Task #1 When and how to conduct hand washing. What does the
advertisement

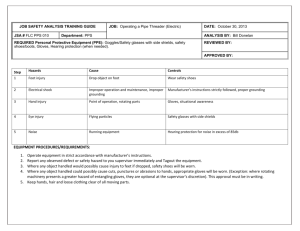
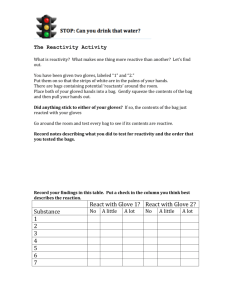
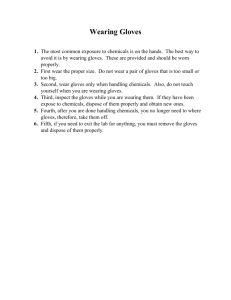
Task #1 When and how to conduct hand washing. What does the learner do? Defines “hand hygiene” and identifies when to wash hands. What does the learner need to know to do this step? When to wash hands. A. When hands are visibly dirty or contaminated with proteinaceous material or are visibly soiled with blood or other body fluids, wash hands with either a non-antimicrobial soap and water or an antimicrobial soap and water. B. If hands are not visibly soiled, use an alcoholbased hand rub for routinely decontaminating hands in all other clinical situations. Alternatively, wash hands with an antimicrobial soap and water in all clinical situations. C. Decontaminate hands before having direct contact with patients. D. Decontaminate hands before donning sterile gloves. E. Decontaminate hands before inserting indwelling urinary catheters, peripheral vascular catheters, or other invasive devices that do not require a surgical procedure. F. Decontaminate hands What cues inform the learner that there is a problem, the step is done, or a different step is needed? Defines “hand hygiene”: A general term that applies to either hand washing, antiseptic handwash, antiseptic hand rub, or surgical hand antisepsis. The following cues indicate that the learner has completely the task: A. When decontaminating hands with an alcohol-based hand rub, apply product to palm of one hand and rub hands together, covering all surfaces of hands and fingers, until hands are dry. B. When washing hands with soap and water, wet hands first with water, apply an amount of product recommended by the manufacturer to hands, and rub hands together vigorously for at least 15 seconds, covering all surfaces of the hands and fingers. Rinse hands with water and dry thoroughly with a disposable towel. Use towel to turn off the faucet. Avoid using hot water, because repeated exposure to hot water may increase the risk of dermatitis. C. Liquid, bar, leaflet or powdered forms of plain soap are acceptable when washing hands with a non-antimicrobial soap and water. When bar soap is used, after contact with a patient’s intact skin (e.g., when taking a pulse or blood pressure, and lifting a patient). soap racks that facilitate drainage and small bars of soap should be used. G. Decontaminate hands after contact with body fluids or excretions, mucous membranes, nonintact skin, and wound dressings if hands are not visibly soiled. H. Decontaminate hands if moving from a contaminated-body site to a clean-body site during patient care. I. Decontaminate hands after contact with inanimate objects (including medical equipment) in the immediate vicinity of the patient. J. Decontaminate hands after removing gloves. K. Before eating and after using a restroom, wash hands with a nonantimicrobial soap and water or with an antimicrobial soap and water. Task #2 How to properly handle linen. What does the learner do? List the guidelines for What does the learner need to know to do this step? Linen and equipment will be What cues inform the learner that there is a problem, the step is done, or a different step is needed? Learner explains when to use handling linen and equipment. separated into “clean” and “dirty,” or contaminated, categories. personal protective equipment when handling linen and equipment. Guidelines for handling linen and equipment include: 1. Wearing gloves when handling soiled linens. 2. Holding and carrying dirty linen away from you. 3. Not shaking dirty linens or clothes. 4. Placing linen and equipment in proper containers. 5. Not touching the inside of disposal containers, etc. Learner demonstrates the proper guidelines when handling linen and equipment. Task #3 When and how to use personal protective equipment (PPE) gloves as a barrier for bodily fluids. What does the learner do? Defines personal protective equipment, and is able to demonstrate the proper method of donning and removing non-surgical gloves in a non-sterile environment. What does the learner need to know to do this step? Gloves are used to prevent contamination of healthcare personnel hands when; 1) anticipating direct contact with blood or body fluids, mucous membranes, non-intact skin and other potentially infectious material; 2) having direct contact with patients who are colonized or infected with pathogens transmitted by the contact route handling or touching visibly or potentially contaminated patient care equipment and environmental surfaces. Gloves can protect both patients and healthcare What cues inform the learner that there is a problem, the step is done, or a different step is needed? The learner employs safe work practices when donning and removing gloves as a PPE. Cue 1. Learner demonstrates proper donning and removal of gloves. Cue 2. Learner employs safe work practices before donning and after the removal of the gloves. SAFE WORK PRACTICES 1. Keep hands away from face Work from clean to dirty 2. Limit surfaces touched personnel from exposure to infectious material that may be carried on hands. Non-sterile disposable medical gloves made of a variety of materials (e.g., latex, vinyl, nitrile) are available for routine patient care. The selection of glove type for non-surgical use is based on a number of factors, including the task that is to be performed, anticipated contact with chemicals and chemotherapeutic agents, latex sensitivity, sizing, and facility policies for creating a latexfree environment. For contact with blood and body fluids during non-surgical patient care, a single pair of gloves generally provides adequate barrier protection. During patient care, transmission of infectious organisms can be reduced by adhering to the principles of working from “clean” to “dirty”, and confining or limiting contamination to surfaces that are directly needed for patient care. It may be necessary to change gloves during the care of a single patient to prevent crosscontamination of body sites. It also may be necessary to change gloves if the patient interaction also involves touching portable computer keyboards or other mobile equipment that is transported from room to room. Discarding gloves between 3. Change gloves when torn or heavily contaminated. 4. Gloves disposed of in closed patient trash receptacle. 5. Perform hand hygiene prior to donning and after removal of gloves. patients is necessary to prevent transmission of infectious material. Gloves must not be washed for subsequent reuse because microorganisms cannot be removed reliably from glove surfaces and continued glove integrity cannot be ensured. When gloves are worn in combination with other PPE, they are put on last. Gloves that fit snugly around the wrist are preferred for use with an isolation gown because they will cover the gown cuff and provide a more reliable continuous barrier for the arms, wrists, and hands. Gloves that are removed properly will prevent hand contamination. Hand hygiene following glove removal further ensures that the hands will not carry potentially infectious material that might have penetrated through unrecognized tears or that could contaminate the hands during glove removal. DONNING PPE GLOVES ■ Use non-sterile for isolation ■ Select according to hand size ■ Extend to cover wrist of isolation gown. (See figure 1) Figure 1. REMOVING PPE Remove PPE at doorway before leaving patient room or in anteroom. GLOVES ■ Outside of gloves are contaminated! ■ Grasp outside of glove with opposite gloved hand; peel off ■ Hold removed glove in gloved hand ■ Slide fingers of ungloved hand under remaining glove at wrist (see figure 2). Figure 2. Task #4 When and how to clean / disinfect equipment between patients. What does the learner do? Discuss Transmission-Based Precautions and Respiratory Hygiene & Cough Etiquette. What does the learner need to know to do this step? A combination of measures designed to minimize the transmission of respiratory pathogens via droplet or airborne routes in healthcare What cues inform the learner that there is a problem, the step is done, or a different step is needed? When the learner successfully demonstrates the components of Respiratory Hygiene/Cough etiguette. settings. The components of Respiratory Hygiene/Cough Etiquette are 1) covering the mouth and nose during coughing and sneezing, 2) using tissues to contain respiratory secretions with prompt disposal into a notouch receptacle, 3) offering a surgical mask to persons who are coughing to decrease contamination of the surrounding environment, and 4) turning the head away from others and maintaining spatial separation, ideally >3 feet, when coughing. These measures are targeted to all patients with symptoms of respiratory infection and their accompanying family members or friends beginning at the point of initial encounter with a healthcare setting. References: Centers for Disease Control and Prevention. Guideline for Hand Hygiene in Health-Care Settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR 2002; 51 (No. RR-16), pp. 1-56. Siegel JD, Rhinehart E, Jackson M, Chiarello L, and the Healthcare Infection Control Practices Advisory Committee, 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (p. 50-51) Wegner, S. Hartman Publishing Inc., n.d., PowerPoint, Infection Control, Chapter 6 SNAC-04