to pediatrician first before using any antihistamine in children (medico-legal issues) Avoid scratching and picking at lesions Corneal protection Prophylactic broad spectrum antibiotic Antivirals for keratitis (varying opinions) Oral acyclovir (Zovirax); newly FDA approved for use in chicken pox in kids. Doses are Age 2-12, 20mg/Kg, po, qid Age 13-18, 800mg, po, qid This causes a shorter infection and fewer lesions. No steroids, because it hampens the immune system. Herpes Zoster Ophthalmicus (Vaircella-Zoster Blepharitis) Background o Caused by varicella virus Cannot have zoster without chicken pox o Virus lies dormant in dorsal root of trigeminal ganglion Trigger factor causes activation of virus Virus “creeps” down axons to erupt in skin Affects corresponding sensory dermatome o Thoracic region is site most often affected; called “shingles” without ocular involvement; about 55% of cases. Usually more localized o Called “herpes zoster ophthalmicus” (HZO) when the first (ophthalmic division) of thes three divisions of the trigeminal (CN V) is involved; about 20% of cases o Ophthalmic division (V1) has three divisions of its own (NFL) Frontal with two division of its own Supraorbital o Forehead o Scalp Supratrochlear o Middle forehead o Upper lid and conjunctiva Most commonly affected nerve in HZO Lacrimal Lacrimal gland Lateral skin of eyelids Nasociliary with four divisions of its own (LINE) Long ciliary o Sensory innervations to globe o Cornea o Iris o Ciliary body o Pupil dilator Infratrochlear o Medial eyelid skin o Medial conjunctiva o Lacrimal sac o Roof of nose Nasal o Nose o Tip of nose Posterior Ethmoidal o Ethmoidal air cells o Sphenoidal sinus Involvement of nasociliary branch results in external and/or internal ocular involvement Maxillary (V2) is second division of trigeminal Roof of mouth Upper teeth Cheeks Nasopharynx Mandibular (V3) is third division of trigeminal Jaw Lower lid Tongue External ear Trigger factors which activate the virus, typically in an aging or compromised immune system Stress and fatigue Emotional or physical trauma (surgery) Neoplasia Corticosteroids or other immunocompromise HIV infection Symptoms o Prodrome Headache and malaise Fever and chills o Varying sensations Neuralgia (significant pain) classically 1-2 days after prodrome Tingling of skin (hyperesthesia) classically 2-3 days after prodrome Especially with hair brushing May also have numbness or crawling skin HZO characteristics: scalp thingles or hurts (exacerbated by combing hair), also itching and/oor irritation around eyes). o Persistent and frequently excruciating pain, easily aggravated by minor stimuli Signs o Diffuse erythema first, moving from forehead down to eyelids o Crops of clear vesicles over affected dermatome o One sided (never cross over 1-2mm past midline) o Clear fluid in vesicles turns yellow and turbid o Vesicles burst and leave scabs (takes 305 days); risk of permanent scarring o Hutchinson’s sign Involvement of tip of nose or side of tip of nise Lesions present, sensitive, painful to touch 75% of patients have ocular involvement if Hutchinson’s sign is positive 25% of patients have ocular involvement if Hutchinson’s sign is negative. o Ocular involvement discussed more in cornea and uvea sections Treatment o Skin and lid lesion therapy (self-limit in 3 weeks) Burow’s solution soaks (1:40) o o o o o Alcohol compresses (70% isopropyl) Prophylactic antibiotic ointments Topical steroids prevent large crusts Antibiotic-steroid ointment (Blephamide, etc) bid to tid Hydrocortisone ointment, tid to qid Oral antihistamines, tid to qid Numbs the nerve conduction See related material in cornea and uvea sections Refer to other health care providers: corneal specialist (with HZO), dermatologist, internist Oral acyclovir (Zovirax): critical to start as soon as possible. 800mg, po, 5x/day Famciclovir 500mg, tid Other medications Oral steroids Analgesics Amitriptyline (post-herpetic neuralgia)/ Elavil Capsaicin (Zostrix), post herpetic neuralgia Primary Herpes Simplex Background o “Fever blister”/ cold sore o Not recurrent which is sight threatening o Infected by direct contact (saliva and mouth contact) or contact with active skin lesions; incubation of virus is 10 days. o Most often seen in infants and young kids (up to 5 years old) or in teenagers Moms/dads kiss them goodnight. o Not younger than 6 months (unless infected with HSV 2 at time of birth) o Very few primary infections are clinically significant. Mild to moderate fever Mild eye involvement (non-specific “pink eye”) 90% of initial episodes are asymptomatic o Once infected, the host has the virus for life; hopefully lives in sumbiosis with virus; dormant viruses reactivate in about 25% of patients due to the following inciting factors UV exposure Trauma Temperature extremes Fever Steroids Infectious disease Menses Surgery o Most adults are infected with HSV 1 as children By age 5, 60% are infected By age 15, 90% are infected o Adults can have primary infections with HSV 2 (genitals) o Serious ocular findings are uncommon in primary herpes infections Skin lesions around lips (common) and eyelids (uncommon) Follicular conjunctivitis (rare) Keratitis (even more rare) Signs and Symptoms o Skin vesicles are most common of the presenting signs. Most frequent around and in mouth or at mucocutaneous border of lips. Often next to lid margins (single or grouped), lower lid more often than upper lid. Possibly blurred between eyelashes Clear, then yellow (3-5days later), fluid-filled vesicles, pin-head sized Vesicles break and then dry to form yellow-brown crusts (7-10 days) which later ddrop off without permanent scarring. Very rough, in crops Painful Originally opaque/ flat o Erosions at mucocutaneous junction of lid skin or skin ulcers elsewhere, occurring separately or simultaneously; shallow ulcers heal within 2 weeks. o See conjunctiva and cornea sections for material on these areas. Treatment o Generally non-specific treatment; no definitive therapy, since lesions classically self-limit Lesions do not leave scars Topical Zovirax (acyclovir) possibly used (though no standard of care); tid to qid for 3 weeks, applied over mildly debrided lesions Warm saline soaks Good hygiene to cleanse Dry agents (except on lesions on lid margins) Calamine lotion 70% alcohol Burow’s solution (1:40) Topical antibiotic ointment use is optional; for avoidance of secondary bacterial infection Oral acyclovir used only if very severe Refer to dermatology if no clearin in 7-10 days Steroids absolutely contraindicated; their use may predispose to serious corneal involvement o Refer to conjunctiva and cornea sections for further material on treatment. Allergic Lid Disease Uticaria and Angioneurotic Edema (Type I Hypersensitivity) Background o Antigen-antibody reaction o Thin lid skin highly sensitive to allergens o Vascularized, spongy tissue edema and swelling o Type I allergy in general caused by Insect bites, bee stings Food allergies (chocolate, milk, nuts, eggs, shellfish, cheese, soybeans) Medications (penicillin, barbiturates, aspirin) Inhalants (mold, dust, pollen) Ingestants (artificial colors, preservatives) o If bilateral, think systemic Signs and Symptoms o Uticaria (synonym = hives) Smooth, slightly elevated patches (wheals) Redder than or paler than surrounding skin Underlying tissue is normal and not swollen Bilateral History of contact o Angioneurotic edema Higher risk of anaphylaxis Superficial skin is normal Deeper tissue edema Lid(s) swollen (ptotic or closed) More common in young because good immune system o Itching- 100% necessary (8-10/10) o Rarely lasts more than several days Treatment o Cold packs for the first 24 hours o Warm packs for second and subsequent days o Oral antihistamine, OTC Nonselective, fast acting, stops the itching Chlorpheniramine maleate 4mg, po, qid Diphenhydramine 25-50mg, po, tid to qid o Oral antihistamine, Rx Loratadine (Claritin) 10mg, qd Cetirizine (Zyrtec) 5-20mg, qd Allegra (Fexofenadine) 60, 100, 500mg, bid o If bee sting, flick out stinger if present; do not tweeze since venom is forced out by tweezing. o Off label antileukotrienes (Cingulair, Accolate) Usually used for asthma. o Follow-up Severe condition: see next day Moderate condition: see in 2-3 days Mild condition: see in 3-5 days or prn Contact Dermatitis- Type IV Background o Delayed hypersensitivity reaction Prior exposure and sensitization to allergen Strong allergens need about 5-10 days Weak allergens require months to years Re-exposure to allergen Reaction begins 12-72 hours later Sometimes difficult to determine the cause o Possible allergens for Type IV reactions Topical medications (neomycin, maxitrol, and neosporin) Cosmetic preservatives Rubber, acrylics (frames) Plants Formaldehyde Nickel Meds/ DPAs o Allergens of particular interest in eyelid allergies Perfumes and fragrances Neomycin Paraben mix (preservative) in Cosmetics Topical creams, ointments, lotions Topical conrticosteroid preparations PPDA (Paraphenylenediamine) Permanent and semi-permanent hair dyes PABA sunscreens Sulfonamides “Caine” preparations Topical anesthetics Anti-itch preparations Formaldehyde Cosmetics Wash and wear clothing Paper Nickel- MANY home and industrial products Balsam of Peru Perfumes Medications Shampoos and hair products Signs and Symptoms o Itching o Early: oozing, erythematous skin o Chronic: skin dries, thicknes, scaly peeling o History of exposure to New medications New clothing Insecticides New cosmetics Recent travel Gardening New work environment (particularly industry) Treatment o Identify specific allergen(s) by history o Patch testing if nature of allergen uncertain “band aid” with known allergens to see if there is a reaction Challenge test- place allergen against antiallergens o Blood test for allergies o o o o o o o o o o Avoid known allergens Burow’s solution, only in acute presentations Domeboro Powder Packets (OTC) Soak clean cotton cloth in solution (old T shirts. Bedsheets, pillow cases) Soak affected area for 20 minutes bid to qid, 1:40 ot 1:20 concentration Re-soak cloth when it dries out. Topical corticosterone cream or ointment to calm itching OTC 0.5% or 1% hydrocortisone products Lotion (humid) or ointment (dry climates) Very severe cases (poison oak, etc) may require systemic steroids (usually po or IM x1) Oral antihistamines, OTC; same regimen as in Type I allergies NSAID ointments Elidel (Pimecrolimus) Protopic (Tacrolimus) Skin moisturizers, in chronic presentations Acute presentation Astringent (Burow’s) if skin is not too dry Topical steroid, oral antihistamine Discontinue/ avoid irritant Risk of lichenification, with resulting excoriation and secondary infection Conjunctivitis (from atropine, neomycin) usually requires steroid pulse with prednisolone 1% or fluorometholone, short-term Follow-up: same regimen as in Type I allergy; expect much slower resolution for chronic (eczematous) type Infestations of Lids Demodex Background o Mites residing in follicles, primarily in facial area Hair and eyelash follicles: Demodex folliculorum Sebaceous glands: Demodex brevis o Older individuals; virtually all adults over age 50 are infested o Demodex folliculorum characteristics Sexually active in the dark Mites leave follicle and copulate on lid margins Females return to follicle to lay eggs Lif span is about 14 days So treatment needs to be 14+ days o Excessive number of mites leads to overt clinical presentation, possibly with symptoms Signs and Symptoms o Some asymptomatic o Bright lights cause mites to recess into follicles o Follicle infestation causes chronic edema Brittle, easily broken lashes (uneven) Lashes easily epilated or fall out spontaneously Pyramidal follicles from edema, mites and eggs Mound of tissue/ debris at the base of the lashes Possibly thickened eyelids from chronic edema o Collarette- thin sleeve at base of lash o Non-specific symptoms, similar to those of blepharitis Itching, burning, vague complaints of soreness, heaviness Corneal irritation (from misdirected eyelashes) o Symptom suggestive of demodicosis Itching at night or in dim light (early morning) Heavy eyelids Irritation, worse in warm weather o Diagnosis of demodicosis depends on Collarettes and pyramidal elevation of eyelash follicles Suggestive symptoms Microscopic examination of mites after eyelash epilation Treatment o In-office Anesthetize lid surface with 0.5% proparacaine Lure mites to the surface with ether Wait 5 minutes Brush 70% alcohol on lid surface Take care not to get ether or alcohol on the cornea Repeat process once weekly for three weeks o At home Lid hygiene (either LC 65 or 50:50 baby shampoo) Lid hygiene must be done twice daily Upon awakening At bedtime After doing lidd hygiene at bedtime, apply copius amount of ophthalmic ointment to lid margins 1% yellow mercuric oxise, OTC (StyeTM) Bland petroleum (Lacrilube SOP, etc) Polysporin or erythromycin Must clean off all ointment the next morning Takes 3-4 weeks for response Phthiriasis Palpebrum Background o “Pediculosis” is general term for louse infestation Body louse (Pediculus corporis) Head louse (Pediculus capitis) Pubic louse (Phthirus pubis) First two are nearly identical, but the last can be distinguished by its broad abdomen and shorter, thicker claws. o A parasite that feeds by sucking blood from the host. To feed, the crab louse injects poisonous saliva into the skin. This produces localized scabbing, itching and irritation. A painless bluish discoloration of the skin that does not disappear with pressure may occur around the area of the bite. o Attach themselves (using their middle and hind legs) among the more widely spaced hairs of the pubic region, armpits and less commonly, the eyebrows and lashes. o Not thought to be vectors for disease. Just irritating. o Females lay 2-3 eggs in a 24 hour period. o Eyelid presentation Caused primarily by the pubic louse (“crabs”) Infrequently caused by Pediculus capitis Simultaneous lid and pubic manifestations o Generally associated with Sexual transmission (1/3 of patients have STD)- so also refer to PCP Transmission also occurs by clothing, bedding, towels Poor hygiene and sanitation Signs and Symptoms o Symptoms range from none to intense itching; due to irritation of louse’s secreted saliva, digestive juices and excreta o Signs Possible palpable pre-auricular node, due to toxins/ STDs Louse or lice, about 1mm in diameter Nits (ova), gray-white shells containing eggs (translucent) Dark red crusting is a mixture of blood and feces “Dark sleep” Very severe cases may have shallow skin ulcerations, possibly keratoconjunctivitis Treatment o Must treat concomitant pelvic or head lice Probability of infestation in other areas of the body were discussed and the patient was advised to seek the care of a physician immediately. Kwell (Rx only)- gamma benzene hexachloride (lindane); also used for scabies Rid (OTC)- pyrethin A-200 Pyrinate (OTC)- pyrethin Nix (OTC)- permethrin Generally one shampooing is sufficient, but manufacturers suggest two shampooing over two weeks Not to be used for pregnant females or infants o Treat family members, sexual contact, and/or classmates Since the organisms can be transferred by close physical contact. o Clothing, bedding, linens heat-treated in laundry dryer, at 140 degrees F for 20-30 minutes (“high” setting) o Medical exam to rule out STDs o Discard cosmetics o Lid therapy (in-office) Direct removal of nits or lice with forceps Pick off and place in CL vial with rubbing alcohol In many cases, the lashes themselves have to be removed either by epilation or by cutting the lashes at their base, because the nits are adhered so strongly to the lash that the only way to achieve nit removal is to remove the lash as well. o o Smother nits and lice on lids with ointment Bland ointment (Lacrilube SOP,Refresh pm etc) qid o Best option: reasily available in office, well tolerated by patients, has few side effects. o No non-ophthalmic ointments such as Vaseline. 1 or 2% yellow mercuric oxide Ammoniated mercuric oxide, 3% Antibiotic ophthalmic ointments Physostigmine 0.25% ointment- too toxic o Cholinesterase inhibitors 20% fluorescein to “paint” lids 2.5% pyrethrum cream Never use Kwell around lids- too toxic Some of these are rarely available in practice, so they may not be practical. Repeat in 24 hours in office. Remove all nits and organisms. Repeat in one week Nits hatch in cycles of 7-10 days. One last follow up in 2 weeks Medications Antibiotic-steroid combinations can (and perhaps should) be considered if lid margins are noticeably inflamed, but removal of the offending parasite will typically resolve inflammation. After two weeks of therapy (per manufacturer’s instructions), recheck for nits; if nits are present, patient is either non-compliant or re-infested; treatment must be repeated. Brown Recluse Spider Bite Causes infection and necrosis Mimics keratoacanthoma Comes in matter of days Oral antibiotics and follow-up Cosmetic Eyelid Surgery History o 1st recorded documentation of blepharoplasty was in the 1st C AD when Aulus Cornelius Celsus described the excision of the skin for “relaxed upper eyelids” in De Re Medica. Does Medicare cover it? o The following three criteria are needed by Medicare and most insurance companies to consider an upper eyelid blepharoplasty a medical necessity. Documentation by the clinican of the diagnosis of dermatochalasis (excess skin) or ptosis (droppy upper eyelids) Pre-operative photographs of the patient Documented improvement of more than 12 degrees in superior visual field with the eyelids taped. Upper Eyelid Blepharoplasty o Upper eyelid blepharoplasty involves removal of excessive skin or muscle to give a more open vibrant look to the upper eyelids. Lower Eyelid Blepharoplasty o Reason for bags: Herniated orbital fat secondary to a weak septum Loss of volume in the midface with aging Excessive skin overhanging o Excessive orbital fat is almost never removed but rather contoured. Instead, the herniated orbital fat is repositioned back into the orbit and the orbital septum is plicated with sutures to give it strength. Some patients may need a pinch of skin removed from the lower eyelids to give it a tight youthful appearance. Midface volume is addressed during the same surgery with autologous fat injection. Postoperative Care o Most cosmetic surgery is performed either under local anesthesia or local with IV sedation, otherwise known as “twilight” anesthesia. Bruising and swelling in the first postoperative week is normal. Ice packs are used to reduce swelling for the first 48 hours. Typiucally most patients are able to return to work or normal activity within one week after surgery. All patients use ophthalmic antibiotic ointment in the postoperative period. Sutures are removed one week after surgery. Revisional Eyelid Surgery o Some of the most dreaded complications of facial platic surgery are those associated with the eyelids. o The most common complaint is the inability to close the eyes completely after previous cosmetic surgery. This problem usually happens when excess tissue and skin were removed during the previous surgery. There are several procedures which can be done or combined to achieve the desired functional and cosmetic outcome. o Although subtle, the natural youthfull eyelid is V-shaped at the corners. The rounded corners of the eyelids after some cosmetic eyelid surgery is an artificial “operated appearance.” This can interfere with normal blink dynamics. The patient usually complains of tearing or dry eyes. This problem can be reversed by a special surgical technique on an outpatient basis. Postoperative hollowness can be revised by placement or injection of fat into the eyelid or orbit. Lumigan Bimatoprost Thyroid disease Organ specific autoimmune process. Expect this with lid retraction. Exophthalmometer- measures the distance the globe protrudes from the orbit (proptosis) o Looks like a pupillometer Normal 12-21mm, ave = 16mm Toxic goiter 12-24mm, ave = 18mm. Thyroid Orbitopathy (most common) o Because it affects the globe o Inflammation o Edema o Secondary fibrosis o Women more than men, 5:1 o 30-50yo o 7% have symptoms: proptosis, diplopia, optic neuropathy, eyelid retraction. MR thickens, along with other muscles and fat. The tendons are normal. o Impinges on the ON and damaging it, causing LOV. This is a lifelong condition Treatment o Treat the thyroid gland (surgery to remove sometimes or drugs to decrease its activity). Iodine 135 destroys the gland. It has a MW of 135. o Treat dry eye with AT.