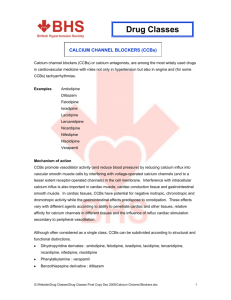
Calcium channel blockers
advertisement

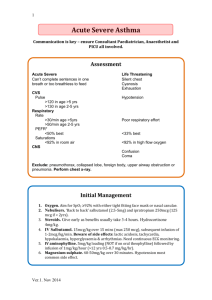
Calcium channel blockers: Toxicity from organic calcium channel antagonists (CCAs) causes a decrease in mechanical contraction of heart and smooth muscle. Severe toxicity produces hypodynamic shock, characterized by bradycardia and hypotension and often accompanied by metabolic acidosis. Because CCAs interfere with normal signaling of stimulatory hormones in the cardiovascular system, standard cardiotonic and vasopressor treatments for hypotension often produce ineffective or minimal effects in patients with severe toxicity. Classification of Ca2+ Channel Antagonists Chemical Class Phenylalkylamines Benzothiazepines Dihydropyridines Drug Verapamil Diltiazem Amlodipine Felodipine Isradipine Nicardipine Nifedipine Nimodipine Nisoldipine Bepridil Diarylaminopropylamine esters The sustained-release and second-generation dihydropyridine CCA preparations are long-acting drugs, they provide a larger drug dose per tablet (especially in children) and can extend the duration of clinical toxicity, and can lead to a delay in clinical manifestation of toxicity. Pathophysiology: An increase in intracellular calcium causes smooth and cardiac muscle to contract and accelerates impulse formation in cardiac pacemaker cells. Conversely, a deprivation of intracellular calcium causes smooth muscle relaxation, a decrease in cardiac contraction, and a slowing of automaticity. Clinically, these effects are recognized as hypotension, bradycardia, and shock. 1 Verapamil is the most potent negative inotrope of all CCAs, causing equal depression of heart contraction and increase in smooth muscle dilation at any concentration. Dihydropyridines are selectively relax smooth muscle at concentrations that produce less negative inotropy. Second-generation drugs are more lipid soluble and have longer duration of action. These drugs cause a more gradual smooth muscle relaxation, producing less reflex tachycardia than is observed with first-generation dihydropyridines. Clinical presentation: CCAs generally produce hypotension with a slow heart rate, CCAs produce bradycardia by decreasing sinus node firing, leading to sinus arrest. Dihydropyridines are well recognized to produce reflex increases in heart rate with an increase in left ventricular stroke volume, leading to an increase in cardiac output at therapeutic and moderate toxic doses. With severe overdose, all CCAs exert a negative inotropic effect with depressed cardiac contraction, conduction block, and hypotension with shock. Other clinical manifestations are organ hypoperfusion, inhibition of metabolic processes, drowsy, Altered mental status, Pulmonary edema, Metabolic acidosis with hyperglycemia, The mechanism of hyperglycemia is related to a suppressive effect of CCAs on pancreatic beta cell insulin release coupled with whole-body insulin resistance. Treatment: Treatment of CCA overdose consists of: (1) providing supportive care, (2) decreasing drug absorption, and (3) augmenting myocardial function with cardiotonic agents. 1- supportive care Supportive care consists of airway protection and management, adequate ventilation, and hemodynamic monitoring. Endotracheal intubation may prevent pulmonary aspiration during gastric instillation of charcoal or if vomiting occurs during the administration of glucagon. 2- Decontamination 2 Activated charcoal should be administered after the patient’s airway is secured. In massive overdose, sustained-release preparations can form gastrointestinal concretions (with ileus), which can persist for days, rendering charcoal less useful.[45][60] In this situation, whole-bowel irrigation with polyethylene glycol may accelerate removal of sustained-release CCA pill fragments. CCA elimination half-life is increased in overdose, and toxicity from massive overdose can last for days. 3- Cardiotonic Drugs (1) provide a reasonable crystalloid bolus (10–20 mL/kg), (2) correct acidemia (keep arterial pH above 7.30 by hyperventilation or with sodium bicarbonate infusion), and (3) correct hyperkalemia (>5.0 mEq/L), preferably with insulin infusion. Calcium salts are the first-line treatment of CCA overdose.[51] Calcium chloride should be initiated as a 10- to 20-mg/kg bolus injection. If this infusion improves heart rate, myocardial conduction, arterial blood pressure, or urine production, then a constant infusion of calcium chloride at 20 to 50 mg/kg/hr should be initiated. Ionized plasma calcium concentrations should be maintained between 2.0 and 3.0 mEq/L. Calcium should not be used if concomitant cardiac glycoside (e.g., digoxin) toxicity is possible. If calcium produces an inadequate clinical response, glucagon should be given in a 0.05- to 0.20-mg/kg bolus infusion. If a benefit is observed, usually within 5 minutes, a constant infusion of glucagon should be initiated, starting at 0.05 to 0.1 mg/kg/hr. Atropine administration is acceptable in the patient initially presenting with bradycardia and hypotension. Catecholamines are the next treatment for refractory CCA overdose. Dopamine can be used in standard doses for cardiogenic shock (10–20 μg/kg/min). Epinephrine has also shown benefit in CCA-intoxicated humans and animals. However, it was found recently that epinephrine worsened myocardial function and did not improve survival compared with saline treatment. The phosphodiesterase inhibitor amrinone has successfully treated refractory CCA hypotension. Insulin apparently improves myocardial 3 mechanical efficiency and contractility by accelerating carbohydrate oxidation and lower plasma potassium concentrations, thereby indirectly improving automaticity and conduction. Serum potassium and glucose levels should be monitored during and after the insulin therapy is stopped. For patients with cardiogenic shock that is refractory to the above treatments, Electrical cardiac pacing may help restore heart rate and should be considered for patients with shock and a heart rate below 40 beats per minute. 4