AppendixPeriton FÖ
advertisement

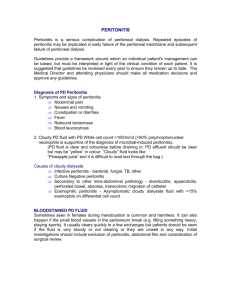
The Pathology of Appendix and Peritoneum The Pathology of Appendix Appendix The vermiform appendix, which is usually 8 to 10 cm Has a retrocecal attachment to the cecum, move freely. The wall of the appendix is composed of the same layers as the rest of the intestine. The most prominent microscopic feature is the predominance of submucosal lymphoid tissue. Acute Appendicitis This condition is by far the most common disease of the appendix Most frequent cause of an abdominal emergency An inflammatory disease of the wall of the vermiform appendix that leads to transmural inflammation and perforation and peritonitis Right lower quadrant syndrome Etiology: Obstruction of its orifice (50 to 80%) – Fecalith / Solid fecal material (50%) – Hyperplastic lymphoid tissue [bacterial or viral infection (e.g., by Salmonella or measles)] – Tumor – Ball of pinworms (Enterobius vermicularis) – Foreign body (e.g., gallstone) Pathogenesis: – – – – – – – Continued mucinous secretion Progressive increase in intraluminal pressure Increased venous pressure Ischemic injury Mucosal ulceration Invasion by intestinal bacteria Additional inflammatory edema and exudation (neutrophil accumulation acute suppurative inflammation) – Gangrene Pathology The appendix is congested, tense, and covered by a fibrinous exudate. Its lumen often contains purulent material. Earliest stage: – Normal glistening serosa a dull, granular, red membrane – A scant neutrophilic exudate – Congestion Later stage: – A prominent neutrophilic exudate – Foci of suppurative necrosis in the mucosa – Fibrinopurulent reaction over the serosa – Abscess formation within the wall, along with ulcerations – Acute suppurative appendicitis Acute gangrenous appendicitis – Large areas of hemorrhagic green ulceration of the mucosa – Green-black gangrenous necrosis through the wall, extending to the serosa, – Rupture (perforation) Suppurative peritonitis perforation of the wall releases the luminal contents into the peritoneal cavity Complications Periappendiceal abscesses (anywhere in the abdominal cavity) Fistulous tracts (the small and large bowel, bladder, vagina, or abdominal wall) Superior mesenteric vein syndrome – Pylephlebitis (thrombophlebitis of the intrahepatic portal vein) – Secondary hepatic abscesses Perforation and diffuse peritonitis Septicemia Wound infection after surgery – in patients with perforation and periappendiceal abscess Mucocele A dilated mucus-filled appendix (bag of mucus) Etiology: – Neoplastic mucin-producing adenoma (mucinous cystadenoma) mucinous cystadenocarcinoma – Non-neoplastic chronic obstruction Complications Infection Rupture (perforation) – discharging mucin and debris into the peritoneum localized collections of mucus attached to the serosa (without tumor cells) Pseudomyxoma peritonei – Cystadenoma or Cystadenocarcinoma perforation seeding of the peritoneum by mucus-secreting tumor cells In less than one third of cases, pseudomyxoma peritonei is caused by disease of the appendix In half, it originates from ovarian mucinous cystadenocarcinoma Tumors Carcinoid – Common – Small ones do not metastasize they do if they are over 1.5 cm, which is very rare The Pathology of Periton The peritoneum is the mesothelial lining of the abdominal cavity and its viscera Peritonitis Peritonitis results in an acute abdomen Classification and Etiology Bacterial peritonitis – – – – Perforation (appendicitis, cholecystitis, diverticulitis, salpingitis, ect.) Ileus (intestinal obstruction, blunt abdomial trauma) Iatrogenic (surgery: infected surgical instruments&environment) Penetrating wounds (bullet, knife, stab, blown from an explosion, falling on a sharp object) – Bacterial invasion of ascites (spontaneous bacterial peritonitis) Chemical peritonitis – Sterile (bile) peritonitis: perforated gallbladder needle biopsy of the liver – Perforated peptic ulcer (stomach or duodenum) Hydrochloric acid Hemorrhage – Acute hemorrhagic pancreatitis release and activation of potent lipolytic and proteolytic enzymes Severe peritonitis and fat necrosis Globules of free fat may be found floating in the peritoneal fluid, and bacterial permeation of the bowel wall leads to a frank suppurative exudate after 24 to 48 hours. – Chemicals introduced by surgery Talc Some chemical in the dialysate Gynecologic conditions – Endometriosis (blood into the peritoneal cavity) – Ruptured dermoid cysts (peritoneal granulomatous reaction) Pathogenesis PERFORATION – Inflamed appendix – Peptic ulcer – Colonic diverticulum – Cholecystitis – Strangulation of bowel – Acute salpingitis Acute abdomen – Severe abdominal pain and tenderness – Nausea, vomiting, and a high fever – Severe cases generalized peritonitis, paralytic ileus, and septic shock – Often the perforation becomes “walled off” in which case a peritoneal abscess results. Origin of organisms: – GIS: E. coli, streptococci, Staphylococcus aureus, enterococci, gram-negative rods, Clostridium perfringens – Genital system: gonococcus and Chlamydia CHRONIC PERITONEAL DIALYSIS Contamination of instruments or dialysate Staphylococci, Streptococci One fourth of cases are aseptic Caused by some chemical in the dialysate SPONTANEOUS BACTERIAL PERITONITIS No appearent cause (such as a perforated viscus) Risk factors: Ascites – Cirrhosis (adults): enteric bacilli – Nephrotic syndrome (children): urinary tract infections TUBERCULOUS PERITONITIS An uncommon site of extrapulmonary TB infection Risk factors: – – – – Cirrhosis HIV infection Diabetes mellitus Malignancy (treatment with TNF agents) Pathogenesis: – – – – Reactivation of latent tuberculous foci Hematogenous spread Infected small intestine Tuberculous salpingitis Pathology A fibrinopurulent exudate covers the surface of the intestines Organization of exudate adhesions (between loops of bowel) – adhesions may be lysed – may lead to volvulus and intestinal obstruction Bacterial salpingitis – Gonococcal – may lead to pelvic peritonitis and adhesions pelvic inflammatory disease Familial Paroxysmal Polyserositis (Familial Mediterranean Fever - FMF) Peritonitis and Amyloidosis Inherited autosomal recessive disorder Recurrent episodes of aseptic peritonitis with fever and abdominal pain Arthritis and pleuritis at some time The disease predominates in Sephardic Jews and other Mediterranean populations, such as Armenians, Turks, and Arabs The pathogenesis of FMF remains obscure Retroperitoneal Fibrosis Dense fibromatous overgrowth of the retroperitoneal tissues Sclerosing retroperitonitis or idiopathic retroperitoneal fibrosis (also called Ormond disease). Uncommon Fibrosing condition of the abdomen, becomes symptomatic when it causes obstruction of the ureters Inflammatory infiltration (lymphocytes, plasma cells, and neutrophils) Hydronephrosis Cystic Lesions and Neoplasms of the Peritoneum Mesenteric and Omental Cysts – Large to small cystic masses (1) arising from sequestered lymphatic channels (mesenteric and omental cysts are usually of lymphatic origin) (2) derived from pinched-off enteric diverticula of the developing foregut and hindgut (3) derived from the urogenital ridge or its derivatives (i.e., the urinary tract and male and female genital tracts) (4) derived from walled-off infections or following pancreatitis, more properly called pseudocysts (5) malignant origin (intra-abdominal adenocarcinomas) – Complications: rupture bleeding torsion intestinal obstruction Primary tumors Mesotheliomas Most common primary peritoneal tumor Asbestos exposure (80%) The pathologic characteristics of peritoneal mesotheliomas are identical to those of their pleural counterparts Secondary tumors Metastatic Carcinoma Quite common Ovarian and pancreatic cancers – penetration to the serosal membrane or metastatic seeding (peritoneal carcinomatosis) Appendiceal mucinous carcinomas – pseudomyxoma peritoneii Extra-abdominal locations – may be implicated in peritoneal seeding