Neuroprotection from Hyperammonemia
advertisement

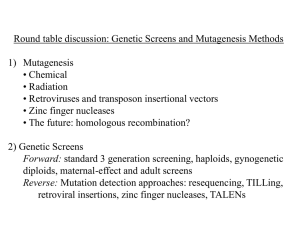
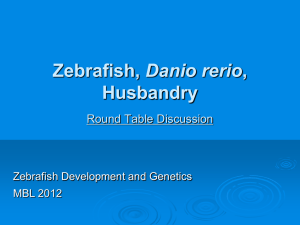
NEUROPROTECTION FROM HYPERAMMONEMIA: SMALL MOLECULE SCREEN Feldman B1, Tuchman M2, Caldovic L2 1 Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda MD, USA; Children’s National Medical Center, Washington DC, USA 2 Hyperammonemia has traditionally been studied in the context of urea cycle defects and liver failure. However it is the exposure of the brain to elevated ammonia that leads to a wide range of neurocognitive deficits, intellectual disabilities and in the most severe cases, coma and death. Although the brain is damaged by hyperammonemia, current treatments focus almost exclusively on reducing ammonia levels through the activation of alternative liver pathways for ammonia disposal or liver transplantation. Our aim is to discover novel drugs that protect the brain from elevated levels of blood ammonia. Ammonia is toxic to all fish and its effects appear to be similar in fish and mammals. Although fish have a complete urea cycle, hyperammonemia can be induced simply by immersing them in water with elevated concentration of ammonia, which is transferred from the water into the blood. In fish hyperammonemia manifests with neurological similarities to humans including hyperventilation, lethargy, convulsions, coma, and death. We developed a zebrafish model of hyperammonemia by immersing 4 days old (dpf) fish in water containing ammonium acetate (AmAc). The LD50 for AmAc in 4 dpf zebrafish was determined by exposing them to increasing concentrations of either AmAc or sodium acetate (control) and monitoring for the cessation of heartbeat as the endpoint. The ability of small molecules to protect 4 dpf zebrafish from ammonia toxicity was determined by exposing them to collections of small molecules dissolved in 10% DMSO followed by addition of AmAc and monitoring whether small molecules prolong survival in AmAc. A screen of NIH Clinical Collections 1 & 2 of 727 compounds with known safety profiles is currently under way. When 4 dpf zebrafish were exposed to increasing concentrations of AmAc, 50% of 4 dpf zebrafish died within 3 hr when exposed to 3 mM AmAc whereas 4 mM AmAc was 100% lethal. Therefore, we used 4 dpf zebrafish exposed to 4 mM AmAc to screen for drugs that increase their survival. We then tested whether glutamine synthetase inhibitor methionine sulfoximine (MSO) and/or NMDA receptor antagonists MK-801, memantine and ketamine, which are known to protect the mammalian brain from hyperammonemia prolong the survival of 4 dpf zebrafish exposed to lethal dose of AmAc. Treatment with MSO, MK-801, memntine or ketamine prolonged the lives of 4 dpf fish exposed to a lethal dose of AmAc. Treatment with the combination of MSO and an NMDA receptor antagonist was more effective than either drug alone. These results demonstrate that zebrafish can be used in a high throughput screen to select ammonia-neuroprotective agents. If successful, drugs that result from this screen would complement current treatment approaches to improve the outcome of patients with hyperammonemia.