January 2013 - Management of Fibromyalgia Syndrome
advertisement
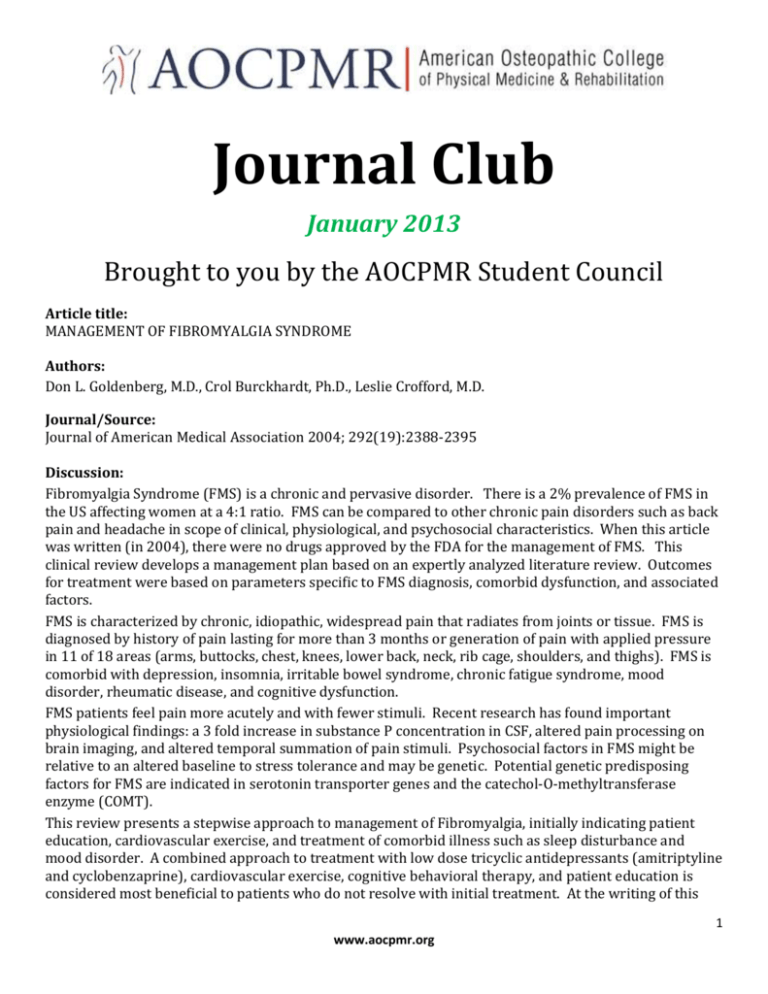
Journal Club January 2013 Brought to you by the AOCPMR Student Council Article title: MANAGEMENT OF FIBROMYALGIA SYNDROME Authors: Don L. Goldenberg, M.D., Crol Burckhardt, Ph.D., Leslie Crofford, M.D. Journal/Source: Journal of American Medical Association 2004; 292(19):2388-2395 Discussion: Fibromyalgia Syndrome (FMS) is a chronic and pervasive disorder. There is a 2% prevalence of FMS in the US affecting women at a 4:1 ratio. FMS can be compared to other chronic pain disorders such as back pain and headache in scope of clinical, physiological, and psychosocial characteristics. When this article was written (in 2004), there were no drugs approved by the FDA for the management of FMS. This clinical review develops a management plan based on an expertly analyzed literature review. Outcomes for treatment were based on parameters specific to FMS diagnosis, comorbid dysfunction, and associated factors. FMS is characterized by chronic, idiopathic, widespread pain that radiates from joints or tissue. FMS is diagnosed by history of pain lasting for more than 3 months or generation of pain with applied pressure in 11 of 18 areas (arms, buttocks, chest, knees, lower back, neck, rib cage, shoulders, and thighs). FMS is comorbid with depression, insomnia, irritable bowel syndrome, chronic fatigue syndrome, mood disorder, rheumatic disease, and cognitive dysfunction. FMS patients feel pain more acutely and with fewer stimuli. Recent research has found important physiological findings: a 3 fold increase in substance P concentration in CSF, altered pain processing on brain imaging, and altered temporal summation of pain stimuli. Psychosocial factors in FMS might be relative to an altered baseline to stress tolerance and may be genetic. Potential genetic predisposing factors for FMS are indicated in serotonin transporter genes and the catechol-O-methyltransferase enzyme (COMT). This review presents a stepwise approach to management of Fibromyalgia, initially indicating patient education, cardiovascular exercise, and treatment of comorbid illness such as sleep disturbance and mood disorder. A combined approach to treatment with low dose tricyclic antidepressants (amitriptyline and cyclobenzaprine), cardiovascular exercise, cognitive behavioral therapy, and patient education is considered most beneficial to patients who do not resolve with initial treatment. At the writing of this 1 www.aocpmr.org article, RCTs for SNRIs were underway and results for these trials are anticipated. Currently, the SNRIs duloxetine and milnacipran, along with the anticonvulsant, pregabalin, are FDA approved medications for FMS. The stepwise plan is based on treatment efficacies as found by literature review. Outcomes of treatment across studies were accumulated mainly by self-assessment using tools such as the FIQ (Fibromyalgia Impact Questionnaire, which measures physical functioning, work status, depression, anxiety, sleep, pain, stiffness, fatigue, and well-being); clinical assessment using manual tenderpoint assessment, dolorimetry (measures threshold and tolerance), and exercise fitness was also utilized. The functionality of FMS patients correlates with their ability to self-manage pain. Some successful treatments, such as CBT and education, address functionality directly and it is interesting to note their impact reported on pain. Pharmacological treatment seemed to have greater effect on peripheral symptomology and it is ironic that in FMS using non-medicinal therapy to reduce pain and drug therapy to treat comorbid symptoms is indicted. Here is a summary of significant effects of the recommended and FDA approved treatments: Patient education improved pain, sleep, fatigue, self-efficacy, quality of life, and 6-minute walk. Cardiovascular exercise was significant for terderpoint pain pressure threshold and general pain. Cognitive behavioral therapy improved pain, function, fatigue, and mood. Combined therapy (CBT, cardiovascular exercise, and education) improved pain severity, physician rating of disease severity, and FIQ. TCAs improved most clinical outcomes, especially sleep quality. SNRIs improved general FIQ scores. Pregabalin lowered pain severity and was effective at improving general pain in a large percent of patients. A drawback to the research presented as highlighted by the authors is the lack of long term study for this chronic illness. Most pharmacological studies were of 6-12 week duration. Findings for tricyclic antidepressants were based on evidence from short term studies and were shown to lose their effect in one long term study. Another shortcoming is a lack of data from patients comorbid with rheumatic disease, which has a 25-65% comorbidity with FMS (the CDC classifies FMS as a type of arthritis). Future research should examine longer term data, individualized patient prognosis and treatment, and operate within a more stringent definition of what comprises Fibromyalgia. Questions: 1. What would be on a differential diagnosis for an FMS patient? 2. How might psychosocial factors contribute to FMS? 3. What is the difference between amitriptyline and cyclobenzaprine? 4. Why might some FMS patients have better outcomes from certain therapies? 5. What is the argument for a physician who believes sharing an FMS diagnosis with a patient will inhibit treatment? 6. Compare findings for cardiovascular, strength training, and stretching exercises. 7. What is the difference between a clinical review and a literature review? 8. What is the difference between coaggregation and comorbidity? Reviewer: Michael Flamm, OMS-II, NYCOM PM&R Journal Club Chair 2 www.aocpmr.org