P127 Diagnosing Tuberculous Peritonitis Early: A Case Report 0n
advertisement

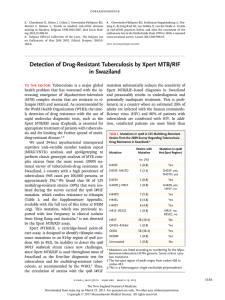
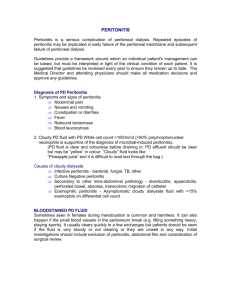
P127 Diagnosing Tuberculous Peritonitis Early: A Case Report 0n Using Xpert MTB/RIF assay Sarah Edwards1, Miruna David2 and Lavanya Kamesh1 1 Renal Unit, 2 Department of Microbiology, Queen Elizabeth Hospital, Birmingham Background: Patients from ethnic minority groups on renal replacement therapy are at increased risk of tuberculosis (TB). Reports suggest rates 70-100 fold greater than those in the general population in the UK and the relatively more frequent occurrence of extra-pulmonary disease (1). Reactivation of latent TB often occurs within the first 12 months after initiating dialysis. However, diagnosing active infection can be challenging. Mycobacterial culture remains the gold standard laboratory diagnostic method, but even with modern liquid culture techniques, a positive result may require up to 6-8 weeks of incubation. This delay in diagnosis and treatment can result in increased morbidity and may have infection control implications. The Xpert MTB/RIF assay like other molecular diagnostic techniques can aid in the prompt diagnosis as it detects and amplifies the DNA of Mycobacterium tuberculosis complex and genetic mutations associated with resistance to rifampicin (2). This test is CE-marked for respiratory (sputum and BAL) samples, however there are numerous studies on its use in extra-pulmonary samples such as lymph node biopsies, cerebrospinal fluid and ascitic fluid. We report a case of tuberculous peritonitis, where a prompt diagnosis was made using the Xpert MTB/RIF assay. Case: A 59 year old Asian lady had been on automated peritoneal dialysis for 7 months when she became unwell. She had a 3 week history of fever, weight loss and poor appetite and subsequently developed cloudy PD fluid. Her peritonitis was treated empirically with intra-peritoneal vancomycin but she continued to have fevers. A CT scan showing lymphadenopathy increased the suspicion of TB, but the lymph node biopsy was inconclusive. Repeated microscopy of the PD fluid showed a leucocytosis, but acid fast bacilli (AFB) smear was negative. Whilst TB culture was in progress, PCR testing of the PD fluid yielded M. tuberculosis DNA with no evidence of mutation for rifampicin drug resistance. This rapid diagnosis allowed early treatment with anti-TB therapy. Fully sensitive TB was not cultured from the PD fluid until day 20. Her symptoms resolved with treatment, although her PD catheter was removed 4 months later due to bacterial peritonitis. Conclusion: This case highlights the usefulness of new molecular assays in reaching an early diagnosis of TB peritonitis, preventing further delays in treatment. This type of PCR testing may be beneficial in the early detection of TB peritonitis although studies into the sensitivity and specificity in PD patients are needed to inform future peritonitis guidelines. ? Clinicians should consider testing by a molecular method for presence of MTB infection culture-negative peritonitis cases in patients at risk of TB. References: 1. High rates of tuberculosis in end-stage renal failure; the impact of international migration. Moore DA, Emerg Infect Dis 2002 Jan;8(1):77-8 2. Availability of an assay for detecting Mycobacterium tuberculosis, including rifampicin-resistant strains and considerations for its use-United States 2013. Centres for disease Control, MMWR Morb Mortal Wkly Rep 2013 Oct 18; 62(41):821-7