Protecting-bone-marrow-through-gene-therap
advertisement
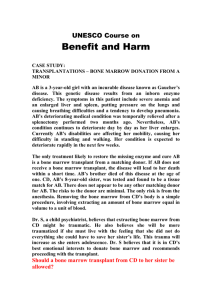
Protecting bone marrow through gene therapy from the toxic side effects of chemotherapy “For the first time in Australia, gene therapy will be used in paediatric oncology”, said Minister for Health, Minister for Medical Research, Jillian Skinner. “Thanks to $3 m of funding from The Kids’ Cancer Project since 2005 and support from other donors, a clinical trial will begin at The Children’s Hospital at Westmead using a gene to protect children’s bone marrow during aggressive chemotherapy to treat lethal brain tumours,” said Ms Skinner. “It has taken 14 years for the research to reach clinical trial stage The clinical trial will aim to test a strategy for protecting the child’s bone marrow so higher doses of chemotherapy can be administered, “she said. Children who will be eligible for the trial have a very poor prognosis and will have exhausted all other conventional treatment options. “Brain tumours in children are very difficult to treat because temezolomide, the chemotherapy drug that is used, has very toxic side effects and can destroy healthy bone marrow cells, leaving the child susceptible to infections. Higher doses could be more effective in treating these lethal tumours, but the drugs are too toxic for young patients, making it difficult to eradicate tumours.” said oncology specialist Dr Geoff McCowage, “We are optimistic, but cautious, and this is the first step along a difficult road” said Professor Ian Alexander, Head of the Gene Therapy Unit. “This is a Phase one trial, where we aim to establish the safety and feasibility of the gene therapy. We can’t be sure patients will benefit, although we hope they will. This is an important platform for building capacity for the future. It will have benefits for other paediatric conditions involving bone marrow. “ The strategy being tested to treat the patients involves gene therapy, which is a process where a specific gene is inserted into a patient’s cells to potentially provide a therapeutic benefit. For this study, the specific gene is for Methyl-guanine Methyl-tranferase (MGMT), a protein that can protect bone marrow cells from temozolomide. Bone marrow has low levels of MGMT while brain tumour cells can have high levels. The aim is to increase the level of MGMT in bone marrow, so higher doses of chemotherapy can be given to the child. The clinical trial will add an MGMT gene delivery solution to harvested blood cells. The solution contains an artificial virus, called a vector, which cannot replicate itself and create new viruses, but can deliver the MGMT gene to the cells. The genetically modified cells are then given back to the patient. The hope is that the genetically modified cells will function in the bone marrow and will increase in number so that when treated with temozolomide, the bone marrow will be protected and higher doses can be given. This could both reduce the side effects of chemotherapy and more effectively treat tumours. “The Government is proud of the support that research provides the health and medical sector in NSW,” said Ms Skinner. The start of the trial represents the bringing together of expertise from across a number of clinical and research areas, through a long-term collaboration between the Oncology Department, Children’s Cancer Research Unit and the Gene Therapy Unit. Now the research outcomes can be translated into clinical practice. The Kids Research Institute at The Children’s Hospital at Westmead has a state of the art cleanroom facility dedicated to gene and cellular therapies for children. This is where the gene transfer vector was produced, and where the patient’s bone marrow cells will be treated. . The Children's Cancer Research Unit, part of the Kids Research Institute, the Hospital’s research arm, undertakes basic, clinical and translational cancer research, focussing on childhood and adolescent tumours which have a poor prognosis. The Unit is the research-dedicated arm of the clinical Oncology Department. The Gene Therapy Unit, a joint initiative with the Children’s Medical Research Institute, focuses on the development of novel gene-based strategies for the treatment of genetic conditions effecting children. Since the very beginning of the research program, The Kids’ Cancer Project (formerly Oncology Childrens Foundation) has contributed the majority of the funding to establish this trial. Their ongoing commitment to supporting the trial will ensure that many years of research effort will successfully be translated into a clinical setting early in 2012. The Sporting Chance Foundation, Westfield, Radpharm, and the NSW State Government and Federal Government have also contributed funds.