MUR Crib Sheet for Anticoagulants
advertisement
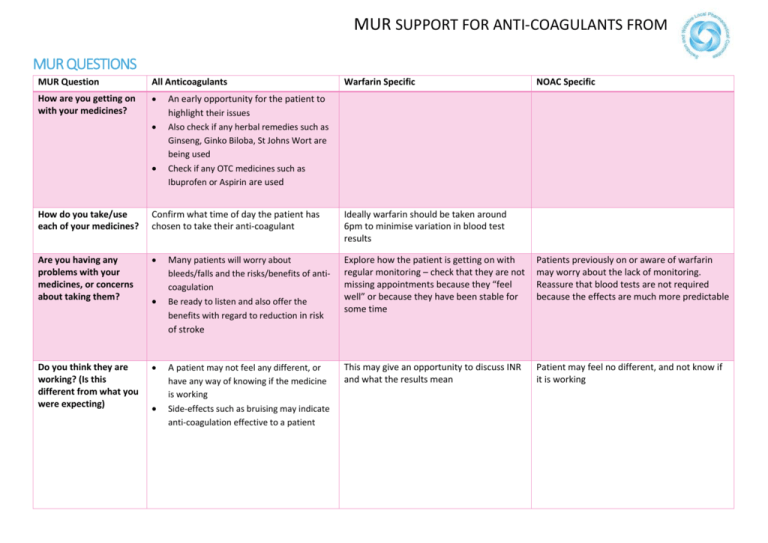
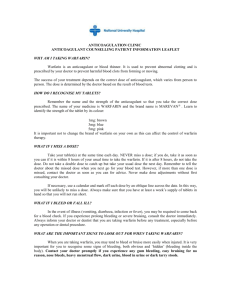
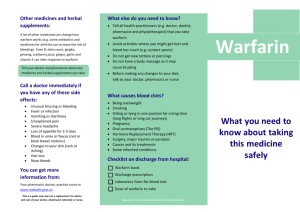
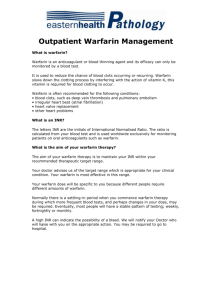
MUR SUPPORT FOR ANTI-COAGULANTS FROM MUR QUESTIONS MUR Question All Anticoagulants How are you getting on with your medicines? Warfarin Specific NOAC Specific An early opportunity for the patient to highlight their issues Also check if any herbal remedies such as Ginseng, Ginko Biloba, St Johns Wort are being used Check if any OTC medicines such as Ibuprofen or Aspirin are used How do you take/use each of your medicines? Confirm what time of day the patient has chosen to take their anti-coagulant Ideally warfarin should be taken around 6pm to minimise variation in blood test results Are you having any problems with your medicines, or concerns about taking them? Many patients will worry about bleeds/falls and the risks/benefits of anticoagulation Be ready to listen and also offer the benefits with regard to reduction in risk of stroke Explore how the patient is getting on with regular monitoring – check that they are not missing appointments because they “feel well” or because they have been stable for some time Patients previously on or aware of warfarin may worry about the lack of monitoring. Reassure that blood tests are not required because the effects are much more predictable Do you think they are working? (Is this different from what you were expecting) A patient may not feel any different, or have any way of knowing if the medicine is working Side-effects such as bruising may indicate anti-coagulation effective to a patient This may give an opportunity to discuss INR and what the results mean Patient may feel no different, and not know if it is working MUR SUPPORT FOR ANTI-COAGULANTS FROM MUR Question All Anticoagulants Do you think you are getting any side-effects or unexpected effects? Bruising more easily or bleeding for longer from minor cuts is normal. Seek medical attention of patient falls, or is injured during treatment – especially if they hit their head (due to increased risk of bleeding) Seek medical help if there is blood in urine or tar coloured stools Anti-coagulants do not cause unexplained bleeds (e.g. nosebleeds) but will make bleeding worse. The cause of the bleeding should be resolved rather than withdrawal of the anti-coagulant It is important to take all anticoagulants regularly at the same time each day Because of the “6pm” rule for warfarin, and the need to take Rivaroxaban with food, 6pm is a good rule of thumb for all anticoagulants unless a different time of day would assist the patient to remember People often miss taking doses of their medicine, for a wide range of reasons. Have you missed any doses of your new medicine, or changed when you take it (prompt: when did you last miss a dose)? Do you have anything else you would like to know about your new medicine, or anything you would like me to go over again? GP should be monitoring renal and liver function annually Warfarin Specific NOAC Specific It is recommended to take warfarin at 6pm each day – this minimises variation in the results of blood tests Never take a “double dose” the next day to make up for a missed dose A good opportunity to discuss alcohol and interacting food/medicines Interactions and changes to diet will take around 5 days to change the result of a blood test Remember to complete a Yellow Card for any adverse effects reported for these relatively new medicines Nausea is not uncommon – avoided in Dabigitran by taking standing up with LARGE glass of water (irritant if it gets stuck) It is not important what time of day the medicine is taken, so long as it is the same time every day A forgotten dose of Rivaroxaban should be taken immediately it is remembered, but should not be doubled up on the same day to make up for a missed dose. A forgotten dose of Dabigatran can be taken any time up to 6 hours before the next scheduled dose. If remembered later than this, it should be omitted If asked about monitoring – GP should be monitoring renal function annually or more frequently if clinical concerns