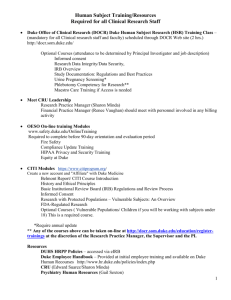
Duke University Medical Center
advertisement

Visiting Fellowship in Transcranial Magnetic Stimulation January 28-29, 2012; April 28-29, 2012; July 21-22, 2012; October 27-28, 2012 Duke University Medical Center Bryan Research Building – 3rd Floor Conference Room 301B Sponsored by the Duke University School of Medicine and the North Carolina Psychological Association Course Description The course, sponsored by the Duke University School of Medicine and the North Carolina Psychological Association, includes hands-on administration of Transcranial Magnetic Stimulation (TMS). In October 2008, the FDA approved TMS for treatment of major depression. Didactic sessions with the TMS faculty of Duke University and Columbia University cover all topics relevant to running a TMS clinical service and a TMS research lab, including: new developments in motor threshold determination, treatment technique, stimulus dosing, risks, complications and contraindications, safety screening and concurrent medications, post TMS management and continuation treatment, clinical and non-clinical research applications, TMS research study designs, and emerging brain stimulation techniques (e.g., magnetic seizure therapy). Target Audience This activity is designed for psychiatrists, psychologists, and researchers who wish to enhance their knowledge of TMS and the related brain stimulation techniques. Learning Objectives At the conclusion of this activity, participants should be able to: State the rationale for the use of TMS in depression, anxiety disorders, and schizophrenia based on current and previous research on the topics Compare and contrast two differences in cortical excitability and implications for depression, anxiety disorders, and schizophrenia Apply the FDA indication for use of TMS in a clinical setting Name the two main components of transcranial magnetic stimulation devices Operate the TMS device and correctly use it to determine the motor threshold and optimal site of two participants Design a screening protocol to evaluate for TMS contraindications and a seizure protocol for management of patients during TMS administration Registration The course is open to physicians, researchers and other professionals and trainees, from the U.S. and abroad. This program is sponsored by the Duke University School of Medicine and the North Carolina Psychological Association. The course registration fee is $1,500 and it is payable by check or online credit card (fee applies). Fee may be waived for full-time Duke faculty and trainees, please inquire when registering. Payment is due by one month before the course start date. A written notice of cancellation must be received 30 days prior to the start of this activity. A 10% cancellation fee will be assessed at that time; after that date, cancellation requests cannot be honored. Please contact Rosa Jou-Zhang at rosa.jouzhang@duke.edu or 919-681-6165 for more information. 1 Accreditation The Duke University School of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. Credit Designation The Duke University School of Medicine designates this live activity for a maximum of 14 AMA PRA Category 1 Credit(s)TM. Physicians should only claim credit commensurate with the extent of their participation in the activity. How to Receive CME Credit In order to receive CME credit, participants must sign-in, review the CME information (accreditation, learning objectives, faculty disclosures, etc.) and attend the CME activity. Participants should also complete the activity evaluation form and return it to the appropriate representative following the CME activity. Continuing Education Statement The Visiting Fellowship in TMS is co-sponsored by the North Carolina Psychological Association and the Duke University School of Medicine. The North Carolina Psychological Association is approved by the American Psychological Association to sponsor continuing education for psychologists. The North Carolina Psychological Association maintains responsibility for this program and its content. This program is offered for 14 hours of continuing education credit. Attendance Requirements To receive credit, you must be present for the entire 2 days and you must sign the sign-in and sign-out sheets each day. No credit will be given to participants who are more than 15 minutes late at the beginning of the morning and afternoon sessions. No credit will be given to participants who leave before the close of the 2-day fellowship Staff and Content Validation Reviewer Disclosure The staff involved with this activity and any content validation reviewers of this activity have reported no relevant financial relationships with commercial interests. Resolution of Conflicts of Interest In accordance with the ACCME Standards for Commercial Support of CME, the Duke University School of Medicine implemented mechanisms, prior to the planning and implementation of this CME activity, to identify and resolve conflicts of interest for all individuals in a position to control content of this CME activity. Planning Committee/Faculty Disclosure The following speakers and/or planning committee members have indicated they have no relationship(s) with industry to disclose relative to the content of this CME activity: Franziska M. Korb, PhD Bruce M. Luber, PhD Antonio Mantovani, MD, PhD Angel V. Peterchev, PhD The following speaker/planning committee member has indicated that s/he has relationship(s) with industry to disclose: Andrew Krystal, MD serves as Principal Investigator for Abbott Laboratories, GSK, Merck, Pfizer, Philips Medical Systems, Sepracor, Takeda, Cephalon, Somaxon; serves as consultant for Abbott Laboratories, Eli Lilly, Philip Medical Systems, Sepracor, Takeda, Somaxon; serves as an Advisory Board Member for GSK, Merck, Pfizer, Sanofi-Aventis, Cepahlon 2 Sarah H. Lisanby, MD serves as Principal Investigator for Magstim, Magventure, Brainsway, Cyberonics, Neuronetics, ANS/St. Jude Medical Disclaimer The information provided at this CME activity is for continuing medical education purposes only and is not meant to substitute for the independent medical judgment of a physician relative to diagnostic and treatment options of a specific patient’s medical condition. Unapproved Use Disclosure Duke School of Medicine requires CME faculty (speakers) to disclose to attendees when products or procedures being discussed are off-label, unlabeled, experimental, and/or investigational (not FDA approved); and any limitations on the information that is presented, such as data that are preliminary or that represent ongoing research, interim analyses, and/or unsupported opinion. This information is intended solely for continuing medical education and is not intended to promote off-label use of these medications. If you have questions, contact the medical affairs department of the manufacturer for the most recent prescribing information. Faculty will be discussing information about pharmaceutical agents that is outside of U.S. Food and Drug Administration approved labeling. The following off-label uses are discussed: TMS for depression in patients who has failed to respond to more than a single medication trial, and use of TMS in the treatment of other psychiatric disorders (e.g. bipolar disorder, anxiety disorders, and schizophrenia). Faculty Sarah H. Lisanby, MD – Activity Medical Director Chair, Department of Psychiatry and Behavioral Sciences Duke University lisan001@win.duke.edu 919-684-5616 Dr. Lisanby earned her BS in mathematics and psychology magna cum laude at Duke University and her MD at Duke University School of Medicine in Durham, North Carolina. After graduating, she completed a residency in psychiatry at Duke University Medical Center, where she served as Executive Chief Resident. Her postdoctoral fellowship in affective disorders research and geriatric psychiatry was conducted at Columbia University. After serving as Brain Stimulation Division Director at Columbia University, she became chair of psychiatry at Duke in October 2010. She became a leader in the field of TMS when her research team innovated the use of TMS to perform convulsive therapy – a procedure termed Magnetic Seizure Therapy (MST). Franziska M. Korb, PhD Postdoctoral Associate (Egner Lab) Center for Cognitive Neuroscience Duke University franziska.korb@duke.edu 919-684-1034 Dr. Korb received her Pre-Diploma (B.Sc.) and Diploma (M.Sc.) in Psychology at the University of Leipzig, Germany. For the research she conducted at the Max Planck Institute of Human Cognitive and Brain Sciences Leipzig she earned her PhD in Psychology from the University of Leipzig. Before coming to Duke she worked as a postdoctoral research associate at the Neurology Department of the University Clinic Cologne. Andrew D. Krystal, MD Professor of Psychiatry and Behavioral Sciences Duke University andrew.krystal@duke.edu 919-684-2057 3 Dr. Krystal received his training at the Duke University School of Medicine, finishing in 1987 before doing residency in Psychiatry and Fellowships in Clinical Neurophysiology and Clinical Research Methodology. His focus is on understanding the pathophysiology of sleep disorders and mood disorders and improving the treatment of these conditions. He has published over 150 papers including work on optimizing ECT stimulus intensity, the Neuronetics rTMS trial, and on the effects of TMS on craving for cigarettes. He is Past-President and sits on the Board of Directors of the International Society for ECT and Neurostimulation. He is working with Dr. Lisanby in developing the clinical and clinical research TMS program at Duke. Antonio Mantovani, MD, PhD – Activity Co-Director Associate Research Scientist Columbia University am2518@columbia.edu 212-543-6081 Dr. Mantovani completed medical training at Rome University and psychiatry training at Siena University. Under the mentorship of Dr. Simone Rossi at Siena University, Dr. Mantovani received his PhD in Applied Neurological Sciences. His graduate work focused on neurophysiological correlates of psychiatric disorders. At Columbia University, he designs and conducts open and sham-controlled trials of Transcranial Magnetic Stimulation (TMS) in the treatment of Obsessive Compulsive Disorder, Tourette Syndrome, Panic Disorder, Depersonalization Disorder, and Major Depression. Bruce M. Luber, PhD Associate Professor of Psychiatry and Behavioral Sciences Duke University bruce.luber@duke.edu 919-681-9876 Dr. Luber received his PhD in experimental psychology from NYU, researching spatial attention using magnetoencephalopgraphy (MEG). His post-doctorate work at Columbia University/NY State Psychiatric Institute focused on the electrophysiology of memory and of ECT. He joined Dr. Holly Lisanby in the then new field of transcranial magnetic stimulation (TMS) at Columbia in 1995. With Dr. Lisanby and collaborators he researched the cortical mechanisms underlying working memory, conditioned learning, pain, deception, and self-recognition. His primary focus is on the use of TMS to explore executive function and memory, and its applications to geriatric psychiatry. He was on the faculty at Columbia University until November 2010 when he moved to Duke University. Angel V. Peterchev, PhD Assistant Professor of Psychiatry and Behavioral Sciences, and Biomedical Engineering Duke University angel.peterchev@duke.edu 919-684-0383 Dr. Peterchev received the A.B. degree in physics and engineering sciences from Harvard University in 1999 and the M.S. and Ph.D. degrees in electrical engineering with a graduate-level minor in cognitive neuroscience from the University of California at Berkeley in 2002 and 2005, respectively. He completed postdoctoral training in TMS at Columbia University in 2007, and remained on the faculty there until the end of 2010 when he moved to Duke University. Dr. Peterchev’s current research focuses on the development and modeling of technology and application paradigms for transcranial brain stimulation, including TMS, electroconvulsive therapy (ECT), magnetic seizure therapy (MST), and the integration of TMS with functional magnetic resonance imaging (fMRI) and electroencephalography (EEG). The ultimate clinical goal of his work is to make transcranial stimulation techniques robustly effective and safe. For more information or to register, please contact Rosa Jou-Zhang rosa.jouzhang@duke.edu Ph: 919-681-6165 Fax: 919-681-9962 4 or visit the Duke CME website at http://cmetracker.net/DUKE/Courses.html TMS CME AGENDA Day Saturday Time Event Faculty Location 8:30-9:00 am Breakfast BRB – Rm 301B 9:00-10:00 am TMS as tool in Neuroscience SHL BRB – Rm 301B 10:00-11:00 am Treatment technique-Stimulus Dosing-Study Design SHL BRB – Rm 301B BREAK Regulatory Statements: IRB, IDE, FDA, Guidelines11:00-11:30 am SHL BRB – Rm 301B ISTS consensus statement 11:30-12:30 pm Magnetic Seizure Therapy (MST) SHL BRB – Rm 301B 12:30-1:30 pm Lunch Break 1:30-2:30 pm Mechanisms of action: Physics of TMS AVP BRB – Rm 301B 2:30-3:30 pm TMS and Motor Cortex Excitability AM BRB – Rm 301B BREAK Hands-on: Motor Threshold determination with FMK/AM BRB – Rm 359/361 research device + Robot Arm Exhibit 3:30-5:00 pm Hands-on: Motor Threshold determination with ADK Erwin Sq, St 340 clinical device Sunday Breakfast Hands-on: TMS device set-up and motor threshold practice with research device 9:00-11:00 am Hands-on: TMS device set-up and motor threshold practice with clinical device 11:00-12:00pm Use of Imaging in TMS 12:00-1:00 pm Lunch Break 1:00-2:30 pm TMS and Mood Disorders 2:30-3:30 pm TMS and Anxiety Disorders and Schizophrenia BREAK Risks, Complications and Contraindications-Safety 3:30-4:00 pm Screening and Concurrent Medications; Post TMS Management-Continuation Treatment General Discussion, Q&A, Course Wrap-up and 4:00-5:00 pm Completion of Course Evaluation BRB – Rm 301B 8:30-9:00 am Faculty Key SHL: Sarah H. Lisanby, MD BML: Bruce M. Luber, PhD AVP: Angel V. Peterchev, PhD AM/BML BRB – Rm 359/361 ADK Erwin Sq, St 340 BML BRB – Rm 301B AM AM BRB – Rm 301B BRB – Rm 301B AM BRB – Rm 301B SHL/AM BRB – Rm 301B AM: Antonio Mantovani, MD, PhD ADK: Andrew D. Krystal, MD FMK: Franziska M. Korb, PhD Locations: Bryan Research Building (BRB) 3rd Floor Conference Room #301B 311 Research Drive Durham, NC 27710 Link to Map: http://www.map.duke.edu/search?q=bryan+research+building Erwin Square Tower 2200 West Main Street, Suite 340 Durham, NC 27705 Link to map: http://maps.duke.edu/building/241 5