Text File: Nursing Informatics and Healthcare Policy
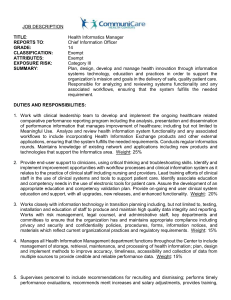
advertisement

Nursing Informatics and Healthcare Policy To practice effectively in today’s continually changing healthcare environment, informatics professional need to be aware of existing and proposed healthcare policy. Policy is defined as a course of action that guides present and future decisions. Both existing conditions and emerging trends in the healthcare industry influence policy decisions. NI professionals need to be more cognizant of events and the healthcare policies that will affect their practice. Healthcare Policy and Nursing Informatics as a Specialty In 1992, the American Nurses Association (ANA) recognized NI as a specialty. To be acknowledged as a specialty within nursing, informatics had to demonstrate a differentiated practice base, identify the existence of educational programs in the field, show support from nationally recognized organizations, and develop a research agenda. The term NI first appeared in the literature in the 1980s. In a classic article that describes its domain, NI was defined as the combination of nursing, information, and computer sciences to manage and process nursing data into information and knowledge for use in nursing practice. Most recently, NI is described more broadly as “…a specialty that integrates nursing science, computer science, and information science to manage and communicate data, information, and knowledge in nursing practice. NI facilitates the integration of data, information, and knowledge to support patients, nurses, and other providers in their decision-making in al roles and settings. This support is accomplished through the use of information structures, information processes, and IT” (ANA, 2001, p.17) Differentiated and Interdisciplinary Practice A description of NI as a differentiated practice is given in the scope of practice and standards document. Informatics nurses should assist with the development and implementation of technology tools for clinical practice, evaluation of the effectiveness of technological tools on nurses’ work, and help prepare nurses to use information technologies. NI practice differentiates itself from other areas of nursing practice but emphasizes its interaction with informatics disciplines such as mathematics, statistics, linguistics, engineering, computer science, and health informatics. In fact, NI has been described as one example of a specific domain of informatics that falls under a broader umbrella of health informatics. Other examples of domain-specific informatics practices are medical informatics, dental informatics, and consumer informatics. The NI community believes it is essential to practice within an interdisciplinary team. An example of the interdisciplinary work is the Vocabulary Summit held annually at Vanderbilt University since 1999. The summit brings together nursing and medical informatics vocabulary experts to explore how further language development in nursing can facilitate the integration of computerized languages among healthcare disciplines. NI supports national efforts, such as those outlined by the Pew Health Professions and Institute of Medicine (IOM) to increase interdisciplinary education. An example of interdisciplinary education is the collaborative effort between the medical informatics (MI) and NI programs at the University of Utah. MI and NI faculty share teaching responsibilities in courses, serve jointly in student committees, work together on projects and share administrative decisions through an executive committee. Preparation for Specialty Practice To become a specialty, it was necessary for NI to show that educational programs are available to prepare nurses to practice in the field. Between 1988 and 1992, the Division of Nursing (DN), Health and Human Services Administration (HHSA), funded two Master’s NI programs, University of Maryland and University of Utah and doctoral program in NI at the University of Maryland. In 1997, NI specialty program opened at Ney York University, and in 1998 a specialty program was implemented at Duquesne University at Pittsburgh. The certification examination currently available through the American Nurses Credentialing Center is for a generalist in NI. From November 1995 through December 2003, 551 nurses have been certified as generalists in NI. A final requirement for a specialty is representation by at least one organization. NI has the support of both nursing and multidisciplinary organizations. Within nursing, there is organizational support in the American Organization of Nurse Executives. Increasingly, multidisciplinary organizations encourage informatics nurses to become actively involved in their organizations to help solve informatics practice issues. Two examples are AMIA and the Health Information Management Systems Society; informatics nurses have served as president of both of these organization. Healthcare Policy Impact on Nursing Informatics Practice Nursing Shortage and Nursing Informatics Nursing has experienced a number of shortages in recent history. An older nursing workforce, a higher ratio of older associate degree graduates rather than their younger baccalaureate counterparts, the availability of more attractive career opportunities for women, decreased interest in nursing as a career, and difficult work environments make this shortage different from those previously experienced. (2000). It is predicted that the shortage will result in a large deficit of nurses. The Bureau of Labor Statistics (BLS) is predicting registered nurse positions will increase more than 600,000 between 2002 and 2012. To cover these new positions and replace retiring nurses 1.1 million more nurses are needed by 2012. Although these numbers differ it is clear that without intervention the healthcare industry is headed for a major crisis in the nursing workforce. It is obvious this shortage will negatively impact the outcomes of patient care. Schools and colleges of nursing have shortened program lengths and instituted accelerated programs for those who already hold a baccalaureate degree in an attempt to increase nursing workforce numbers. In 2002 the AAN Commission on Workforce launched a multiphase project to develop IT that will help support nurses in their day-to-day work, thereby reducing the demands of their jobs. In Phase I, interdisciplinary, creative thinkers were assembled to determine how technology could be used to facilitate nurses’ work. Technology solutions should improve existing care processes and outcomes, increase access through the use of portable and handheld devices, incorporate Internet capability to overcome distance barriers of care and improve access to knowledge acquisition. As Phase II of the AAN technology project, systems will be designed, implemented and tested to determine their effect on nurses’ work. The additional integration of clinical data repositories, multidiscipline documentation, and point of care devices would help nurses access and share information in their work environments and finally nurses are migrating to organizations that have installed cutting-edge technology, making IS a marketing tool for attracting nurses. The long list of recommendations for IT solutions designed to help nurses perform their work demonstrates how the public policy issue of the nursing shortage impacts NI. Patient Safety and Nursing Informatics In U.S. hospital admissions it was estimated that between 44,000 and 98,000 patients die each year from medical errors. Among other strategies the report recommended the implementation of computerized physician order entry (CPOE) systems requiring the prescriber to enter data directly into computer systems to reduce medication errors. This began a continuing discussion of IT and patient safety within healthcare. Surveys confirm that concern for patient safety is the biggest factor driving IT. 47% of chief information officers who participated in the HIMM’S leadership survey in February 2004 specified that increasing patient safety would be their main focus in upcoming years. California law 1875, passed in 2003, applies pressure to hospitals to install IT to help healthcare professionals reduce errors. The National Alliance for Health Information Technology (NAHIT) is partnership of diverse healthcare leaders who are working to influence the use of technology to improve patient safety, quality, and efficiency. Connecting for Health(CFH), another public-private collaborative, was established by the Markle Foundation with additional support from the Robert Wood Johnson Foundation. The Markle Foundation is a private philanthropy that works to enable technology to improve people’s lives. This group addresses barriers to developing an interconnected health information infrastructure and is concerned with reducing medical errors, improving the quality of care, lowering costs and empowering patients. CFH has obtained consensus on an initial set of data standards, developed case studies on security, and defined the electronic personal health record. Strategies to achieve their goal include policy development, research, supporting solutions and involving the public. National Informatics Initiatives and Nursing Informatics Executive Order for National Interoperable Information System Clinical information systems (CIS) were introduced in some form during the 1970s and informatics professionals have discussed the need for system improvement, integration, and wider dissemination since that time. National events have placed IS at the forefront of health policy. On April 27, 2004, President George W. Bush issued an executive order “Incentives for the Use of Position of the Health Information Technology Coordinator” that has the potential to impact every healthcare entity, provider, and NI professionals in the United States. Components of the order are (1) establish a national health information technology coordinator position; (2) work to develop a nationwide interoperable health IT infrastructure; and (3) develop, maintain and direct implementation of a strategic plan to guide implementation of interoperable health IT in both public and private sectors. Guidelines for the infrastructure are (1) appropriate information is available at the time and place needed for medical decisions, (2) health quality is improved and evidence-based medical care is delivered, (3) healthcare costs are reduced, (4) more information is available to promote greater competition, (5) health information is exchanged, and (6) identifiable health information is secure and protected. The executive order helped to thrust IT into the spotlight as an important political issue. In June 2004, bipartisan House members formed a congressional caucus to influence issues surrounding IT. The caucus is expected to support policies such as financial incentives to increase the acceptance of IT by healthcare providers. Various Washington leaders have proposed bills to support the purchase and implementation of IS. These modest bills will not be effective overall in supporting the purchase of IS but should raise questions about how money is needed to accomplish the mandate. Unlike past years, the President’s budget does include money for nationally integrated IS nut informatics professionals, including nurses, recognize the amount would only fund a few demonstration projects. Even though Secretary Thompson has said mandates will not be used, the National Coordinator for Health IT, Dr. David Brailer, has warned that government would not wait long for the private sector to create a technology infrastructure in healthcare. He continually reminds audiences that everyday the infrastructure does not exist, 5-10 people die because needed information is not available or is unreadable. The American Association of Retired Persons (AARP), 35 million members strong, supports mandatory electronic prescribing rules and federal efforts to increase adoption of CPOE. All informatics professionals will need to help healthcare workers accept IT and push for implementation of CPOE. Informatics nurses have worked for years of implementation teams and are well positioned to continue to help get the national infrastructure in place. It will definitely take a collection of strategies, financial incentives, improved IT, and collaboration between public and private healthcare entities to accomplish the President’s order. National Health Information Infrastructures National Health Information Infrastructure is a voluntary initiative involving 3-stage process over 10 years, is intended to improve the effectiveness, efficiency, and overall quality of health and healthcare in the United States. NHII calls for comprehensive knowledge-based networks that integrate clinical, public health, and personal health information to improve decision making by having information available to providers. Informatics nurses were invited to attend and offer input into the NHII plan. As representatives of the largest healthcare provider group, nurses who were experts in informatics needed to be among the stakeholders included in further delineation of the NHII. Health Insurance Portability and Accountability Act (HIPAA) HIPAA was passed in 1996 and is intended to improve public and private health programs by establishing standards to facilitate the efficient transmission of electronic health information. The law designates financial penalties for noncompliance with standards related to specific transactions. Also known as administrative simplification, HIPAA requires the DHHS to establish national standards for electronic healthcare transactions; for national identifiers for providers, health plans, and employers; and for the security and privacy of health data. The privacy rule of HIPAA was published in December 2000 and became effective in April 14, 2001 with a compliance date of April 14, 2003. In essence the regulation requires health plans, healthcare clearinghouses, and healthcare providers to protect and guard against the misuse of identifiable health information. For example, under HIPAA patients must be permitted to review and amend their medical records. Healthcare providers have expressed concern that accessing their records could cause patients increased anxiety. Ross and Lin (2003) have determined that there are benefits, such as enhanced doctor-patient communication, and only minimal access of patients to their records. According to reports misunderstanding of HIPAA can prevent the sharing of needed information by healthcare providers. Informatics nurses are responsible for understanding and helping to implement the HIPAA regulations. Informatics nurses are also in a position to research potential impact of regulations on patients and can impact regulations by offering comments during the public comment period after the rules are published. National Agenda for Nursing Informatics The DN, HRSA, is responsible for setting national policy to guide the preparation of the nursing workforce, including preparation in the area of NI. Although the DN has supported NI projects, the nursing workforce has continued to be deficient in informatics skills. As a result, in 1997 the DN convened the National Nursing Informatics Work Group (NNIWG) to make recommendations to the National Advisory Council for Nurse Education and Practice (NACNEP) for setting the nation’s nursing informatics agenda (NIA) for nursing education and practice. There are five assumptions considered by NACNEP to be a basis for all further discussion if NI initiatives: (1) learners are students, faculty and clinicians, (2) NI must be considered within an interdisciplinary context of partnerships and collaboration. (3) Efforts should target disadvantaged and underserved populations. (4) Initiatives should be responsive to other government funding priorities. (5) Collaboration among federal agencies and between federal and private entities is necessary. Five key directions for informatics in nursing education and practice were recommended to the Secretary, DHHS in the NACNEP report. The recommendations are as follows: (1) educate nursing students and practicing nurses in core informatics content. (2) Prepare nurses with specialized skills in informatics. (3) Enhance nursing practice and education through informatics projects. (4) prepare nursing faculty in informatics. (5) Increase collaborative efforts in NI. The 1998 legislation specifically named informatics as one of the seven priority areas for strengthening capacity and is consistent with the NIA’s first strategic direction include core informatics knowledge and skill in al undergraduate, graduate, and continuing education programs. Recognizing the need to identify core informatics skills and knowledge to be included in all educational programs. If core content is included in educational programs, the nursing workforce increasingly will be prepared to use information technologies that have been or are being installed in healthcare delivery environments. The second strategic direction for NI is to increase the number of nurses with specialized skills in informatics. One interesting model would be to develop collaborative educational programs that cut across traditional disciplinary lines. Schools of medicine, nursing, dentistry, and IS management could be full partners in these programs, collaborating to share financial burdens, decision-making, curriculum planning, teaching and evaluation. Collaborative programs could provide core informatics content to students from multiple disciplines and then allow students to apply knowledge within their individual professional domains. The third strategic direction for NI is to enhance nursing practice and education through informatics projects. There is a need to improve the informatics skill of the nursing workforce, particularly with nurses who have been out of school for a few years. Informatics nurses need to work with academic and healthcare delivery entities to develop programs that use telehealth technologies to improve nursing workforce skills. The fourth strategic direction for NI is to improve faculty skills in NI so that they in turn can promote the development of informatics competency in students. To add the need to develop informatics skills might be overwhelming to some faculty members. Existing technology could facilitate innovative ways to meet the informatics needs of both faculty and students. Teleconferencing could be used for faculty to “attend” informatics courses offered on other campuses to improve their skills. Collaborative arrangements might also allow informatics nurse experts on one campus to educate students in other campus, thereby decreasing the unmet demand for faculty prepared to teach NI. It would also decrease the stress placed on faculty members to increase their skills in so many important areas of healthcare all at once. The fifth and final strategic direction is to increase collaborative efforts in NI. Many healthcare policy makers advocate that collaborative efforts are key to using resources wisely. The NIA also advocates collaborative efforts between federal agencies and among public and private organizations to identify and fund needed informatics research and projects. In 1998, the National Library of Medicine , National Heart, Lung, and Blood Institute, and the health informatics community collaborated to identify ways that information technologies could be used to accomplish the goals of the National Heart Attack Alert Program. Telehealth and Nursing Informatics Telehealth services have been provided for about 50 years but telehealth remains an underutilized tool for nursing and NI. Telehealth is the use of electronic information and telecommunications technologies to support long distance clinical healthcare, patient and professional health-related education, public health and health administration. In spite of the advances in telehealth technologies, disjointed development, research, demand and investment have produced the small telehealth market. The market that has been developed in telehealth has been independent of a national strategy or effort. Unfortunately telehealth provides such specialized tools it falls outside of the influence of groups like American Medical Association and the Advanced Medical Technology Association. Both telehealth and information technologies face barriers of acceptance, reimbursement, and licensure. Efforts are being made to close the gap but until recently, documentation of telehealth events has frequently been independent of or isolated from IS. In a 1997 report to Congress, the three major issues of reimbursement, licensure, and security were implicated in preventing the widespread adoption and use of telehealth. Nineteen states have passed laws requiring physicians to obtain full and unrestricted licenses to deliver interstate telehealth services, seven states issue special purpose licenses for telehealth practice. In December 2003, the center for Telemedicine Law and the Office for the Advancement of Telehealth (OAT) in HRSA assembled telehealth experts and state licensing board members to discuss options for eliminating interstate licensure barriers that impact telehealth practice. On the other hand the National Council of State Boards of Nursing (NCSBN) has implemented a model of mutual recognition in which nurses obtain a state-based license that is nationally recognized and locally enforced. A nurse obtains one license in the state of residence and can practice in other states that agree to participate in the compact, a legal document that regulates business between two or more states, without obtaining additional licenses. As of July 2004, 17 states have passed and implemented the Nursing Compact. Lack of reimbursement has been identified as the key barrier to expanding telehealth practice. The sustainability of telehealth programs is dependent on third party reimbursement. Third party payers account for over 88% of all telehealth reimbursements. Seventy-two telehealth programs surveyed had billable services, more than half of these programs are receiving reimbursement from private payers. The Balanced Budget Act passed in 1997 mandated the first national reimbursement policy of telehealth services for Medicare recipients. Telehealth providers felt the regulations as implemented were not inclusive enpugh to meet health needs to rural areas and voiced their concerns to CMS (formerly the Health Care Finance Administration) and Congress and asked for changes in the reimbursement policies. The Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000 (BIPA) changed some of the reimbursement policies. For example, an eligible provider no longer has to present the patient in the originating site. This ruling facilitates the increased use of telehealth in areas where specialists are not located. Information nurses, while largely focused on IS, generally have failed to recognize the need to integrate telehealth technologies with existing IS. Since telehealth technologies have such a tremendous potential to increase underserved populations’ access to healthcare, it would be fantastic to see more nurse practitioners deliver their services using telehealth.