- Sandhills Center
advertisement

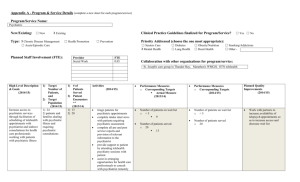
Sandhills Center B-3 Physician Consultation/ Psychiatric Consultation (Adult Mental Health/Child Mental Health) Medicaid Billable 02-25-2014 Revised 05-14-14 Revised 10-13-14 Communication between a primary care provider and a psychiatrist for a patient-specific consultation that is medically necessary for the medical management of psychiatric conditions by the primary care provider. This service is coverable under the State Plan under physician services. A consultation service that provides brief, intermediate and extensive levels of consultation between a Psychiatrist and a Primary Care Provider to ensure appropriate management of psychiatric conditions by the Primary Care Provider. The individual must be a patient of the primary care provider. The Psychiatrist may or may not observe the individual as appropriate as a component of the consultation. This consultation may take the form of email, telephone, fax or face-to-face communication. Staffing Requirements Primary Care Provider or Board Certified in Adult or Child Psychiatry and holds a current license in the state of NC. Service Type/Setting Psychiatric Consultation is a periodic service intended to ensure that Primary Care Providers have access to appropriate consultation that is medically necessary for the medical management of psychiatric conditions by the primary care provider. Services provided to individuals that are independently seen by a psychiatrist should be billed under psychiatric CPT codes. This service is not available to a patient who is under the care of another psychiatrist. This service may be provided in the office of the psychiatrist, the primary care provider office or the facility where the individual lives. Program Requirements This service will be delivered by Psychiatrists that are contracted and credentialed by SHC and meet the provider qualification policies, procedures, and standards established by the Division of MH/IDD/SA Services and the requirements of 10A NCAC 27G. These policies and procedures set forth the administrative, financial, clinical, quality improvement, and information services infrastructure necessary to provide services. Page 1 of 3 Utilization Management This service does not require prior approval. Brief: Simple or brief communication to report tests and/or lab results, clarity or alter previous instructions, integration new information into the medical treatment plan or adjust therapy or medication regimen. This level is typically provided in 15 minute increments. Intermediate: Intermediate level of communication between the psychiatrist and the primary care provider. Does not require face-to-face assessment of patient. To coordinate medical management of a new problem in an established patient, evaluate new information and details and/or initiate a new plan of care, therapy or medication regime. This level is typically provided in 16-30 minute increments. Extensive: Complex or lengthy communication, such as prolonged discussion between the psychiatrist and the primary care provider regarding a seriously ill patient, lengthy communication needed to consider lab results, response to treatment, current symptoms or presenting problem. Staffing of case between psychiatrist and primary care provider to consider evaluation findings and discuss treatment recommendations, including medication regimen. This level is typically provided in 31-60 minute increments. Entrance Criteria Must be under the care of a primary care provider, and requires a consultation between a psychiatrist and their primary care practitioner for appropriate medical or MH treatment. Adult ages 18 and older with Serious Mental Illness (SMI) and/or Severe and Persistent Mental Illness (SPMI) and a LOCUS level of 0 (basic level) or greater. Children ages 3-21 with serious emotional disturbance (SED) and a CALOCUS level of 0 (basic level) or greater. Continued Stay Criteria The recipient continues to meet eligibility criteria and participant needs continue to require this service. Discharge Criteria Primary Care Provider no longer requires assistance with the individual’s psychiatric needs. Page 2 of 3 Expected Outcomes Amelioration or stabilization of psychiatric symptoms or appropriate referral to medically necessary services to achieve psychiatric stabilization. Service Documentation Requirements Minimum standard is a progress note for each treatment encounter that meets the criteria specified in Clinical Coverage Policy No. 8C, and includes, but not limited to, the recipient’s name, Medicaid identification number, date of service, the name of the service, the duration of the service, purpose of contact, describes the provider’s interventions including the time spent performing the interventions, effectiveness of the intervention, the signature, credentials and licensure of the staff providing the service. Refer to Clinical Coverage Policy No. 8C for a complete listing of documentation requirements. Service Exclusions/Limitations Total expenditures on Physician Consultation cannot exceed the 1915(b)(3) resources available in the waiver. Physician Consultation may not be provided by family members. LME/MCO Monitoring and Quality Management Protocols for Review of Efficacy and CostEffectiveness of Alternative Service Sandhills Center will monitor this service for quality and fidelity to the definition through billing audit reviews. Page 3 of 3