CT Fellow Manual - Anesthesiology Intranet
advertisement

DEPARTMENT OF ANESTHESIOLOGY
ADULT CARDIOTHORACIC
ANESTHESIOLOGY
Fellowship Program
PROGRAM HANDBOOK AND
POLICY MANUAL
2014-2015
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Table of Contents
Handbook & Policy Manual
Program Personnel and Contact Information
Program Manual Statement
General Information
Department of Anesthesiology Resident and Fellow Listing
Faculty Listing and Clinical/Research Interests
Program Curriculum
Evaluation and Promotion Policy
Program Evaluation Process
Disciplinary, Concern/Complaints, Grievance
GME Disciplinary Policy
Program Concern/Complaint Policy
GME Grievance Policy
Duty Hours Policy
GME Duty Hours Policy
Program Duty Hour Monitoring Process
Program Call Policy/Guidelines
Alertness Management and Fatigue Mitigation
Unusual Resident-Initiated Extensions - Additional Duty
Senior Resident and Fellow - Preparation to Enter Unsupervised Practice of Medicine
Eligibility and Selection Policy
GME Eligibility and Selection Policy
Leave Policy
GME Leave Policy
Program Leave Process
Moonlighting Policy
GME Moonlighting Policy
GME Additional Pay for Additional Work Policy
Physician Impairment and Health (Substance Abuse) Policy
Professionalism Policy
Quality Improvement and Patient Safety Guidelines
Research / Scholarly Activity Guideline
Supervision Policy
GME Supervision Policy
Program Supervision Policy
Progressive Authority & Responsibility
Guidelines for When Residents Must Communicate with the Attending
Clinical Responsibilities by PGY Levels for Supervision
Transitions of Care Guidelines – Hand-off Process
GME USMLE (and COMLEX) Examinations
ACGME Specific Program Requirements
Page 2 of 60
3
4
4
8
10
11
32
32
36
36
36
37
37
37
37
37
38
39
39
39
39
42
42
42
44
44
44
45
48
55
56
56
56
56
57
57
57
59
59
60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Program Personnel and Contact Information
Ferenc Puskas, MD, PhD.
Kathy Riggs
Fellowship Program Director
Residency/Fellowship
Coordinator
303-848-6716
303-724-1761
303-724-1765
303-724-1761
Kathy.riggs@ucdenver.edu
Ferenc.puskas@ucdenver.edu
Page 3 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Program Manual Statement
The University of Colorado Department of Anesthesiology complies with Accreditation Council
for Graduate Medical Education (ACGME) and CUSOM Graduate Medical Education (GME)
policies, procedures and processes which are available on the GME website and manual. In
addition, direct access is available by clicking hyperlinks throughout this Program Manual.
The program reviews all GME and program policies, procedures and processes at least
annually with residents/fellows.
General Information
A. EDUCATIONAL FUND
The department provides book and educational support as follows for Fellows:
o
Educational Travel and Book Support ($2000 for fellowship)
o
SCA Membership
Your book and travel funds are given to you by the Department of Anesthesiology. Even
though you are allocated money for travel and books, please understand that there are
guidelines that must be followed to use these funds. You are not required to use the allotted
money. Unused money is returned to the department’s general fund. These funds may not be
used for computers, lap tops, I-phones or hardware of any kind.
The deadline for using your book and travel fund is May 30th of your graduating year. Please
submit all receipts for books and travel prior to that date.
How to Order and Get Reimbursed for Books:
1. The preferred method: To order a book(s), send an email to your Program Coordinator
indicating which book(s) you want to order. She will order the book(s) for you. The cost of the
book is automatically subtracted from your educational fund.
2. If you would prefer to purchase books on your own, give your itemized receipt (not the credit
card statement) to your Program Coordinator and she will process the reimbursement.
How to Schedule and Get Reimbursed for Travel:
Conference Registration Fees:
Many conferences have online registration. To use this method, you need to register for the
course from the computers in the Anesthesiology Library (AO1 Building). The Program
Coordinator can pay the fee with a department credit card. If the conference does not have online
registration, complete the registration and give it to the Program Coordinator who will fax the
form along with payment.
Airline Tickets and Hotel:
You are encouraged to book airline tickets through the University of Colorado’s Travel and
Expense System.
Page 4 of 60
University of Colorado School of Medicine
Department of Anesthesiology
1. Log on to https://my.cu.edu . Your username
and password
Residency
Programis the same as your email’s login
information.
2. Click on “My Tools”
3. Click on “Open CU Travel and Expense System”
4. Complete your information under “Trip Search”
5. You will need to pay for your hotel first, but will be reimbursed after the trip.
6. Bring a copy of your conference brochure, all receipts, including travel itinerary, to your
Program Coordinator for reimbursement.
Mileage:
If you choose to drive to a conference that is out of state, you are either reimbursed the mileage
rate (.50/mile) or the cost of round trip airfare, whichever is lower. Driving to an out-of-state
conference is highly discouraged; you are using your own vehicle, your own insurance and if you
are in an accident, you will receive no compensation from the Department of Anesthesiology or
from the State of Colorado for injury or damages to person or vehicle.
How to Submit Receipts for Reimbursement:
1. You must submit original receipts. You must also provide a copy of the meeting flyer. You do
not need to save meal receipts. You will be paid a daily meal per diem, the amount of which
depends on the city you are visiting. You receive 75% of the total meal per diem on the first and
last day of travel and a full per diem for the days in between.
2. Your Program Coordinator will submit your expenses through the University of Colorado’s
online finance system. Once the reimbursement is submitted, you will receive an email from
AutoNotification@concursolutions.com asking you to log on to the system to certify and submit
the reimbursement. (Instructions below).
3. Your reimbursement is deposited directly into your checking account, usually within 3 days of
your approval.
How to Approve Reimbursements:
First you will receive an email from AutoNotification@concursolutions.com entitled “Report
Ready for Submission”
1. Log on to MyCU - Use the link in the email or open your browser to the my.CU portal
(my.cu.edu). Log in using the same credentials used to access your campus email. Select the
MY.TOOLS tab and click the Open CU Travel and Expense System.
2. Review the Expense Report – In the Active Work section, select the appropriate report. On the
Expense List page, review the transactions included in the report.
3. Certify and Submit Expense Report – Click the Submit Report button. A pink window will pop
up. Type an asterisk (Shift 8) in the box. Two names will appear in the box. Click on Kirstin Runa
or Roger Japp (Use Roger’s name first if available). Then click Submit Report.
4. Log out.
Page 5 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
B. COLORADO PHYSICIAN HEALTH PROGRAM (CPHP)
Office: 303-860-0122 Fax: 303-860-7426
The Colorado Physician Health Program (www.CPHP.org) is a not-for-profit organization,
independent of other medical organizations and the government. CPHP provides peer assistance
services at no cost for licensed physicians and physician assistants of Colorado. CPHP clients are
assured confidentiality as required by law or regulation. Peer assistance services aid individuals
who have difficulties or problems such as emotional, psychological or medical issues. CPHP assists
its clients with medical and/or psychiatric conditions (e.g. Alzheimer’s disease, HIV infection,
depression or substance abuse) as well as psychosocial conditions (e.g. family problems or stress
related to work or professional liability difficulties).
CPHP provides diagnostic evaluation, treatment referral as well as treatment monitoring and
support services. CPHP believes that early intervention and evaluation offer the best opportunity
for a successful outcome and preventing the health condition from needlessly interfering with
medical practice.
CPHP does not (with rare exceptions regarding safety) disclose the identity or information about
any current or former participant without a written release of information. CPHP maintains
records on participants by code number; thus appointment schedules, file folders, etc. are
recorded by number. This number is used in lieu of a client name to assure anonymity within the
program. Any identifying information is kept in locked files. Only CPHP staff are aware of the
individual identify of a participant. Staff members sign a formal confidentiality agreement that
specifies the confidentiality requirements and imposes consequences should a breach occur.
CPHP clients are not identified to the Board of Medical Examiners.
C. CONTROLLED SUBSTANCES POLICY AT UCH
The UCH Anesthesia Operating Room Pharmacy Controlled Substances Policy and Procedure is
included in the Policies section of this manual. In addition, The Impairment Physician Policy can
be found in the Graduate Medical Education Manual.
D. HEALTH, DENTAL, LIFE AND DISABILITY INSURANCE
Please refer to the 2013-2014 Graduate Medical Education Manual, for a summary of your
benefits.
E. E-MAIL ACCOUNTS
Fellows are provided a University e-mail address, which you are encouraged to use. Instructions
on how to access your e-mail is provided in your orientation packet.
F. MEAL TICKETS
See the 2013 Hospital Meal Policy.
Page 6 of 60
University of Colorado School of Medicine
Department of Anesthesiology
G. PAYROLL
Residency Program
Payday is the last working day of the month. Automatic deposit is mandatory. If you have not
completed an automatic deposit form, please do so as soon as possible to avoid delay of your July
paycheck.
H. CASE DOCUMENTATION
Fellows are required to document cases and procedures each month. At the end of each
academic year, an Annual Training Report (a record of your O.R. cases) is submitted to the
ABA.
I. MOONLIGHTING POLICY
The Department of Anesthesiology adheres to the Graduate Medical Education’s policy on
Moonlighting. Please review pages 68-71 of the GME Housestaff Manual.
J. GRIEVANCE PROCEDURES FOR HOUSESTAFF
Residents who wish to communicate complaints or resolve issues within the program or
department may bring them up at our monthly Resident/Chair Forum or meet with their Faculty
Advisor, the Residency Director or the Chairman at any time. In addition, Complaints, and
Grievance Procedures are described on pages 36 and 61 of the 2012-2013 of the Graduate
Medical Education Manual.
K. ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME)
The ACGME Program Requirements for Graduate Medical Education in Anesthesiology are listed
on their website. To access this document, log on to www.acgme.org; click on Review Committees;
click on Anesthesiology; Click on Program Requirements; then click on the PDF link for
Anesthesiology.
L. DEPARTMENT OF ANESTHESIOLOGY FACULTY AND RESIDENTS
A list of our program faculty and residents/fellows can be found on pages XXX. In addition, a
roster of departmental employees is listed on the Intranet (http://virtue.ucdenver.edu/) under
“Directory”.
M. EMERGENCY CONTACT INFORMATION
It is essential that we have current information on file for you in case of an emergency. Please
inform your Program Coordinator – {Kathy Riggs, 303-724-1765 or Kathy.riggs@ucdenver.edu}
of address or phone number changes and the person to contact in case of an emergency.
Page 7 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Anesthesiology Residents/Fellows
2013-2014
PGY 4
Grant Armour, MD – University of Colorado
Timothy Casias, MD – University of Colorado
David Dragoo, MD – University of Illinois
Samuel Gilliland, MD – University of Kansas, Kansas City
Neena Gupta, MD – Virginia Commonwealth University
Ross Hanson, MD – University of Rochester
Brian Johnson, DO – Western University of Health Sciences
Sarah Killeen, MD – University of South Alabama
Mike Kim, DO – Touro University
Emily McQuaid-Hanson, MD – University of Rochester
Neil Mehta, MD – University of Chicago
Carolyn Mohr, MD –East Carolina University
Benjamin Snyder, MD – University of Colorado
Mario Villasenor, MD – University of Texas – San Antonio
Matthew Wyatt, MD – University of Colorado
PGY 3
K. Slade Bigelow, DO- Rocky Vista University
Nathaniel Brown, MD- St. Louis University
Melvina Cheung, MD- Eastern Virginia Medical School
Terry Easton, MD- Indiana University
Zachary Hesse, MD- Hahnemann University
Luke Johnson, MD- University of Colorado
Tam Nguyen, MD- University of Colorado
Jason Papazian, MD- University of Colorado
Aaron Persinger, MD- University of Nebraska
Shaina Richardson, MD- University of Nevada
Justin Schulte, MD- Sanford
Jillian Vitter, MD- Georgetown University
Scott Vogel, DO- Oklahoma State University College of Osteopathic Medicine
Jennifer Wu, MD- Baylor
Erin Zurflu, MD- Georgetown University
PGY 2
Benjamin Abram, DO- Georgetown University
Alexander Behm, MD- Michigan State University
Steven Bourland, DO- Rocky Vista University
Laura Coats, MD- Indiana University
Kristina Coger, MD- University of Nevada
Meagan Gold, MD- University of Colorado
Lyndsey Graber, MD- University of Colorado
Chloe Hughes, MD- University of Colorado
Benjamin Lippert, DO- Touro University
Matthew Lyman, MD- Saint Louis University
Lauren McLaughlin, DO- Rocky Vista University
Benjamin Reynolds, MD- R Franklin University
Colby Simmons, DO- Kansas City University
Shannon Simon, MD- George Washington University
Leah Winters, MD- Wake Forest University
PGY 1
Ryan Cotter, MD- Mount Sinai
David Douin, MD- Tufts University
Page 8 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Brian Duggar, MD- Virginia
Commonwealth
University
Residency
Program
Antasia Giebler, DO- Arizona College of Osteopathic Medicine
Cardiothoracic Fellows
Natalie Hamilton, MD- University of Colorado
Kari Obma, MD- University of Wisconsin
Pain Medicine Fellow
Amanda Wallace
Page 9 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Program
Faculty Listing Residency
and Clinical/Research
Interests
Name
Cardiothoracic Anesthesiology Faculty
Area of Interest
Paul Chetham, M.D.
Cardiothoracic Anesthesia
Randall Clark, M.D.
Pediatric Cardiothoracic
Anesthesia
Cardiothoracic Anesthesia
Greg Deward, M.D.
Robert Friesen, M.D.
Sandra Fritz, M.D.
Pediatric Cardiothoracic
Anesthesia
Pediatric Cardiothoracic
Anesthesia
Cardiothoracic Anesthesia
Glenn Gravlee, M.D.
Cardiothoracic Anesthesia
Eric Helander, M.D.
Cardiothoracic Anesthesia
Peter M. Hession, M.D.
Cardiothoracic Anesthesia
George Justison, B.S.
Clinical ManagerPerfusion
Cardiothoracic Anesthesia
K. Peter Fritz, M.D.
Edwin Lee, M.D.
Glenn Merritt, M.D.
Fadi Nasrallah, M.D.
Pediatric Cardiothoracic
Anesthesia
Cardiothoracic Anesthesia
Luke Osborne, M.D.
Cardiothoracic Anesthesia
Ferenc Puskas, M.D.
Cardiothoracic Anesthesia
Ernesto Salcedo, M.D.
Echocardiography
Tamas Seres, M.D.
Cardiothoracic Anesthesia
Scott Stenquist, M.D.
Pediatric Cardiothoracic
Anesthesia
Cardiothoracic Anesthesia
SICU
Pediatric Cardiothoracic
Anesthesia
Cardiothoracic Anesthesia
Breandan Sullivan, M.D.
Mark Twite, MD
Nathaen Weitzel, M.D.
Program
Page 10 of 60
Hospital
Exempla St Joseph
Hospital
The Children’s Hospital
Exempla St. Joseph
Hospital
The Children's Hospital
The Children’s Hospital
Exempla St. Joseph
Hospital
University of Colorado
Hospital
Exempla St Joseph
Hospital
Exempla St. Joseph
Hospital
University of Colorado
Hospital
Exempla St. Joseph
Hospital
The Children’s Hospital
University of Colorado
Hospital
Exempla St. Joseph
Hospital
University of Colorado
Hospital
University of Colorado
Hospital
University of Colorado
Hospital
The Children's Hospital
University of Colorado
Hospital
The Children’s Hospital
University of Colorado
Hospital
University of Colorado School of Medicine
Department of Anesthesiology
Residency
Program
Curriculum
Didactic Program
Schedule
Didactic Conference Weekly Schedule
DAY/TIME
TOPIC
MONDAY
6:45-7:45 a.m.
Grand Rounds
4:00-5:00 pm
Research Seminar (once a month)
Tuesday
3:30-4:30 pm
Board Preparation Conference (1st week)
3:30-4:15 p.m.
Resident/Chair Forum (2nd week)
4:15-5:00 p.m.
Journal Club (2nd week)
3:30-4:30 pm
M&M/Clinical Case Conference (3rd and 4th week)
Wednesday
3:30-4:30 pm
CA1 Conference
THURSDAY
6:30-7:00 a.m.
In-Training Exam Lecture Series
FRIDAY
6:30-7:00 a.m.
Cardiac Lecture Series (Every Friday – attendance is mandatory
for Residents/Fellows rotating on the cardiothoracic service.)
Attendance at Grand Rounds, ITE Resident Lectures, Resident Chair/Journal Club
and Clinical Case Conferences is considered mandatory if you are rotating at
University of Colorado Hospital! If you are rotating at our satellite locations (DHMC,
VAMC), they are teleconferenced in the assigned conference room location(s). You
will be expected to sign in.
A.
CORE LECTURE SERIES
Page 11 of 60
University of Colorado School of Medicine
Department of Anesthesiology
During July and August a series of Core Residency
Lectures are offered
which are especially geared for new
Program
anesthesia residents; however they provide good refresher lectures for residents and fellows. A
sample weekly schedule can be found in this manual. Fellows also participate in Cardiac
Anesthesia Interdisciplinary Lectures. The calendar for these lectures is online at:
https://virtue.ucdenver.edu then click on Conference Calendar.
B.
CLINICAL CASE CONFERENCES
Clinical Case Conferences are discussions of patient cases involving interesting
management problems in anesthesiology. Often the cases presented involve morbidity or
mortality, so the conference is sometimes called “M&M.” These cases are contributed by
residents, CRNA’s and faculty based on perioperative, critical care, or pain management
experiences. These cases can be about unexpected (or expected) difficulties encountered
or just about interesting patient management problems. The goal is a free-wheeling
discussion between the moderator, presenters, and attendees that educates everyone.
Since these conferences also review events surrounding complications and deaths that
required peer review, trends and patterns discovered through the peer review process
will also be discussed. Discussions are aimed at developing strategies that will lead to
successful problem management. These conferences emphasize complete discussion of
alternate methods of care and the suitability of those methods for specific cases.
C.
ATTENDANCE AT CONFERENCES
Fellow attendance at conferences is expected. The Joint Commission on Accreditation of
Hospitals requires that attendance records by kept. A sign-in sheet is prepared for each
conference; it is the responsibility of the fellow to sign in. CME credit is granted for
attendance at Grand Rounds and the Clinical Case Conferences.
D.
CARDIOTHORACIC ANESTHESIOLOGY TOPICS
Topics to be covered by the Fellowship Program:
1. Embryological development of the cardiothoracic structures
2. Pathophysiology, pharmacology, and clinical management of patients with cardiac
disease, including cardiomyopathy, heart failure, cardiac tamponade, ischemic heart
disease, acquired and congenital valvular heart disease, congenital heart disease,
electrophysiologic disturbances and neoplastic and infectious cardiac diseases
3. Pathophysiology, pharmacology, and clinical management of patients with respiratory
disease, including pleural, bronchopulmonary, neoplastic, infectious and inflammatory
diseases
4. Pathophysiology, pharmacology, and clinical management of patients with thoracic
vascular, tracheal, esophageal, and mediastinal diseases, including infectious, neoplastic
and inflammatory processes
5. Non-invasive cardiovascular evaluation: electrocardiography, transthoracic
echocardiography, TEE, stress testing, cardiovascular imaging. (TEE education must be
based upon the training objectives for advanced perioperative echocardiography of the
American Society of Echocardiography and the Society of Cardiovascular
Anesthesiologists outlined in “Guidelines for Training in Perioperative
Echocardiography” [Appendix I]
6. Cardiac catheterization procedures and diagnostic interpretation: invasive cardiac
catheterization procedures, including angioplasty, stenting, and transcatheter laser and
mechanical ablations
Page 12 of 60
University of Colorado School of Medicine
Department of Anesthesiology
7. Non-invasive pulmonary evaluation:
pulmonary
function tests, blood gas and acid-base
Residency
Program
analysis, oximetry, capnography, pulmonary imaging
8. Preanesthetic evaluation and preparation of adult cardiothoracic patients;
9. Pharmacokinetics and pharmacodynamics of medications prescribed for medical
management of adult cardiothoracic patients
10. Perianesthetic monitoring; non-invasive and invasive (intraarterial, central venous,
pulmonary artery, mixed venous saturation, cardiac output)
11. Pharmacokinetics and pharmacodynamics of anesthetic medications prescribed for
cardiothoracic patients
12. Extracorporeal circulation, including myocardial preservation, effects of CPB on
pharmacokinetics and pharmacodynamics, cardiothoracic, respiratory, neurological,
metabolic, endocrine, hematological, renal, and thermoregulatory effects of CPB and
coagulation/anticoagulation before, during, and after CPB
13. Pharmacokinetics and pharmacodynamics of medications prescribed for management
of hemodynamic instability: inotropes, chronotropes, vasoconstrictors, vasodilators
14. Circulatory assist devices: intra-aortic balloon counterpulsation, left and right
ventricular assist devices, and biventricular assist devices
15. Pacemaker insertion and modes of action
16. Cardiac surgical procedures: minimally invasive myocardial revascularization, valve
repair and replacement, pericardial, neoplastic procedures, and heart and lung
transplantation
17. Thoracic aortic surgery: ascending, transverse, and descending aortic surgery with
circulatory arrest, CPB employing low flow and or retrograde perfusion
18. Esophageal surgery: varices, neoplastic, colon interposition, foreign body, stricture,
tracheoesophageal fistula;
19. Pulmonary surgery: thoracoscopic or open lung reduction, bronchopulmonary lavage,
one-lung ventilation, lobectomy, pneumonectomy and bronchoscopy: endoscopic,
fiberoptic, rigid, laser resection
20. Postanesthetic critical care of adult cardiothoracic surgical patients
21. Perioperative ventilator management: intraoperative anesthetic, and critical care unit
ventilators and techniques
22. Pain management of adult cardiothoracic surgical patients
23. Research methodology/statistical analysis
24. Quality assurance/improvement
25. Ethical and legal issues
26. Practice management
E.
INTRADEPARTMENTAL ACTIVITIES
Activity
Lectures
Conferences, Seminars TEE Workshop
Morbidity and Mortality Conferences
Journal Club
# Per Year
48
48
20
12
The cardiothoracic anesthesia fellow will arrange the monthly journal clubs. The fellow
will deliver at least one Grand Rounds presentation during the one year period. In the
second half of the fellowship year the fellow will prepare didactic lectures for residents.
Page 13 of 60
University of Colorado School of Medicine
Department of Anesthesiology
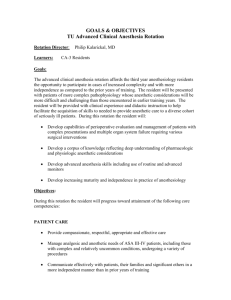
Program Goals and Objectives locatedResidency
at:
Program
http://virtue.ucdenver.edu/Resident/RotationGoals.htm
A.
DEFINITION
Cardiothoracic Anesthesia is the subspecialty of anesthesiology devoted to the
preoperative, intraoperative, and postoperative care of adult patients undergoing
cardiothoracic surgery and related invasive procedures. Clinical training will also include
exposure to echocardiography, cardiology lab-based as well as intraoperative echo
studies, with the goal of “Perioperative TEE Board Certification”.
B.
DURATION AND SCOPE OF EDUCATION
Subspecialty training in adult Cardiothoracic Anesthesia will be a minimum of twelve
month in duration, beginning after satisfactory completion of Accreditation Council for
Graduate Medical Education (ACGME) accredited residency program in anesthesiology.
Cardiothoracic Anesthesia education requires an intensive continuum of training
therefore it should not be interrupted by frequent or prolonged periods of absence.
The adult cardiac portion focuses on all elements of the perioperative care of patients for
all forms of cardiac surgery, including coronary revascularization, valve replacement,
valve repair, adult surgery for congenital abnormalities, and ventricular remodeling.
Fellows will gain experience with the placement and clinical use of ventricular assist
devices in addition to intra-aortic balloon pump (IABP) and extracorporeal membrane
oxygenation (ECMO) technology. The fellow is participating in the heart and lung
transplantation program at UCHSC and getting experience in perioperative management
of transplant patients. The scope of training includes participation in perioperative
management of patients undergoing major vascular surgery such as surgery involving the
aorta or great vessels.
During the elective Pediatric Cardiac Anesthesia rotation the fellow will be involved in
perioperative management of children with congenital heart diseases. In addition, the
rotation focuses on all elements of anesthesiology for thoracic surgery, including
bronchoscopy, mediastinoscopy, thoracotomy, lung resection, pneumonectomy, lung
volume reduction and lung transplantation.
The training will include anesthesia for non-operative diagnostic and interventional
cardiac and thoracic procedures outside the operating room. One month of the training
period is designated to participate in postoperative management of patients after
cardiothoracic surgery in the SICU.
The fellow is to act in a supervisory capacity to residents rotating through the cardiac
operating rooms, which also entails teaching responsibilities.
Participation in ongoing and/or fellow/advisor –designed clinical or basic studies is
encouraged also. Since transesophageal echocardiography has become incorporated as a
routine monitor used in all patients undergoing open heart procedures, it is expected that
all fellows will acquire advanced clinical proficiency and mastery in the use and
application of intraoperative TEE.
C.
GOALS AND OBJECTIVES
The fellowship in Cardiothoracic Anesthesia will be structured to ensure optimal patient
Page 14 of 60
University of Colorado School of Medicine
Department of Anesthesiology
care while providing fellows theResidency
opportunityProgram
to develop skills in clinical care and
judgment, teaching and research. The fellow will be proficient in providing anesthesia care
for patients with cardiac, vascular or thoracic diseases undergoing surgery with and
without extra corporeal circulation. The fellow will develop skills in the conduct of
preoperative patient evaluation and interpretation of cardiovascular and pulmonary
diagnostic test data, hemodynamic and respiratory monitoring, advanced level
perioperative TEE, and management of cardio pulmonary bypass. The fellow will
understand the principles and practice of pharmacological and mechanical hemodynamic
support, and perioperative critical care including ventilatory support and perioperative
pain management.
The specific objectives are listed below:
CARDIOTHORACIC ANESTHESIA - UNIVERSITY OF COLORADO HOSPITAL
Definition
The Cardiothoracic Anesthesiology Fellowship is a one-year learning tour in cardiothoracic
anesthesiology. The adult cardiac portion focuses on all elements of the perioperative care of
patients for all forms of cardiac surgery, including coronary revascularization, valve replacement,
valve repair, arrhythmia surgery, ventricular remodeling and heart transplantation. In addition,
the Fellowship focuses on all elements of anesthesiology for thoracic surgery, including
bronchoscopy, mediastinoscopy, thoracotomy, lung resection, pneumonectomy, lung volume
reduction, tracheoplasty and lung transplantation. The Fellowship focuses on major vascular
surgeries also including open and closed aortic surgeries in the OR or in interventional radiology
locations as well as pacemaker placement and management, arrhythmia management and
interventional cardiology cases in interventional cardiology or electrophysiology laboratory
locations. These cases are: percutaneous management of mitral valve diseases, percutaneous
closure of ASD and VSD, radiofrequency ablations and pacemaker placements and checkups. The
emphasis during the Fellowship year is to manage simple and complex cardiothoracic and major
vascular cases with increasing independence. The Fellow has his/her own cases and supervises
residents on cardiothoracic rotation.
Curriculum
The goal is to provide a broad exposure to all elements of anesthesia for adult cardiac surgery.
The clinical experience is supplemented by a detailed manual, a book, a weekly subspecialty
conference and a monthly journal club. In addition, the rotation provides clinical experiences with
all elements of thoracic anesthesiology, including preoperative assessment, consultation, line
placement, thoracic epidural analgesia, double lumen endotracheal tube placement and
confirmation of the position, fiberoptic bronchoscopy, and one lung ventilation.
The Fellow will do their own cases and supervise residents under supervision by an attending. As
distinguished from the CA-3 resident the emphasis during this year is to establish leadership role
in anesthesia management in simple and complex cases. After establishing a deep understanding
of the problems of cardiac anesthesia the Fellow will put the problems in the perspectives of
evidence based medicine. Besides handling the clinical challenges of cardiothoracic anesthesia the
Fellow will build up a wide range experience and knowledge in clinical practice of
transesophageal echocardiography (TEE). The Fellow will use TEE as a monitoring or diagnostic
tool based on the clinical situation.
Medical Knowledge
At the conclusion of this Fellowship program, the Fellow should demonstrate the following:
Page 15 of 60
University of Colorado School of Medicine
Department of Anesthesiology
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
Residency Program
Describe the anatomy and physiology of the normal heart in comparison with the
heart in different acquired and congenital heart diseases.
Discuss pharmacology pertinent to the cardiovascular system.
Explain the epidemiology and the trend of treatment of coronary artery disease.
Evaluate the indication and outcome of different kind of coronary artery surgeries
including pump and off-pump procedures.
Describe the epidemiology and pathophysiology of different valvular heart
diseases and evaluate the indications and outcomes of different surgical
modalities based on recent literature.
Explain the advantage and disadvantage of valve repair surgeries.
Describe the epidemiology, anatomy and pathophysiology of major congenital
heart diseases.
Describe the anesthetic management of patients with congenital heart diseases for
non-cardiac or cardiac surgery explaining the role of different transient cardiac
shunts.
Discuss and explain the rationale of induction and maintenance of anesthesia
techniques for cardiothoracic surgery.
Characterize the patient population waiting for cardiac transplantation.
Describe the anesthetic management for ventricular assist device placement and
heart transplantation.
Describe the anesthetic management for pulmonary embolectomy.
Describe the management of pulmonary hypertension.
Describe the management of right ventricular failure.
Describe the myocardial remodeling due to coronary artery disease.
Describe coronary anatomy and consequences of coronary occlusion.
Describe the hemodynamic changes and myocardial remodeling due to valvular
heart diseases.
Discuss the possible complications and their treatment during cardiopulmonary
bypass.
Describe the indications and therapeutic role of intra-aortic balloon pump (IABP)
treatment.
Describe the role of ECMO in catastrophic adult cardiac cases.
Describe the pathophysiology and possible complications of aortic surgery.
Describe the anesthesia management of circulatory arrest.
Describe the indications and role of left ventricular partial bypass.
Describe the pharmacology of different inotropic and vasoactive agents and their
role in complex heart cases.
Describe the role of Nitric Oxide in anesthetic management of complex cardiac
cases.
Describe common problems and their treatment during postoperative recovery of
the complicated cardiac surgery patient.
Describe the changes of the coagulation system during cardiopulmonary bypass.
Describe the TEG and other coagulation laboratory parameters used for evaluate
the coagulation system during cardiac surgery. Establish treatment plan based on
the changes of coagulation parameters.
Describe the role of Factor VIIa in treatment of catastrophic bleeding.
Describe the management of ventilation of the complicated cardiac/thoracic
surgery patient.
Describe preoperative assessment for thoracic surgery.
Use preoperative respiratory parameters to expect complications during
anesthetic management of thoracic cases.
Describe risks of prolonged intubation.
Page 16 of 60
34.
35.
36.
37.
38.
39.
40.
University of Colorado School of Medicine
Department of Anesthesiology
Describe the causes andResidency
treatment of Program
failing one-lung ventilation.
Describe possible complications after major lung resection and pneumonectomy.
Describe the patient population waiting for lung transplantation. Evaluate the
outcome of single or double lung transplant.
Describe the anesthetic management of lung transplantation.
Describe different techniques for analgesia during and after thoracic surgery.
Describe the expected postoperative recovery of the complicated thoracic surgery
patient.
Use advanced TEE techniques to evaluate and monitor the patient and seek for
pathology which might change the surgical and anesthetic management.
Patient Care
At the conclusion of the Fellowship program, the Fellow should be able to:
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
Insert, manage, and interpret the results of arterial catheterization, central venous
catheterization and pulmonary artery catheterization.
Prepare the patient for cardiopulmonary bypass, while considering possible
complications.
Manage complex cases with or without cardiopulmonary bypass.
Prepare the patient for coming off cardiopulmonary bypass while considering
possible difficulties.
Manage the process of coming off cardiopulmonary bypass.
Prepare the patient for transport to the SICU after cardiac surgery in a safe and
timely manner.
Transport the patient into the SICU safely.
Give detailed report in SICU with continuous vigilance about the patient’s
hemodynamic status.
Perform fiberoptic bronchoscopy for double lumen tube placement.
Insert and manage double lumen endotracheal tubes with independence.
Place and manage epidural catheters for patients having cardiothoracic surgery.
Identify high risk patients and establish effective plan to treat the problems.
Conduct one-lung ventilation; solve hypoxic conditions considering the indications
for cardiopulmonary bypass.
Transfer thoracic patients to the PACU and ICU.
Recognize acute respiratory failure and establish appropriate treatment.
Safely reintubate patients after thoracotomy when indicated.
Recognize massive intrathoracic bleeding and initiate immediate treatment.
Initiate appropriate analgesia after thoracic surgery.
Communication and Interpersonal Skills
At the conclusion of the Fellowship program, the Fellow should be able to:
1.
2.
3.
4.
5.
Identify the relevant preoperative information needed to plan anesthesia for
cardiac surgery.
Supervise residents and coordinate the cardiac anesthesia and surgery team to
prepare the patient for cardiac surgery.
Expect possible complications during cardiac anesthesia management based on
clinical and laboratory data and establish appropriate treatment plan.
Identify complications during the cardiac surgical procedure quickly by
observation and interaction with the surgical team.
Supervise residents and coordinate the cardiac anesthesia and surgery team to
manage the patient during cardiac surgery.
Page 17 of 60
6.
7.
8.
9.
University of Colorado School of Medicine
Department of Anesthesiology
Identify the relevant preoperative
information
Residency
Programneeded to plan anesthesia for
thoracic surgery.
Expect possible complications during the thoracic surgical procedure based on
clinical and laboratory data and establish appropriate treatment plan.
Identify complications during the thoracic surgical procedure quickly by
observation and interaction with the surgical team.
Supervise residents and coordinate the cardiac anesthesia and surgery team to
manage the patient during thoracic surgery.
Professionalism
At the conclusion of the Fellowship program, the Fellow will be able to:
1.
2.
3.
4.
5.
6.
7.
Prepare the patient for the cardiothoracic procedures and invasive monitoring.
Prepare the patient for possible complications.
Properly perform consultative and preoperative assessments for complex cardiac
and thoracic cases.
Effectively work as a team leader to solve complications and difficulties during the
anesthetic management.
Effectively communicate with the surgical team in critical situations.
Effectively communicate with the pain team to set up appropriate plan for pain
management during and after surgery.
Supervise and teach residents along with other students during the cardiothoracic
procedures.
Systems based practice
1. Understand billing and collections for cardiac and thoracic procedures including
modifiers for these procedures.
2. Complete the appropriate paperwork and computer work for preoperative,
intraoperative, and postoperative documentation.
3. Understand billing and collections for transesophageal echocardiography
4. Recognize strengths and limitations of current patient care systems supporting
cardiothoracic surgery patients and make constructive suggestions for improvement
in these systems as needed.
PEDIATRIC CARDIAC ANESTHESIA-THE CHILDREN’S HOSPITAL
CONGENITAL HEART DISEASE CT ANESTHESIOLOGY ROTATION
Fellows will rotate with congenital heart anesthesiology for a minimum of seven weeks during
their yearlong Fellowship. The experience will include cases utilizing cardiopulmonary bypass,
cardiac cases off-pump, thoracic operations and cases in the cardiac catheterization laboratory.
Page 18 of 60
University of Colorado School of Medicine
Department of Anesthesiology
The Fellows will also participate in anesthesia
cases Program
of non-cardiac surgery in children with
Residency
congenital heart disease while on the cardiac rotation and as appropriate during their general
rotations. The rotation is divided into weekly blocks to permit adequate time and rest to absorb
the educational information without being overwhelmed by the intensity of a prolonged serviceexperience.
Medical Knowledge
Anatomy & Physiology
Cardiovascular physiology of common forms of CHD:
o Mixing Lesions: VSD, ASD, PDA, AV canal
o Obstructive Lesions (two ventricle physiology): CoA, AS, PS, ToF
o Single Ventricle: HLHS, Tric Atr,Heterotaxy syndrome/Unbalanced AV canal
o Stages of single ventricle palliation and physiological implications
Respiratory physiology
Pulmonary Hypertension
Transition from fetal circulation
Pharmacology of vasoactive medications and prostaglandin / prostacyclins
Preoperative preparation
Parental preoperative anxiety
Informed consent issues ethical and legal aspects, including Jehovah's Witnesses.
Preoperative laboratory testing in children
Preoperative cardiac evaluation including interpretation of echocardiographic results
Premedication techniques
Pediatric history and physical techniques 1
Induction and Maintenance of General Anesthesia
Induction techniques and medications
Maintenance techniques adapted for physiological needs and neurological considerations
Cardiopulmonary Bypass
Neurological implications of pH management, bypass flow rates and temperature
Management of hematocrit and electrolytes
Coagulation and coagulopathies
Pediatric Equipment and Monitoring
Arterial catheterization and central venous monitoring
Transport of critically ill children
Application and interpretation of NIRS and its limitations
Cardiac catheterization Laboratory and Bedside Cardiac Anesthesiology
Atrial Septostomy
Hemodynamic catheterization and vascular intervention including stenting
Electrophysiology studies
Post Heart transplant surveillance
Closure of ASD with transcatheter device
Closure of PDA
Closure of aortopulmonary collaterals
Page 19 of 60
Cardiac MRI
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Techniques for anesthesia
Interpretation of results for preoperative anesthetic and operative planning
Regional Anesthesia for Thoracic Procedures
Local anesthetics
Thoracic epidural techniques
Caudal techniques
Postoperative pain management
Pediatric Co-existing Diseases
VATER/VACTERL
Goldenhar syndrome
Down’s Syndrome
William’s Syndrome
Heterotaxy Syndrome
Achondroplasia
Ellis Van-Creveld
Patient Care Skills (including technical skills to be learned and demonstrated)
The Fellow will be expected to become competent in:
1. Performing preanesthetic assessment and preparation of the pediatric cardiac patient
2. Appreciating pediatric and developmental pharmacology in light of the patient’s
physiology
3. Interpretation of pediatric laboratory results
4. Maintaining intraoperative temperature regulation
5. Providing appropriate perioperative fluid and transfusion therapy
6. Recognition and therapy for common coagulation abnormalities in this population
7. Assessing postoperative pain therapy
8. Recognizing and managing common transport and ICU handoff problems
9. Detailing methods and goals of mechanical ventilatory support
10. Pharmacological support of circulation
11. Considerations for anesthesia management during diagnostic/therapeutic procedures
outside the operating room complex
12. Recognition and treatment of perioperative vital organ dysfunction
13. Understanding of the psychological impact of serious medical conditions and surgery on
pediatric patients and their families
Interpersonal and Communication Skills
1. Perform thorough and compassionate pre-operative evaluations
2. Access current literature to delineate specific concerns regarding the perioperative care of
all scheduled complex patients
3. Communicate anesthesia plan and concerns with attending staff, surgeons and nurses
4. Provide rapport with parents caretakers, Children and surgeons
5. Actively participate in conferences
6. Interface with the patient’s family
Page 20 of 60
University of Colorado School of Medicine
Department of Anesthesiology
7. Follow their patients post-operatively
and discuss
any concerns with faculty
Residency
Program
Professionalism
1.
2.
3.
4.
Function effectively in the operating room environment as part of a team
Effectively transfer patients to the CICU and Cardiac Pre/Post Unit
Communicate post-operative plans to the CICU/CPPU nurses
Discuss Post-operative pain management strategies with CICU Staff, and pain
management team as appropriate
5. Provide Pre-operative consultative services
6. Regularly attend and participate in Surgical and catheterization lab conferences,
7. Fellows will at all times show compassion and respect for families and patients in their
care; Sensitivity to gender, culture, disabilities, and age specific anxiety is expected.
Effective, timely, and cordial interactions with the other care team providers are integral
to success.
Systems-Based Practice
1. Case discussion, and conferences allow the Fellow to learn about different types of
practices
2. Fellows complete a billing sheet on all cases and have access to Billing Codes fro all cases.
3. Pharmacy Medication Trays have cost of all medication listed, so that Fellows can take
that into consideration when choosing agents to use.
4. Heart Institute M&M conferences focus on systems based problems and solutions
5. Fellows will learn of the SPA and the Congenital Cardiac Anesthesiology Society’s roles
and resources in the field of CHD anesthesiology.
Practice-Based Learning and Improvement
1. Monthly Journal Club-prepared by Fellows with faculty mentoring. The purpose is to teach
Fellows critical appraisal of the literature as well as utilization of available medical
databases, evidence based medical resources and medical informatics to assist decision
making
2. Monthly research conference
3. Problem Based Learning Discussion-prepared by a Fellow with faculty mentoring to
discuss the management of a patient with an anesthetic or medical dilemma. Systems,
practice issues are included as part of the discussion
4. Grand Rounds-Fellows give 2/year on a topic of their choice, a Medline search, list of
references, slides and handouts are expected.
5. Monthly M&M conferences-frequently focus on systems based and problems based issues
and solutions.
Page 21 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
ECHOCARDIOGRAPHY ROTATION – UNIVERSITY OF COLORADO HOSPITAL
Medical Knowledge
At the conclusion of this Fellowship program, the Fellow should demonstrate the following:
A. Basic principles.
1. M-Mode, 2-D, Doppler
B. M-mode/single crystal:
1. Basic positions/views.
2. Normal anatomy.
3. Current diagnostic application/uses:
a. LV Chamber size and function
i. systolic
ii. diastolic
iii. regional wall abnormalities
iv. LV thickness
v. LV volumes, estimated vs. Simpson calculations
b. Valvular Heart Disease
Page 22 of 60
University of Colorado School of Medicine
Department of Anesthesiology
c. Pericardial effusion and
Tamponade
Residency
Program
C. Sector scan.
1. How different from M-mode; how technically obtain sector views.
2. Normal anatomy and views:
a. Parasternal long axis.
b. Parasternal short axis.
c. Apical 4 chambers, 2 chamber and long axis.
d. Subcostal.
e. Suprasternal.
3. Normal measurements and values.
4. Valvular abnormalities, including all 4 cardiac valves:
a. Stenosis.
b. Insufficiency.
5. Myocardial disease:
a. Differentiate global (dilated CM) vs. focal wall motion abnormalities (CAD).
b. Utilization of wall motion score.
c. Differentiate different segments of involvement in relationship to specific
coronary artery.
d. Importance of quality images to see endocardium.
e. Calculate ejection fraction:
i. Simpson: computerized (how derived).
ii. Visually estimating ejection fraction.
f. Hypertrophic cardiomyopathy:
i. ASH (asymmetric septal hypertrophic) vs. hypertrophic in other areas
(apical).
ii. Differentiate obstructive (SAM) vs. nonobstructive forms.
g. Restrictive CM:
i. “Sparkling” of myocardium and differential diagnosis.
ii. Amyloidosis: value of Doppler.
iii. Obliterative/Endocardial fibroelastosis.
6. Pericardial disease:
a. Effusion:
i. Size estimation.
ii. Hints to cardiac tamponade (RA collapse, RV collapse, IVC dilation and
non-changing size).
b. Constriction: importance of Doppler information.
7. Cardiac masses:
a. Tumors.
b. Vegetations.
c. Clot; mural; transient pulmonary emboli in right heart chambers.
d. Pseudo-tumors:
i. Eustachian valve.
ii. Chiari network.
e. Masses attached to pericardium.
8. Adult congenital heart disease: See individual lesions.
a. Structural abnormalities require knowledge of congenital heart disease
pathology.
b. Doppler flow with emphasis on color flow Doppler abnormalities to detect leftright shunts.
D. Doppler.
1. Differentiate pulsed wave (PW), continuous wave (CW), and color
flow Doppler (CFD), and how they are obtained.
Page 23 of 60
University of Colorado School of Medicine
Department of Anesthesiology
2. How to measure valvular gradients:
peak velocity,
mean velocity, pressure half time and
Residency
Program
valve area calculation.
3. How to estimate valvular regurgitation:
a. Regurgitant jet area.
b. Appropriate chamber dilatation.
c. Width of regurgitant jet.
d. PISA.
4. Estimate pulmonary artery pressure: tricuspid regurgitant jet derivation.
5. Recognize left-right shunts:
a. PDA: Parasternal short axis view.
b. ASD: Subcostal view best.
c. VSD: Parasternal short axis and apical 4 chamber views best.
6. Diastolic LV function:
a. E velocity.
b. A velocity.
c. E/A ratio.
d. IVRT (isovolumic relaxation time).
e. Deceleration time (DT) on anterior mitral leaflet and tricuspid valve.
f. Typical pattern of noncompliant left ventricle vs. restrictive pattern.
g. Differentiate restrictive cardiomyopathy vs. constrictive pericarditis.
h. Pulmonary vein identification and value, especially in mitral regurgitation.
i. Hepatic vein/IVC identification.
j. Tissue Doppler
E. Harmonic imaging.
F. Contrast imaging.
1. Viability
2. Endocardium visualization.
G. Transesophageal echo (TEE).
1. Compare single plane, biplane, multiplane techniques.
2. Technique:
a. Patient selection.
b. Sedation/anesthesia.
c. Antibiotic prophylaxis
d. Probe insertion.
e. Imaging planes: correlate with anatomy:
i. Base.
ii. Mid-esophageal.
iii. Transgastric.
iv. Aorta.
3. American Society of Echocardiography (ASE) criteria for appropriates experience and
training.
4. Specific diagnostic usefulness:
a. Cardiac masses.
b. Source of systemic embolus:
i. Tumor-atypical location.
ii. LA clot.
iii. Spontaneous contrast.
iv. Vegetations.
v. Atrial septal aneurysm.
vi. PFO with contrast injection.
vii. Aortic plaque.
c. Endocarditis:
i. Value/sensitivity vs. TTE.
Page 24 of 60
University of Colorado School of Medicine
Department of Anesthesiology
ii. Complications:Residency
abscess, ruptured
chordae.
Program
d. Aortic dissection.
e. Intraoperative monitoring, such as with mitral regurgitation severity post
repair.
f. Differentiate forms of left ventricular outflow tract obstruction.
g. Congenital disease.
h. Unable to visualize cardiac structure with transthoracic echo.
5. Contraindications for use.
6. Complications.
Patient Care
At the conclusion of the Fellowship program, the Fellow should be able to:
1. Develop specialized expertise in the performance and interpretation of perioperative
transthoracic and transesophageal echocardiography with the specific goal of attaining the
American Board of Echocardiography's Certification in Perioperative TEE at completion of
Fellowship training
2. Communicate effectively and demonstrate caring and respectful behaviors when
interacting with patient and their families.
3. Gather essential and accurate information about their patients.
4. Make informed decisions about diagnostic and therapeutic interventions based on patient
information and preferences, up-to-date scientific evidence, and clinical judgment.
5. Develop and carry out patient management plans.
6. Counsel and educate patients and their families.
7. Use information technology to support patient care decisions and patient education.
8. Work with health care professionals, including those from other disciplines, to provide
patient-focused care.
Communication and Interpersonal Skills
At the conclusion of the Fellowship program, the Fellow should be able to:
1. Create and sustain a therapeutic and ethically sound relationship with patient
2. Use effective listening skills and elicit and provide information using effective nonverbal,
explanatory, questioning, and writing skills.
3. Work effectively with others as a member or leader of a perioperative, cardiothoracic,
postoperative and critical care team or other professional group.
Professionalism
At the conclusion of the Fellowship program, the Fellow will be able to:
1. Analyze practice experience and perform practice-based improvement activities using a
systematic methodology.
2. Locate, appraise, and assimilate evidence from scientific studies related to their patients’
echocardiographic findings.
3. Apply knowledge of study designs and statistical methods to the appraisal of clinical studies
and other information on diagnostic and therapeutic effectiveness.
4. Use information technology to manage information, access on-line medical information; and
support their own education.
5. Facilitate the learning of residents, medical students and other health care professionals.
Systems based practice
1. Know how types of medical practices and delivery systems differ from one another, including
methods of controlling health care costs and allocating resources.
Page 25 of 60
University of Colorado School of Medicine
Department of Anesthesiology
2. Practice cost effective health care and
resource allocation
Residency
Programthat do not compromise quality of
care.
3. Advocate for quality patient care and assist patients in dealing with system complexities.
4. Partner with health care managers and providers to assess, coordinate, and improve health
care and know how these activities can affect system performance.
CRITICAL CARE ROTATION – UNIVERSITY OF COLORADO HOSPITAL
Medical Knowledge
The Fellow will be expected by the completion of the rotation to have an understanding of the
following and how these topics apply to the patient admitted to the critical care unit:
1.
2.
3.
4.
5.
6.
7.
8.
cardiovascular system anatomy and physiology
coronary vascular anatomy
physiology of coronary blood flow
regulation of cardiac output and low cardiac output states
diseases of cardiovascular system and pathophysiology of the disease states
learning the principles of heart failure and treatment options including transplantation
explaining indications, contraindications, risks, benefits procedural based techniques
developing technical knowledge with:
a.
pulmonary artery catheter placement and its usefulness in ICU
b.
modes of ventilation
c.
thoracentesis
d.
developing behavioral patterns allowing optimal decision-making abilities
Page 26 of 60
e.
f.
g.
h.
i.
University of Colorado School of Medicine
Department of Anesthesiology
displaying emotional
stability,Program
flexibility
Residency
utilizing strong cognitive processes
exhibiting strong communicative skills
decision making abilities with implementation abilities
patient advocacy approach
Patient Care
The Fellow will learn principles of intensive care in regards to the preoperative, intraoperative,
and postoperative care of cardiothoracic patients. In particular, they are expected to understand
the following:
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
coronary artery disease states, treatment options, benefits of intra arterial balloon pump
mitral valve disorders
aortic valve disorders
management of anti-coagulation
cardiopulmonary bypass and its effects on post operative period
infective endocarditis and management
care of patients for heart and lung transplantation
management of thoracic aneurysms
management of patient on mechanical ventilation and applying different modes of
ventilation and learning how to apply different modes to selective groups of patients
principles of ethics in intensive care
interaction with Chaplin and learning how to discuss patient care related issues with
family members
to learn as a member of multidisciplinary team and how to integrate the other team
members in coordinating care in ICU
advanced interpretations of monitoring data
procedures requiring drainage of pleural effusions
placement of renal replacement therapy catheters
cardioversion
advanced cardiopulmonary resuscitation
advanced diagnosis and management of cardiac arrhythmias
initiation of nutrition both enteral and parenteral when indicated
Communication and Interpersonal Skills
At the conclusion of this Fellowship program, the Fellow should demonstrate the following:
1. the necessity of effective communication in the ICU setting especially in regards to team
communication, e.g., nursing staff, consultants and surgical attendings
2. techniques to improve effective communication with patients, peers and health care team
for the patient’s interest
The Fellow will be responsible for:
1. communicating risks benefits to patient and family
2. patient thus understands what they will experience and its significance
3. inspire confidence in patient for staff
4. effective communication skills to health care team
5. listening to what others have to say
6. attitudinal and behavioral ways that support open and unimpeded communication
Professionalism
Page 27 of 60
University of Colorado School of Medicine
Department of Anesthesiology
At the conclusion of this Fellowship program,
the Fellow
should demonstrate the following:
Residency
Program
1.
2.
3.
4.
5.
6.
7.
8.
9.
learn definitions, concepts and give examples of medical professionalism
understand what professional ethics is
what defines strong personal character
act in ways that show commitment to medical professionalism
wear professional attire where appropriate
follow hospital, departmental protocol
establish professional relationships
strive for self improvement
behave with professional ethics and honesty
Practice-based learning and improvement
At the conclusion of this Fellowship program, the Fellow should demonstrate the following:
1. clinical experience
2. reflective practice
3. individual strengths and weaknesses in how one learns
4. the role of criticism for self improvement
5. the value of evidence based medicine as it applies to cardiovascular intensive care
6. critical thinking and integration of sound scientific literature
7. self awareness of abilities and limitations
8. reflective practice and skill for continued learning
9. enthusiasm
10. commitment for learning and acquiring, maintaining knowledge
Systems based practice
At the conclusion of this Fellowship program, the Fellow should demonstrate the following:
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
how the health care team interacts for the patient’s benefit
how the health care team approaches patient care in regards to the following:
patient presentation of cardiovascular disease
works to investigate patient illness and optimize care
system optimization of patient
system risk to patient
management of health care team
coordination of cardiothoracic surgery and anesthesia
safe patient transport
cost effective care
coordinate with CT Surgery and nursing staff
participate in quality improvement programs
function as a team member
initiate and provide appropriate consultation
show awareness and appreciation of their effect on patient care
Page 28 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
PERFUSION ROTATION – UNIVERSITY OF COLORADO HOSPITAL
Medical Knowledge:
At the conclusion of the Fellowship program, the Fellow will be able to:
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
Describe the characteristics of the components of a perfusion circuit
Describe all of the safety devices for the perfusion circuit
Discuss how all of the above fit together for a safe and controllable system
Identify the different types of pumps used during CPB and explain their function
Discuss safety concerns and methods of servoregulating each type of pump
Describe the different types of filtering technology used during CPB
Discuss the characteristics of individual filter types used during CPB
Describe the characteristics of an ideal oxygenator
Discuss the historical development of oxygenator techniques
Describe different types of membrane oxygenators
Discuss the oxygen characteristics of different membrane oxygenators
Describe the design characteristics of heat exchangers
Discuss the placement of heat exchangers in the CPB circuit
Describe the difference between a reservoir and a cardiotomy
Describe different reservoir technologies and configurations
Describe internal filtering systems found in cardiotomy systems
Discuss safety issues as they relate to reservoir.
Describe the different types of ultrafiltrators
Describe the operational characteristics of ultrafilters
Discuss the impact of hemoconcentration of circulating concentrations of drugs and ions
Describe and discuss the actions necessary prior to surgery
Describe a method of initiating CPB
Describe the parameters monitored during maintenance of CPB
Describe a method for weaning from CPB
Describe the use of the hemoconcentration before, during and after CPB.
Describe cannulation as it relates to the CPB patient
Describe the methods of physiologic monitoring for the CPB patient.
Identify the important monitoring variables that would assure that CPB delivery of
nutrients meets the tissue demands
Define homeostasis and physiological mechanisms that assure adequate uptake and
removal of metabolic products
Describe the physiological variables used to assess cellular energy balance during CPB
Describe the physiology of myocardial preservation
Discuss the determinants of appropriate myocardial preservation techniques
Discuss the technical details related to cardioplegia administration
Describe the desired characteristics of cardioplegia solutions
Discuss the role of each component used to achieve this ideal solution
Recognize optional pharmacological agents and explain their purpose
Describe the physiology of systemic hypothermia
Discuss application of systemic hypothermia to specific surgical procedures
Page 29 of 60
University of Colorado School of Medicine
Department of Anesthesiology
39. Understand and apply the requirements
of the
Standards for Perioperative Autologous
Residency
Program
Blood Collection and Administration
40. Describe the effects of hemodilution on the rheology of blood
41. Discuss how hemodilution changes the oxygen content and colloid osmotic pressure
42. Apply the formulas to calculate the hematocrit and colloid osmotic pressure after
hemodilution
43. Describe the indications for cell washing
44. Describe the contraindications for autotransfusion
45. Describe the general operation of the appropriate cell saving device
46. Discuss proper procedure for storage reinfusion and discard of end product
47. Discuss record keeping preventive maintenance and quality control
48. Describe the different types of ultrafiltrators
49. Describe the operational characteristics of ultrafilters
50. Discuss the impact of hemoconcentration of circulating concentrations of drugs and ions
51. Describe the use of the hemoconcentration during CPB to control hematocrit
52. Describe the actions of the various drugs available to reduce the amount of blood loss
during and after cardiac surgery
53. Describe the indications and contraindications for each of the drugs
54. Discuss dosing and CPB considerations for each drug.
55. Describe the perfusion techniques unique to the pregnant patient
56. Describe the physiological and anticoagulation needs of this patient
57. List the most frequent open-heart procedures for the pregnant patient
58. List and discuss the inherited and acquired blood disorders that are important to CPB
59. Describe the therapeutic approaches to each to be able to perform CPB
60. Discuss the potential for a catastrophe
61. Describe the proper responses and actions to a catastrophe
62. Discuss the rationale for using assisted venous return
63. Describe the indications for selective cerebral perfusion
64. Discuss the perfusion circuit; temperatures; pressures; and flows used with selective
cerebral perfusion
65. Discuss the outcomes of the technique compared to only profound hypothermic
circulatory arrest
66. Discuss the relationship of ECG blood pressure, blood gas, chemistry, and
67. temperature as they relate to patient status
68. Describe the indications for ECMO
69. Discuss the advantages of each cannulation technique
70. Discuss management of the ECMO patient – especially flows and anticoagulation
71. Describe how to terminate ECMO
72. List the indications and contraindications for the IABP
73. Identify the equipment required for the procedure
74. Describe the purpose for IABP
75. Discuss proper timing
76. Discuss the indications and contraindications for VAD implantation
77. Compare and contrast the different VAD systems and indications for use
78. Describe the cannulation techniques or VADS
79. Describe the long-term management requirements for each VAD system
Patient Care
At the conclusion of the Fellowship rotation, the Fellow will be able to:
Understand the basics of extracorporeal circulation, IABP and ventricular assist device function as
it relates to the safe conduct of anesthesia and postoperative care in the cardiothoracic patients
Page 30 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Communication and Interpersonal Skills
Residency Program
At the conclusion of the Fellowship rotation, the Fellow will be able to:
Communicate effectively with the cardiac Perfusionist, Cardiac Surgeon, Critical Care Team and
Ventricular Assist Device Team
Professionalism
At the conclusion of the Fellowship rotation, the Fellow will be able to:
1. Analyze practice experience and perform practice-based improvement activities using a
systematic methodology
2. Locate, appraise, and assimilate evidence from scientific studies related to extracorporeal
circulation
3. Apply knowledge of study designs and statistical methods to the appraisal of clinical
studies and other information on diagnostic and therapeutic effectiveness
4. Use information technology to manage information, access on-line medical information;
and support their own education
5. Facilitate the learning of residents, medical students and other health care professionals
Practice-based learning and improvement
At the conclusion of the Fellowship rotation, the Fellow will be able to:
1. Demonstrate a pattern of self-directed learning, related to extracorporeal circulatory
issues pertaining to patients under their care
2. Show an ability to use and synthesize different types of evidence into safe patient care
Systems based practice
At the conclusion of the Fellowship rotation, the Fellow will be able to:
1. Demonstrate understanding of how perfusion, IABP and VAD outcomes are related to a
multidisciplinary system of care
2. Initiate appropriate consultations with other specialists, and construct a clinical plan for
complex problems
3. Demonstrate understanding of protocols and how they impact quality and safety
Evaluation, Examination and Promotion
Sample Program Evaluations:
http://virtue.ucdenver.edu/ResidentEvaluation/SampleEvaluations.htm
A. CLINICAL COMPETENCE COMMITTEE (CCC)
Every six months, all of the evaluation forms received on each resident during the previous six
month period are tabulated and the numerical scores from each category are graphed. In addition,
comments made on each resident are summarized and test scores are reviewed. The Clinical
Competence Committee meets three times a year (or more often as specific resident needs
dictate) to review these evaluation forms. Residents receive a copy of every CCC report. Currently,
the membership of the CCC is:
Dr. Nathan Weitzel, Committee Chair
Dr. Scott Markowitz (Children’s)
Page 31 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Dr. Thomas Henthorn
Dr. Leslie Jameson
Dr. Fadi Nasrallah (UCH)
Dr. Jack Humphrey (DHHA)
Dr. Jason Krutsch (Pain Medicine)
Dr. Christopher Lace (UCH)
Dr. Glenn
Gravlee (UCH)
Residency
Program
Dr. Jake Friedman (VA)
Dr. Fareed Azam (ICU)
Dr. Randall Clark (Children’s)
Dr. Ferenc Puskas (Cardiothoracic Anesthesia)
Chief Residents
Twice a year, in January and July, a Record of Training Report on each resident is submitted to the
American Board of Anesthesiology (ABA). The information used to complete these reports comes
from the recommendations of the Clinical Competence Committee. The ABA uses these reports as
the basis for granting credit toward its Clinical Anesthesia training requirements.
B. EVALUATION AND PROMOTION
Purpose
The program recognizes the need to provide a structure by which performance related to the
training program will be assessed and consideration given for promotion to the next level of
training. Evaluation will be provided in accordance with Graduate Medical Education Committee
policy and ACGME common program requirement V.A.c: which says “a process involving use of
assessment results to achieve progressive improvements in residents' competence and
performance".
Note: This policy addresses performance relating to academic program requirements and does
not supersede other institutional or legal requirements that must be met by the resident to
remain in a training program.
Policy
Any resident participating in training will be provided, at a minimum, a semi-annual formal
evaluation developed by the Program Director. Residents shall be allowed to review semi-annual
evaluations contained in permanent records and other evaluations as determined by program
policy. The formal written evaluation shall:
Address each of the six ACGME core competencies.
Include well defined scoring and rating criteria that seek to minimize subjective
assessment of performance.
Include language indicating satisfactory performance, advancement to the next level of
training (if applicable) or provide specific actions and performance requirements by the
resident to return to a level of satisfactory performance or advancement to the next level
of training.
Be signed and dated by the resident and Program Director.
Become a part of the permanent record file for the resident.
In the event that academic status of a resident is changed to Probation or Termination a letter of
notification to the resident will be co-signed by the Associate Dean for GME. Additional
information is provided in the institutional policy titled “Grievance Policy and Procedure”.
C. EVALUATION OF RESIDENTS/FELLOWS AND FACULTY
Evaluation of residents and faculty are done monthly through the on-line evaluation program,
MedHub. See provided examples on www.virtue.ucdenver.edu/residents. Residents can view
their evaluations on line at any time by logging on to www.ucdenverMedHub.com. Residents are
encouraged to discuss their evaluations frequently with their advisors (at least semi-annually). In
addition, residents are required to complete evaluations on faculty members they have worked
Page 32 of 60
University of Colorado School of Medicine
Department of Anesthesiology
with during the month. These evaluations
are anonymous.
The process for completing and
Residency
Program
reviewing evaluations will be discussed at orientation. Similarly, faculty members are required to
complete monthly evaluations on each resident they work with during the month. They can view
their evaluations on line but cannot see which resident completed the evaluation.
D. MULTI-SOURCE EVALUATION
Residents are evaluated by nursing personnel from the operating room/PACU and the critical care
unit. These evaluations are done on line through MedHub. A sample evaluation form can be found
at www.virtue.ucdenver.edu/residents.
E. ROTATION EVALUATION
At the end of each rotation you will receive an email asking you to complete an evaluation form.
This evaluation form can be accessed through the on-line evaluation program, MedHub. A sample
evaluation form can be found at www.virtue.ucdenver.edu/residents.
F. PROGRAM EVALUATION
Once a year in May, you will be asked to complete a program evaluation/program survey. This
evaluation/survey is completed through Survey Monkey, an online survey tool.
G. EXAMINATION
1. Department of Anesthesiology Expectations
a. All Fellows, upon graduation, should successfully pass both written and oral portions of
the examinations of the American Board of Anesthesiology on the first attempt.
2. BLS/ACLS
BLS/ACLS certification is required of all residents. Classes for residents are offered through the
Anesthesiology department on an as needed basis.
Evaluation and Promotion Policy
The University of Colorado Department of Anesthesiology complies with the GME
Evaluation and Promotion Policy and the program policy is as follows:
Program Evaluation Process
Programs must use MedHub or the ACGME Residency Competency Evaluation System for the
following required evaluation types:
- Resident Performance Evaluation:
Evaluation of Fellow performance includes the following activities:
Page 33 of 60
University of Colorado School of Medicine
Department of Anesthesiology
1. Faculty evaluation of FellowsResidency
- must be completed
within 2 weeks following each
Program
rotation or educational experience and must be immediately available for review by the resident.
Resident notification of completed evaluations should be set up in MedHub by requiring that the
residents sign off on the evaluation.
2. Multiple Evaluators - Program directors must obtain and incorporate evaluative input
from multiple sources, as appropriate/available for the specialty or service, such as peers,
patients/families, self-assessment, other medical professionals, administrative and support staff,
and students.
3. Program directors must provide each Fellow with a documented performance
evaluation summary at least semi-annual, incorporating input from the Clinical Competency
Committee.
- Faculty Performance Evaluation:
The program director must evaluate faculty performance as it relates to the educational
program at least annually.
1.
Resident evaluation of Faculty – Residents must be given the opportunity to submit
confidential evaluations of faculty at the end of every rotation. Programs must not allow
faculty to view these individual evaluations by residents. Resident evaluations of faculty
must be aggregated and
made anonymous and provided to faculty annually in a summary report. This summary
may be released as necessary, with program director review and approval in instances
where evaluations are required for faculty promotions.
a. In order to maintain confidentiality of faculty performance evaluations, small
programs with four or fewer residents may use one of the following:
i. Aggregate the faculty evaluations for the subspecialty and core residency
programs to increase anonymity.
Generalize and group residents’
comments to avoid identifying specific resident feedback.
ii. Aggregate faculty performance evaluations across multiple academic years.
2. Program directors must maintain continuous and ongoing monitoring of faculty
performance.
This may include automated alerts regarding low evaluation scores on end-of-rotation
evaluations by residents, regular surveillance of end-of-rotation evaluations, and regular
verbal communication with residents regarding their experiences.
3. Division Chiefs and/or Department Chairs should be notified by the program director
when faculty receive unsatisfactory evaluation scores. Faculty performance must be
reviewed and discussed during the annual faculty evaluation review process conducted by
the Chair or Division Chief.
Page 34 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Disciplinary, Concern/Complaints,
Grievance
GME Disciplinary Policy
The University of Colorado Department of Anesthesiology complies with the GME Disciplinary
Policy linked above.
Program Concern/Complaint Policy
To ensure that residents and fellows are able to raise concerns and complaints in a
confidential and protected manner in an environment which fosters open communication
without fear of intimidation and retaliation, the University of Colorado Department of
Anesthesiology complies with the GME Concern/Complaint Policy. The program specific
concern/complaint policy is as follows:
The following options and resources are available and communicated to residessnts, fellows,
and faculty annually:
Step One
Discuss the concern or complaint to the program’s Program
Program Coordinator as appropriate.
Director,
or
Step
Two
If the concern or complaint involves the Program Director and/or cannot be addressed
in option one, residents and fellows have the option of discussing issues with the section
heads, division chiefs, and department chairs as appropriate.
Step Three
If residents are not able to resolve their concerns or complaints within the program,
they may contact the GME Designated Institutional Official (DIO) via one of the following:
• Confidential email - gme@ucdenver.edu
• Anonymous Reporting Form on the GME website:
http://www.ucdenver.edu/academics/colleges/medicalschool/education/graduateme
dicaleducatio n/concerns/Pages/form.aspx
Other Resources for Concerns and Complaints:
Page 35 of 60
University of Colorado School of Medicine
Department of Anesthesiology
1.
2.
3.
Professionalism First (Ethics Point)
is an anonymous
Residency
Programreporting mechanism for
residents and fellows to document exemplary professional behavior and identify
professional lapses of either faculty, or other residents and fellows.
http://www.ucdenver.edu/academics/colleges/medicalschool/facultyAffairs/Professio
nalismFirst/ Pages/default.aspx
Housestaff Association: 303-724-3039
http://www.ucdenver.edu/academics/colleges/medicalschool/education/graduateme
dicaleducatio n/ResidentsFellows/Pages/HousestaffAssociation.aspx
University of Colorado Ombuds Office: 303-724-2950
http://www.ucdenver.edu/about/departments/OmbudsOffice/Pages/OmbudsOffice.asp
x
GME Grievance Policy
The University of Colorado Department of Anesthesiology complies with the GME
Grievance Policy linked above. Grievances are limited to allegations of wrongful dismissal,
wrongful suspension, wrongful nonrenewal or wrongful renewal without promotion of the
annual Resident Training Agreement. Being placed on probation and immediate suspension
from clinical responsibilities are not grievable. The decision to suspend from the program,
dismiss, not renew or renew without promotion a resident is an academic responsibility and is
the decision of the University of Colorado School of Medicine Graduate Medical Education
programs.
Duty Hours
Policy
GME Duty Hours Policy
The University of Colorado Department of Anesthesiology complies with the GME Duty
Hours Policy and Procedures, linked above, which follows the intent and language found in the
ACGME guidelines.
The University of Colorado Department of Anesthesiology also complies with the Duty
Hours Process and the program specific monitoring process is outlined below.
Program Duty Hour Monitoring Process
The University of Colorado School of Medicine policy on duty hours for Residents follows
the intent and language found in the Accreditation Council for Graduate Medical Education
(ACGME) guidelines addressing this topic. All ACGME and non-ACGME programs must follow
the following principles:
1. Be committed to and be responsible for promoting patient safety and Resident
well-being and provide a supportive educational environment.
2. The learning objectives of the program must not be compromised by excessive
reliance on
Residents to fulfill service obligations.
3. Clinical education must have priority in the allotment of Residents’ time and energy.
4. Duty hour assignments must recognize that faculty and Residents collectively have
responsibility for the safety and welfare of patients.
Page 36 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
ADULT CARDIOTHORACIC ANESTHESIOLOGY
ROTATION SCHEDULE
REQUIRED:
Clinical Cardiac: 6 month, (2 month at Exempla Saint Joseph Hospital)
Clinical Thoracic: 1 month (University of Colorado Hospital)
Pediatric Congenital: 1 month (Children’s Hospital Colorado)
Critical Care: 1 month (University of Colorado Hospital)
Research: 1 month (University of Colorado Hospital or Children’s Hospital Colorado)
ELECTIVES:
Echocardiography Laboratory: 1 month (University of Colorado Hospital)
Perfusion: 1 month (University of Colorado Hospital)
Research: 1 month (University of Colorado Hospital or Children’s Hospital Colorado)
Alertness Management and Fatigue Mitigation
All residents and core faculty are required to complete GME modules on duty hours,
alertness management, fatigue and sleep deprivation. The program educates all faculty and
residents to recognize the signs of fatigue and sleep deprivation and provide education in
alertness management and fatigue mitigation processes. If any residents are too fatigued to
properly care for patients they are immediately sent home for rest. Their patient load will be
handed over to the attending supervisor and/or distributed to the rest of the residents equally.
Program Call Policy/Guidelines
Programs must educate all faculty and Fellows to recognize the signs of fatigue and
sleep deprivation; provide education in alertness management and fatigue mitigation
processes; and must adopt and apply policies to prevent and counteract the potential negative
effects on patient care and learning such as back- up call schedules and naps. All Residents
and Fellows are required to complete the online educational fatigue and sleep deprivation
module. The module is available on the GME website for faculty. Programs may provide
additional training and must identify and document faculty training methods.
Duty Hour Requirements
Duty hours are defined as all clinical and academic activities related to the
program, i.e., patient care (inpatient and outpatient), administrative duties related to patient
care, the provision for transfer of patient care, time spent in-house during call activities and
scheduled academic activities such as conferences. Duty hours do not include reading and
preparation time spent away from the duty site.
Page 37 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Averaging must occur by rotation – 4 week period, 1 month period, or the period of a
rotation if less than 4 weeks. Vacation and leave must be excluded when calculating duty
hours, call frequency or days off.
When Residents and Fellows are assigned to a rotation outside their program, the
specialty-specific Program Requirements regarding duty hours, as well as the receiving
program’s duty hour policy apply.
1. Maximum Hours of Work Per Week – 80
hour rule:
Duty hours must be limited to 80 hours per week, averaged over a four-week period,
inclusive of all in-house call activities, and internal and external moonlighting.
2. Mandatory Time Free of Duty – 1-in-7
off rule:
A. Residents must be scheduled for a minimum of 1 day free of duty every week
(when averaged over a 4-week period). At-home call cannot be assigned on these free
days.
Unusual Resident-Initiated Extensions - Additional Duty
Care of a single patient defined: Continuity for severely ill or unstable patient, academic
importance of the events transpiring, or humanistic attention to the needs of the patient or
family.) Residents must appropriately hand over care of all other patients to the team
responsible and document reasons for remaining to care for the single patient in question in
the MedHub system. The Program Director will review each submission of additional service,
and track both individual resident and program wide episodes of additional duty.
Senior Resident and Fellow - Preparation to Enter Unsupervised Practice of
Medicine
Residents in the final years of education [as defined by the ACGME Anesthesiology Review
Committee, must be prepared to enter the unsupervised practice of medicine and care for
patients over irregular or extended periods. This preparation must with the 80 hour, 28 hour
and Day off standards. There may be circumstances [as defined by the Anesthesiology Review
Committee] when senior residents must stay on duty to care for their patients or return to the
hospital with fewer than eight hours free of duty. Circumstances of return-to- hospital activities
with fewer than 8 hours away from the hospital will be monitored by the program director.
Eligibility and Selection Policy
GME Eligibility and Selection Policy
The University of Colorado Department of Anesthesiology complies with the GME Policy
regarding Eligibility and Selection, linked above, and program specific information is as follows:
Applicants eligible for appointment must meet the following qualifications to
maintain compliance with the Institutional Requirements published by the ACGME
1. Graduation from a medical school in the United States or Canada accredited by the
Liaison Committee on Medical Education (LCME); or
Page 38 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
2. Graduation from any college of Osteopathic Medicine accredited by the American
Osteopathic Association (AOA); or
3. Graduation from medical school outside of the United States or Canada and
possessing a currently valid certificate from the Educational Commission for Foreign Medical
Graduates (ECFMG) prior to appointment; or, have a full and unrestricted license to
practice medicine in Colorado; or
4. Graduation from medical schools outside the United States and completion of a Fifth
Pathway Program provided by an LCME - accredited medical school.
5. Individuals applying for Fellowship programs must document completion of an
appropriate residency program, including an ACGME-accredited residency, or meet
requirements as outlined in ACGME program requirements.
6. Programs may establish additional selection criteria. For example, determine specific
passing scores for the USMLE. Specific criteria must be published for applicants to review as
part of the required program-level policy on Eligibility and Selection.
7. Residents in our program must be a U.S. citizen, lawful permanent resident, refugee,
asylee, or possess the appropriate documentation to allow resident to legally train at the
University of Colorado Denver School of Medicine.
8. Applicants must be eligible for either a training certificate or a permanent medical
license as granted by the Colorado Medical Board.
Selection from among eligible applicants is based on residency program-related criteria
such as:
1. Ability, aptitude, academic credentials, communication skills, and personal
qualities such as motivation and integrity, and the ability to function within parameters
expected of a practitioner in the specialty.
a. Programs may select to include the GME Programs Technical Standards and
Essential Functions for Appointment and Promotion template.
http://www.ucdenver.edu/academics/colleges/medicalschool/education/graduat
emedicaleduca tion/GMEDocuments/Documents/GMETechStandards.pdf
2. To determine the appropriate level of education for individuals wishing to transfer
from another training program, the program director must receive written verification
of previous educational experiences and a statement regarding the performance
evaluation of the transferring resident prior to acceptance into the program.
3. Programs will review and select applicants in a manner consistent with provisions
of equal opportunity employment and must not discriminate with regard to sex, race,
age, religion, color, national origin, disability or any other applicable legally protected
status.
Programs are encouraged to participate in an organized matching program, where
available, such as the National Resident Matching Program (NRMP).
Page 39 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Residency and Fellowship
POLICY ON ENTRY REQUIREMENTS AND SELECTION CRITERIA
Department of Anesthesiology
University of Colorado School of Medicine
ENTRY REQUIREMENTS
The Department of Anesthesiology at the University of Colorado does not discriminate with
regard to age, sex, race, religion, national origin, disability, or Veteran status.
The Department of Anesthesiology has both advanced and categorical positions. Therefore
applicants may need to complete a PGY 1 year prior to entering the program. The PGY 1 year
must be in direct patient care in accordance with RRC specifications (review the ACGME
website for more information (www.acgme.org).
Certification by the National Board of Medical Examiners (NBME), the National Board of
Osteopathic Medicine (NBOME), or the Educational Commission for Foreign Medical
Graduates (ECFMG) is required.
International medical graduates must hold a valid ECFMG (Educational Commission for Foreign
Medical Graduates) certificate, or have a full, unrestricted license to practice medicine in a U.S.
licensing jurisdiction, or have completed a Fifth Pathway program provided by an LCMEaccredited medical school.
The University Of Colorado School Of Medicine recognizes that housestaff enrolled in its
program are trainees, not employees. As such, applicants also must be able to meet the
conditions of the school’s Houseofficer Training Agreement. Specifically, they must:
1. Be a U.S. citizen or hold a valid U.S. resident alien card;
2. Possess (or be eligible to obtain) all three of the following:
a) valid passport;
b) valid 1-94 card (obtained upon entry to the U.S.) that indicates D/S J-1 (Duration of
Status forJ-1 visa);
c) J-1 visa sponsorship from the ECFMG to train at the University Of Colorado
School Of Medicine in the Department of Anesthesiology.
SELECTION CRITERIA
1. We look for ability, aptitude, academic credentials, communication skills, and personal
qualities such as motivation and integrity, and the ability to function within parameters
expected of a practitioner in the specialty.
2. To determine the appropriate level of education for individuals wishing to transfer from
another training program, the program director must receive written verification of
Page 40 of 60
University of Colorado School of Medicine
Department of Anesthesiology
previous educational experiences and
a statement
regarding the performance evaluation of
Residency
Program
the transferring resident prior to acceptance into the program.
3. We will review and select applicants in a manner consistent with provisions of equal
opportunity employment and will not discriminate with regard to sex, race, age, religion,
color, national origin, disability or any other applicable legally protected status.
4. We participate in the National Resident Matching Program (NRMP).
5. The application deadline, except for the MSPE letter, is October 1st. Interviews are scheduled
from November through January.
Leave Policy
GME Leave Policy
The University of Colorado Department of Anesthesiology complies with the GME policy
regarding Resident/Fellow Leave, linked above. The program leave process is outlined
below.
Leave Process
This policy and procedural steps relate to Family and Medical Leave of Absence,
military leave, sick leave, vacation and other leaves of absences. Any leave time that impacts
the Resident’s ability to satisfy requirements necessary to complete the program is addressed
under Leave Documentation on page 2.
Family and Medical Leave of Absence
It is the policy of the University of Colorado School of Medicine Graduate Medical
Education Committee to allow leave for maternity, paternity, adoption, illness of a close
relative that requires the trainee’s care, or illness of the Resident. Residents may be granted
up to 12 calendar weeks of leave during a 12-month period for certain family and medical
reasons with the program holding the Resident position.
Leaves are granted at the discretion of the Program Director and with the prompt
notification of the Associate Dean for Graduate Medical Education, provided that the time
away does not cause any undue hardship for the program as defined by the Program Director.
The Program Director will determine how much of the time will need to be made up in order
to fulfill the specialty Board certification and RRC requirements.
If leave is granted, the Resident must first use the current year’s vacation and/or
educational leave as part of the leave thereby continuing to receive stipend. If the paid leave is
not desired for the first 4 weeks, but instead at a later time during the leave, OR any/all of the
leave is to be unpaid, the Program Director must state in the Leave Documentation (see below)
this exception has been made. Vacation and/or education leave cannot be used to extend
the length of the leave beyond the 12 weeks. The only paid leave available to Residents
is the 3-week vacation and/or 1-week educational leave (PGY II and above) per contract year.
Once that is exhausted, the Resident must go on unpaid leave.
Benefits during a Family and Medical Leave of Absence:
During the 12-week period of Family and Medical Leave of Absence, a funding source
Page 41 of 60
University of Colorado School of Medicine
Department of Anesthesiology
must be identified to pay the cost of maintaining
the Program
Resident’s benefit package (health,
Residency
dental, disability and life insurance) through GME.
Benefits for leaves that exceed, or are not eligible for, the 12-week period of Family
and Medical Leave:
Health and Dental: During this leave, the Resident must self-pay entire premium(s) to
maintain coverage. If the Resident is eligible and decides to continue benefits through the COBRA
continuation of the CU GME Health Benefits Plan, the Resident must follow the enrollment
procedures detailed in the Plan Document posted at
www.medschool.ucdenver.edu/gme/healthdental to obtain coverage.
Absence from Training- Vacation and
Approved Conferences
A.
VACATION LEAVE
Consistent with the policies of the American Board of Anesthesiology and the Graduate
Medical Education Committee of the University of Colorado, we as a department have
adopted the policy that fellows will be permitted three weeks of vacation per year (15
working days plus whatever weekend time can be wrapped around it.) All
vacation/educational leave requests need to be approved by the fellowship director.
DO NOT buy plane tickets or make reservations until vacations are final, otherwise, you
may have to forfeit. Vacations officially start on Monday, although every attempt is made
to give fellows the preceding weekend off. Before making any plans to leave prior to
Monday, check with your Fellowship Director,
B.
EDUCATIONAL LEAVE
Attendance at scientific meetings is optional. Per the American Board of Anesthesiology’s
Booklet of Information, March 2007, “attendance at scientific meetings, not to exceed 5
working days per year, shall be considered a part of the training program.” If a
resident/fellow chooses to attend more than 5 days of meetings, it must be taken as
vacation time. All meeting time must be approved by Dr. Puskas. The department will
fund up to a total of $2000 of meeting expenses for fellows during the one-year fellowship
period. Any expenses in excess will be the resident's responsibility. Appropriate receipts
for travel expenses will be required for reimbursement and should be given to your
Program Coordinator.
C. FAMILY/MEDICAL LEAVE
Please refer to the Policy on Family/Medical Leave and Leave of Absence in the GME 2013 - 2014
Housestaff Manual.
D. MILITARY LEAVE
Legislation exists which requires all employers to permit its employees two weeks per year
military leave without loss of any other privileges. We as a department will meet those
Page 42 of 60
University of Colorado School of Medicine
Department of Anesthesiology
requirements. However, residents who Residency
have a military
reserve or National Guard obligation must
Program
also understand the current guidelines from the ABA.
If the resident feels that while fulfilling military reserve activity he or she will be performing the
duties of an anesthesia resident (as an elective rotation at a military hospital), he/she may receive
credit for this rotation by petitioning the Credentials Committee of the ABA for prospective
approval prior to taking the rotation.
Moonlighting Policy
GME Moonlighting Policy
The University Of Colorado Department Of Anesthesiology recognizes that moonlighting
is not an activity associated with part of the formal educational experience and
complies with the GME Moonlighting Policy linked above. The GME Moonlighting
Approval Form must be completed and approved prior to engaging in moonlighting
activities. All moonlighting and additional pay for additional work hours must be
logged in Med Hub and count toward duty hours.
For reference, the GME Additional Pay for Additional Work Policy and Approval Form are
provided and linked below:
GME Additional Pay for Additional Work Policy
GME APAW Approval Form
Definitions:
External Moonlighting - any medically-related professional activity, which is
outside the course and scope of the approved training program, and takes place
at a hospital, clinic, business, or other practice site that is not a site of practice
for the program.
Internal Moonlighting–any medically-related professional activity that is
outside the course and scope of the approved training program and is provided
in a site of practice for the program.
Internal Moonlighting Billing—If a provider is submitting claims to payers
for professional services, the services may only be provided in the outpatient
setting and must be outside the course and scope of the approved training
program.
Policy
The Graduate Medical Education Committee (GMEC) recognizes that moonlighting is
not an activity associated with part of the formal educational experience. Residents
must not be required to participate in moonlighting activities.
Residents must meet the following requirements:
1. The individual wishing to moonlight must obtain annually, prior written approval
to perform specific duties/procedures in a moonlighting environment from the
Page 43 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Program Director. (CompleteResidency
the ApprovalProgram
for Resident Moonlighting request
form and return to the GME office).
2. The individual seeking permission to moonlight must possess a valid license to
practice medicine in the State of Colorado. A “Physician Training License” does not
meet this requirement. For additional information see Colorado Revised Statutes
Article 36, also known as the Medical Practice Act. 3. The individual seeking permission
to moonlight must secure professional liability (malpractice) insurance coverage apart
from that provided to residents as part of the formal academic training program.
Coverage provided residents as referred to in the residency contract do not include
activities occurring as part of a moonlighting experience.
4. Residents moonlighting at either UCH or Children’s Hospital Colorado (CHCO) must be
appointed a GME Instructor/Fellow through the Faculty Affairs Office.
5. Time spent by residents in Internal and External Moonlighting must be counted toward
the
80-hour Maximum Weekly Hour Limit as required by ACGME and GME.
6. Programs operating under an exception to the 80-hour weekly duty limit endorsed by
the GMEC and approved by the appropriate RRC may not allow residents to moonlight
while serving on rotations with a duty hour exception.
7. PGY-1 residents are not permitted to moonlight.
8. Individuals possessing a J-1 visa are not eligible to moonlight.
9. The resident must be in good standing (not on Focused Review nor Probation or
having significant performance issues).
10. Residents with prior permission to moonlight will have that permission revoked by the
Program Director if academic performance is determined to no longer be at a
satisfactory
level, e.g., probation or other major concerns arise.
11. Residents continuing to moonlight following revocation of permission can be dismissed
from the program. This notice must be contained in documentation placing the
resident on probation.
12. The obligation to notify an outside employer is the responsibility of the resident who
established that employment relationship, not the responsibility of the University
or
training program.
Physician Impairment and Health (Substance Abuse)
Policy
The University of Colorado Department of Anesthesiology complies with the GME
Physician Impairment and Health (Substance Abuse) Policy.
Page 44 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Residency and Fellowship
POLICY ON CONTROLLED SUBSTANCES
Department of Anesthesiology
University of Colorado Denver, School of Medicine
Related Policies and Procedures:
Drug and Alcohol Free Workplace
Fitness for Duty
Employee/Volunteer Health Screen
Employee Discipline
Description: University of Colorado Hospital Operating Room and the Department of
Anesthesiology are committed to a safe, healthy, and productive work environment for all
employees, free from the effects of substances that impair employee judgment, and could result in
increased safety risks, injuries, and faulty decision-making.
Accountability: All anesthesia care providers that handle controlled substances.
Definitions:
Impaired Employee: Alterations in behavior, cognitive abilities, physical agility, and
dexterity due to the ingestion of ethyl alcohol or drugs, including substances with known
mind or function altering effects on the person.
Controlled Substance/Drug: Any substance that has known mind or function-altering
effect on a person, including psychoactive substances and including but not limited to,
substances prohibited or controlled by state and federal laws. Drugs may include
prescription or nonprescription, and legal or illegal substances.
Discrepancy: A variation from a quantity expected. An OR pharmacy employee will
compare the distribution/administration records(s) [narcotic return bag] with the
anesthesia record. The amount dispensed should equal the amount given, plus the amount
to credit, if any, plus the amount to waste. Any differences found versus what was
expected in quantities returned or charted, will be considered discrepant.
Deviation: Not following established procedures in the handling, charting or safe keeping
of controlled medications, resulting in lost or uncharted medications.
Policies/Procedures:
1) The OR Pharmacy shall have locked storage for all controlled substances. All records for
controlled substances shall be maintained in a readily retrievable manner for five years.
Controlled substances records will be maintained in a manner to establish receipt and
distribution of all controlled substances. Records of all controlled substances will be maintained
separately from non-controlled medication records. The OR pharmacist will maintain a perpetual
inventory of all controlled substances used in the operating room setting. Administration and
wasting records will be maintained separately from the patient charts. An OR pharmacy employee
will compare the distribution/administration records(s) [narcotic return bag] with the anesthesia
record.
Page 45 of 60
University of Colorado School of Medicine
Department of Anesthesiology
a) If any discrepancy is found inResidency
checking theProgram
narcotic bag against the anesthesia record,
the anesthesiologist, resident, CRNA, or SRNA that signed for the controlled substances will be
questioned about the discrepancy. If there is no legitimate and verifiable accountability of the
controlled substances after twenty four hours, please refer to the protocol of section 4.
b) Poorly documented transactions, illegible handwriting or failure to document
doses/ incomplete records will be subjectively deemed as non-compliant and follow the
protocols of section 4.
2) Controlled substances procedure during satellite hours (06:30-17:00)
a) The anesthesiologist, resident, Certified Registered Nurse Anesthetist (CRNA), or
Student Registered Nurse Anesthetist (SRNA) will come to the OR Pharmacy to request specific
controlled drugs for each case or they may obtain the controlled drugs from the Pyxis Medstation.
b) The requested drug order is filled by the Pharmacist or Technician and placed in a
narcotic return bag with the patients name, date, drug, quantity, and the anesthesiologist’s,
resident’s, CRNA’s, or SRNA’s name written on the bag.
c) Each line on the controlled drug daily record (CDDR) must be filled out with the
patient's name, (last name first, first name last). The operating suite number and time can be
added if known. The record is signed by the anesthesiologist, resident, CRNA, or SRNA and
initialed by the pharmacist or technician.
i) As each drug is dispensed, the quantity dispensed is subtracted from the
previous total, so that a continuous inventory is maintained. Enter only one drug
per line.
ii) If the anesthesiologist, resident, CRNA, or SRNA obtains controlled medication
from the Pyxis Medstation, the individual fills in the required information on the
bag.
d) The amount of drug that is administered to the patient will be recorded by the
anesthesiologist, resident, CRNA, or SRNA on the patient’s anesthesia record. The drug amounts
administered, returned for credit, and amount to be wasted is recorded on the narcotic return
bag. All unused drug to waste or to credit, is placed inside the bag and returned to the pharmacy
satellite at the end of the case.
e) When the bag is returned to the Pharmacy, the Pharmacist or Technician receiving the
bag will initial the narcotic return line(s) on the CDDR sheet indicating that the narcotic bag has
been returned.
f) When the pharmacy receives a copy of the anesthesia record, all doses of controlled
drugs charted are checked against the return bag. The amount dispensed should equal the amount
given, plus the amount to credit, if any, plus the amount to waste.
i) If any discrepancy is found in checking the narcotic bag against the anesthesia
record, the anesthesiologist, resident, CRNA, or SRNA signing for drug will be
questioned about the discrepancy. If there is no resolution for the discrepancy
after twenty four hours, please refer to the protocol of section 4.
ii) A discrepancy record will be kept in the pharmacy, along with a file including a
photocopy of the narcotic bag, a photocopy of the anesthesia record and an
explanation of the discrepancy.
iii) If the anesthesiologist, resident, CRNA or SRNA fails to return the bag after the
case, the pharmacy will question the anesthesiologist, resident, CRNA or SRNA
about the missing bag. The anesthesiologist, resident, CRNA, or SRNA will write an
explanation resolving the discrepancy on the photocopy. If, after a day, the
discrepancy has not been resolved and/or the anesthesiologist, resident, CRNA or
SRNA is unavailable, please refer to the protocol of section 4.
Page 46 of 60
University of Colorado School of Medicine
Department of Anesthesiology
g) In the morning the Pharmacist
will waste the
previous day's narcotic bags. The OR
Residency
Program
Pharmacist will cosign the return bags with another available Pharmacist or Technician prior to
being wasted. The bag label will be kept in the OR Pharmacy for approximately one month and
filed in the Central Pharmacy and then eventually stored at the warehouse on file for 3 years.
3) Controlled substances procedure when satellite is not open
a) After 1700 when the satellite is not open, the resident, CRNA, SRNA, or anesthesiologist
will pick up controlled drugs from the Pyxis Medstation located in the sterile cores of the OR.
b) The resident, CRNA, SRNA, or anesthesiologist will fill in the patient’s name, date, and
the amount of each controlled drug signed out on the narcotic return bag.
c) The narcotic return bag is returned to the Pharmacy drop box at the end of the case.
The drop box is located outside of the operating room.
d) The Pharmacist collects all narcotic return bags from drop box the next "open" morning
and checks them against the inventory record and Pyxis receipt tapes and reconciles any
discrepancies according to the procedures when the OR Pharmacy is open.
e) Poorly documented transactions, illegible handwriting or failure to document
doses/incomplete records will be subjectively deemed as non-compliant and follow the
protocols of section 4.
4) Deviations from the Anesthesia Operating Room Pharmacy Controlled Substances Policy
and Procedure
a) Non-reconciled controlled substance doses, as described below, will be recorded on a
discrepancy tracking form and immediately investigated. If the discrepancy cannot be resolved
within 24 hours of discovery, the following protocol will be put into action:
i) The first incident of deviation from the controlled substances policy and
procedure will result in reporting the incident to the Department of
Anesthesiology Quality Assurance Committee and the Senior Medical
Director of Perioperative Services. The anesthesia care provider must
submit within twenty four hours of being requested to do so a written
explanation and a documented action plan to assure total compliance with
controlled substances in the future.
ii) If a second unresolved discrepancy (or deviation) by the same provider
occurs within one year, it will result in suspension from the OR schedule and
the anesthesia care provider will be sent to Concentra Clinic Labs for the
purpose of obtaining a urine/blood sample to test for controlled substances.
They will also personally appear before an emergency meeting of a quorum
of the Department of Anesthesiology Quality Assurance Committee to
explain the discrepancies. If and when the testing results are returned
negative for controlled substances the provider will then be immediately
returned to the OR schedule.
iii) The third unresolved discrepancy (or deviation) will result in suspension
from the operating room and referral to Colorado Physician Health Program
(CPHP). Reinstatement to the operating room will be based on a written
action plan for return to work agreed upon by CPHP, the referred individual,
and the Department of Anesthesiology.
Professionalism Policy
The University of Colorado Department of Anesthesiology complies with the GME
Professionalism Policy linked here.
Page 47 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
All residents/fellows must abide by the professionalism principles and guidelines as stated by
the ACGME program requirements and as detailed in the GME Professionalism Policy. In
addition, professi onals are h el d a c c o u n t a b l e t o t h e f o l lo w i n g s pec i alty -specific
board and/or society codes of medical professionalism {American Board of Anesthesiology}.
The program director and faculty monitor resident professionalism by:
Professionalism – Code of Conduct
Residents are responsible for demonstrating and abiding with the following
professionalism principles and guidelines. Physicians must develop habits of conduct that are
perceived by patients and peers as signs of trust. Every physician must demonstrate sensitivity,
compassion, integrity, respect, professionalism, and maintain patient confidentiality and privacy.
A patient’s dignity and respect must always be maintained. Under all circumstances, response to
patient needs shall supersede self-interest. A medical professional consistently transmits respect
for patients by his/her performance, behavior, attitude and appearance. Commitment to carrying
out professional responsibilities and an adherence to ethical principles are reflected in the
following expected behaviors:
A. Respect patient privacy and confidentiality.
B. Respect patient self-autonomy and the right of a patient and a family to be involved in care
decisions.
C. Respect the sanctity of the healing relationship.
D. Respect individual patient concerns and perceptions.
E. Respect the systems in place to improve quality and safety of patient care.
A professional consistently demonstrates respect for peers and co-workers:
A. Respect for colleagues is demonstrated by maintaining effective communication.
B. Respect for diversity of opinion, gender and ethnicity in the workplace.
*In addition, professionals are held accountable to specialty-specific board and/or society codes of
medical professionalism.*
Professionalism – Uniform Dress Code
Residents must adhere to the following to reflect a professional appearance in the clinical work
environment and are also held accountable to relevant individual institution policies.
Page 48 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
Residency and Fellowship POLICY ON SEXUAL
HARASSMENT Department of Anesthesiology
University of Colorado School of Medicine
The Department of Anesthesiology has adopted the University of Colorado Sexual Harassment
Policy. The policy is listed below:
INTRODUCTION
This administrative policy statement implements Regent Policy 2-J, Sexual Harassment
Policy.
POLICY STATEMENT
The University of Colorado is committed to maintaining a positive learning, working and living
environment. The University does not discriminate on the basis of race, color, national origin,
sex, age, disability, creed, religion, sexual orientation, or veteran status in admission and
access to, and treatment and employment in, its educational programs and activities. (Regent
Law, Article 10, amended 11/8/2001). In pursuit of these goals, the University will not tolerate
acts of sexual harassment or related retaliation against or by any employee or student.
This Policy (1) provides a general definition of sexual harassment and related retaliation;
(2) prohibits sexual harassment and related retaliation; and (3) sets out procedures to
follow when a member of the University community believes a violation of the Policy has
occurred. It is also a violation of this Policy for anyone acting knowingly and recklessly either
to make a false complaint of sexual harassment or to provide false information regarding a
complaint.
Robust discussion and debate are fundamental to the life of the University. Consequently,
this policy shall be interpreted in a manner that is consistent with academic freedom as
defined in Regent Law, Article 5 D (amended 10/10/02). It is intended that individuals who
violate this Policy be disciplined or subjected to corrective action, up to and including
termination or expulsion.
DEFINITIONS
Appointing authority/disciplinary authority: an appointing authority is the individual with the
authority or delegated authority to make ultimate personnel decisions concerning a particular
employee. A disciplinary authority is the individual who has the authority or delegated
authority to impose discipline upon a particular employee.
Complainant: a complainant is a person who is subject to alleged sexual harassment.
Respondent: a respondent is a person whose alleged conduct is the subject of a complaint.
Sexual harassment: sexual harassment consists of interaction between individuals of the same
or opposite sex that is characterized by unwelcome sexual advances, requests for sexual
favors, and other verbal or physical conduct of a sexual nature when: (1) submission to such
Page 49 of 60
University of Colorado School of Medicine
Department of Anesthesiology
conduct is made either explicitly or implicitly
a term orProgram
condition of an individual's
Residency
employment, living conditions and/or educational evaluation; (2) submission to or
rejection of such conduct by an individual is used as the basis for tangible employment or
educational decisions affecting such individual; or (3) such conduct has the purpose or effect of
unreasonably interfering with an individual's work or academic performance or creating an
intimidating, hostile, or offensive working or educational environment.
Hostile environment sexual harassment: (described in subpart (3) above) is unwelcome
sexual conduct that is sufficiently severe or pervasive that it alters the conditions of education
or employment and creates an environment that a reasonable person would find intimidating,
hostile or offensive. The determination of whether an environment is "hostile" must be based on
all of the circumstances. These circumstances could include the frequency of the conduct, its
severity, and whether it is threatening or humiliating. Examples which may be Policy
violations include the following: an instructor suggests that a higher grade might be given to a
student if the student submits to sexual advances; a supervisor implicitly or explicitly
threatens termination if a subordinate refuses the supervisor's sexual advances; and a student
repeatedly follows an instructor around campus and sends sexually explicit messages to the
instructor's voicemail or email.
Retaliatory Acts: It is a violation of this policy to engage in retaliatory acts against any employee or
student who reports an incident of alleged sexual harassment, or any employee or student who
testifies, assists or participates in a proceeding, investigation or hearing relating to such
allegation of sexual harassment. Students and employees who believe they have been
retaliated against because of testifying, assisting or participating in a proceeding,
investigation, or hearing relating to an allegation of sexual harassment, should meet with and
seek the advice of their campus sexual harassment officer, whose responsibilities include handling
retaliation.
POLICIES AND PROCEDURES
A.
Obligation to Report
In order to take appropriate corrective action, the University must be aware of sexual
harassment or related retaliation. Therefore, anyone who believes that s/he has experienced
or witnessed sexual harassment or related retaliation should promptly report such behavior to
a campus sexual harassment officer (see campus Appendix discussed below) or any
supervisor (see section B below).
B.
Supervisor's Obligation to Report
Any supervisor who experiences, witnesses or receives a written or oral report or complaint
of sexual harassment or related retaliation shall promptly report it to a campus sexual
harassment officer. This section of the Policy does not obligate a supervisor who is required
by the supervisor's profession and University responsibilities to keep certain communications
confidential (e.g., a professional counselor or ombudsperson) to report confidential
communications received while performing those University responsibilities. Each campus
shall have an appendix to this Policy designating the supervisory positions that qualify under
this exception.
C.
Investigation Process
1. Reports or complaints under this Policy shall be addressed and resolved as promptly as
practicable after the complaint or report is made. Ordinarily, investigations shall be
concluded and reports submitted to the reviewing committee no later than 90 days
following the receipt of a complaint. Ordinarily, the final report shall be sent to the Chancellor
or President no later than 30 days after the committee's receipt of the draft report of the
investigation.
Page 50 of 60
University of Colorado School of Medicine
Department of Anesthesiology
It is the responsibility of the sexual harassment
officer(s)
to determine the most appropriate means for
Residency
Program
addressing the report or complaint. Options include: 1) investigating the report or complaint in
accordance with paragraph C.3. Below, 2) with the agreement of the parties, attempting to resolve
the report or complaint through a form of alternative dispute resolution (e.g., mediation), or
3) determining that the facts of the complaint or report, even if true, would not constitute a
violation of this Policy. The campus sexual harassment officer(s) may designate another individual
(either from within the University, including an administrator, or from outside the University) to
conduct or assist with the investigation or to manage an alternative dispute resolution process.
Outside investigators shall have training, qualifications and experience as will, in the judgment of
the sexual harassment officer, facilitate the investigation. Anyone designated to address an
allegation must adhere to the requirements of this Policy and confer with the sexual harassment
officer(s) about his or her progress. (See campus appendix for a list of resources for further
assistance or additional information.)
2. All reports or complaints shall be made as promptly as feasible after the occurrence. (A
delay in reporting may be reasonable under some circumstances, as determined on a
case-by-case basis. An unreasonable delay in reporting, however, is an appropriate
consideration in evaluating the merits of a complaint or report.)
3. If an investigation is conducted: The complainant and the respondent shall have the right to:
a. Receive written notice of the report or complaint, including a statement of the
allegations, as soon after the commencement of the investigation as is practicable and to the
extent permitted by law; b. Present relevant information to the investigator(s); and
c. Receive, at the conclusion of the investigation and appropriate review, a copy of the
investigator's report, to the extent permitted by law.
4. The Chancellor, the respondent's appointing authority and the respondent's supervisor
shall be notified that an investigation is taking place. The sexual harassment officer shall advise
the respondent's supervisor whether the respondent should be relieved of any supervisory or
evaluative authority during the investigation and review. If the respondent's supervisor
declines to follow the recommendation of the sexual harassment officer, s/he shall send a
letter explaining the decision to the Chancellor with a copy to the sexual harassment officer.
5. At the conclusion of an investigation, the investigator shall prepare a written report which
shall include a statement of factual findings and a determination of whether this Policy has
been violated. The report shall be presented for review to the standing review committee
designated by the Chancellor, or, in the case of System Administration, the President.
6. The standing review committee may consult with the investigator, consult with the parties,
request that further investigation be done by the same or another investigator, or request
that the investigation be conducted again by another investigator. The standing review
committee may adopt the investigator's report as its own or may prepare a separate report
based on the findings of the investigation. The standing review committee may not,
however, conduct its own
investigation or hearing. Once the standing review committee has completed its review, the
report(s) shall be sent to the campus sexual harassment officer(s), the complainant and the
respondent, to the extent permitted by law. The report shall also be sent to the Chancellor,
or, in the case of System Administration*, to the President. If a Chancellor is the respondent or
complainant, the report shall be sent to the President. If the President or the Secretary of the
Board of Regents is the respondent or complainant, the report shall be sent to the Board of
Regents.
*For the purposes of this Policy, System Administration includes the Office of the Secretary of the
Board of Regents and Internal Audit.
Page 51 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
D.
Reporting Process
1. A. If a Policy violation is found, the report(s) shall be sent to the disciplinary authority for the
individual found to have violated the Policy, and the disciplinary authority must initiate a disciplinary
process against that individual. The disciplinary authority shall have access to the records of the
investigation. If disciplinary action is not taken, the appointing authority and the Chancellor, or
in the case of System Administration, the President, shall be notified accordingly.
b. Following a finding of violation of the Policy, the disciplinary authority shall forward to the
sexual harassment officer and to the Chancellor, or in the case of System Administration, the
President, and a statement of the action taken against an individual for violation of this
Policy.
c. I f a Policy violation is not found, the appointing authority and the Chancellor, or in the case of
System Administration, the President, shall be notified accordingly.
2. The sexual harassment officer shall advise the complainant and respondent of the
resolution of any investigation conducted under this Policy.
3. A copy of the investigator's written report as approved by the standing review committee
shall be provided to: (1) the complainant; (2) the respondent; and (3) the respondent's
appointing authority.
4. In all cases, the sexual harassment officer shall retain the investigator's report, as
approved by the standing review committee, for a minimum of three (3) years or for as long as
any administrative or legal action arising out of the complaint is pending.
5. All records of sexual harassment reports and investigations shall be considered
confidential and shall not be disclosed publicly except to the extent required by law.
6. Complaints involving two or More Campuses: When an alleged Policy violation involves
more than one campus, the complaint shall be handled by the campus with disciplinary
authority over the respondent. The campus responsible for the investigation may request the
involvement or cooperation of any other affected campus and should advise
appropriate officials of the affected campus of the progress and results of the investigation.
7. Complaints By and Against University Employees and Students Arising in an Affiliated
Entity: University employees and students sometimes work or study at the worksite or program
of another organization affiliated with the University. When a Policy violation is alleged by or
against University employees or students in those circumstances, the complaint shall be
handled as provided in the affiliation agreement between the University and the other entity. In
the absence of an affiliation agreement or a provision addressing this issue, the University may,
in its discretion, choose to 1) conduct its own investigation, 2) conduct a joint investigation with
the affiliated entity, 3) defer to the findings of an investigation by the affiliated entity where the
University has reviewed the investigation process and is satisfied that it was fairly conducted, or
4) use the investigation and findings of the affiliated entity as a basis for further investigation.
E.
No Limitations on Existing Authority
No provision of this Policy shall be construed as a limitation on the authority of a disciplinary
authority under applicable policies and procedures to initiate disciplinary action. If an
individual is disciplined for conduct that also violates this Policy, the conduct and the
discipline imposed shall be reported to a campus sexual harassment officer. If an
investigation is conducted under this Policy and no Policy violation is found, that fact does not
prevent discipline of the respondent for inappropriate or unprofessional conduct under other
applicable policies and procedures.
Page 52 of 60
University of Colorado School of Medicine
Department of Anesthesiology
F.
Information and Education Residency Program
The President's office shall provide an annual report documenting: (1) the number of reports or
complaints of Policy violations; (2) the categories (i.e., student, employee, or other) and sexes of the
parties involved; (3) the number of Policy violations found; and (4) examples of sanctions imposed
for Policy violations.
Each campus shall broadly disseminate this Policy, distribute a list of resources available on
the campus to respond to concerns of sexual harassment and related retaliation, maintain the
campus appendix to the sexual harassment policy, and develop and present appropriate
educational programs. Each campus shall maintain information about these efforts, including a
record of how the Policy is distributed and the names of individuals attending training
programs.
G.
Oversight Committee
There shall be an oversight committee consisting of campus and system representatives
appointed by the President. No one shall serve on this committee who has been involved with a
sexual harassment case in any capacity during the previous two years. The oversight
committee shall annually gather and review information regarding investigations conducted
under this Policy and the ultimate actions taken as a result of such investigations. The
oversight committee shall b e r e s p o n s i b l e f o r m a k i n g c o n f i d e n t i a l f i n d i n g s a n d
recommendations to the University Counsel for the purpose of enabling the University
Counsel to provide legal advice to the Board, the President, the campus Chancellors, and other
University officials, as appropriate concerning the equitable, effective and lawful
implementation of the policy.
H.
Review of the University Policy
Pursuant to the University Policy on Sexual Harassment, effective July 1, 1999, the Policy
underwent review and revision in 2000-2003. In accordance with this Policy as reviewed and
revised in 2003, the President shall periodically have this Policy reviewed.
RELATED POLICIES
Administrative Policy Statement, "University Policy on Amorous Relationships Involving
Evaluative Authority," provides that an amorous relationship between an employee and a
student or between two employees constitutes a conflict of interest when one of the
individuals has direct evaluative authority over the other and requires that the direct
evaluative authority must be eliminated.
For related complaint, grievance or disciplinary processes refer to Regent Policies under 5.
Faculty, 5. H. Faculty Senate Grievance Process and 5. I. Faculty Dismissal for Cause Process
(for faculty), State Personnel Board Rules (for classified employees), and campus student
disciplinary policies and procedures (for students).
UCD Sexual Harassment Policy Campus Appendix
Campus Resources:
If you wish to report sexual harassment or need additional information, contact the UCD Sexual
Harassment Officer at (303) 315-2724; send correspondence to PO Box 173364, Campus
Box 130, Denver CO 80217-3364; or email richard.webb@uch.edu.
The Ombuds Office is a resource available to all members of the University community. It is an
independent entity which will provide informal, confidential and neutral services to
members of the university community in resolving conflicts, complaints, and disputes. For the
downtown Denver campus office call (303) 556-4493. For the office serving the AMC call
(303) 724-2950.
Page 53 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
The Associate Dean in the GME Office is also a resource for assistance in resolving complaints
of sexual harassment. The supervisor who receives the complaint is obligated to report it to
the UCD Sexual Harassment Officer. The Resident should also inform the UCD Sexual
Harassment Officer.
UCD Department of Human Resources is located on the downtown Denver campus. The
Department provides services to faculty, exempt professional and classified staff. Phone:
(303) 315-2700.
The emergency phone number for police serving all campuses is 911.
The CU-Denver Student and Community Counseling Center serving the downtown Denver
campus is located in room 4036 of the North Classroom Building. (303) 556-4372.
Exception to the Obligation to Report:
The Sexual Harassment Policy obligates supervisors who experience, witness or receive written
or oral reports or complaints of sexual harassment or related retaliation to promptly report the
information to a campus sexual harassment officer. The policy also requires that exceptions to
this requirement be identified. The Ombuds Office at UCD is not required to inform the
sexual harassment officer of confidential communications, including information regarding
sexual harassment.
Source: President's Office
Prepared by: Associate Vice President for Human Relations and Risk Management
Approved by: Elizabeth Hoffman
Application: All Campuses and System Administration
Effective Date: July 1, 2003
Replaces: University Policy on Sexual Harassment
Quality Improvement and Patient Safety Guidelines
The University of Colorado Department of Anesthesiology complies with the GME Quality
Improvement and Patient Safety Policy linked here.
Quality Improvement/Patient Safety activities include but are not limited to the following:
-
Quality Improvement/Patient Safety Conferences (e.g., Morbidity and Mortality)
Participation in institutional Quality Management Committees
Grand Rounds
Patient Satisfaction Surveys
Core Measures
Utilization Management
Elective Quality Improvement rotations (e.g., LEAN)
Scholarly activity resulting in implementation of initiatives to improve patient
quality and safety of care
Policy:
Each residency and fellowship program must ensure each resident participates in Quality
Improvement/Patient Safety activities. The level of participation will vary depending on the
Page 54 of 60
University of Colorado School of Medicine
Department of Anesthesiology
functional
Residency Program
role of the resident or fellow in patient care and the QI/PS activities currently
underway within the clinical setting and institution.
1. At a minimum, every training program must incorporate Quality
Improvement/Patient Safety Conferences (e.g., Morbidity and Mortality) into its
curriculum, including use of the prescribed Patient Safety/M&M/Occurrence
Review Form if applicable to the institution.
2. At least annually, in conjunction with the Annual Program Evaluation, the Designated
Institutional Official for GME will provide the GMEC with a report of QI/PS
activities as they pertain to the residents and the teaching programs.
3. The DIO will address any concerns identified regarding insufficient QI/PS involvement.
Research / Scholarly Activity
Guideline
Scholarly Activity
Scholarly activity is a requirement for successful completion of the residency program. In
so much, each resident is required to research, prepare and present a lecture for their
peers, faculty, and medical students. The requirements are as follows:
Research, prepare and present:
CA 2 Year- 1 Journal Club Presentation
CA 3 Year- 1 Senior Lecture
Supervision
Policy
GME Supervision Policy
The University of Colorado Department of Anesthesiology follows the GME Supervision
Policy linked above.
To ensure oversight of resident supervision and graded authority and responsibility, the
program follows the ACGME classification of supervision (CPR VI.D.3):
Program Supervision Policy
.
Each patient must have an identifiable, appropriately-credentialed and privileged
attending physician (or
licensed independent practitioner as approved by each Review Committee) who is
ultimately responsible for that patient’s care. This information should be available to
residents, faculty, and patients. Residents and faculty members should inform patients of
their respective roles in each patient’s care.
Page 55 of 60
University of Colorado School of Medicine
Department of Anesthesiology
All Residents working in clinical Residency
settings mustProgram
be supervised by a licensed physician.
Within the State of Colorado, the supervising physician must hold a regular faculty or
clinical faculty appointment from the University of Colorado School of Medicine. For
clinical rotations occurring outside of Colorado the supervising physician must be
approved by the training Program Director.
The program must demonstrate that the appropriate level of supervision is in place for all
Residents who care for patients. To ensure oversight of Resident supervision and graded
authority and responsibility, the program must use the ACGME classification of supervision
(CPR VI.D.3):
Direct Supervision:
The supervising physician is physically present with the
Resident and patient.
Indirect Supervision:
With direct supervision immediately available – the supervising physician is
physically within the hospital or other site of patient care, and is immediately
available to provide Direct Supervision.
With direct supervision available – the supervising physician is not physically
present within the hospital or other site of patient care, but is immediately
available by means of telephonic and/or electronic modalities, and is available to
provide Direct Supervision.
Oversight:
The
supervising
physician
is
available
to
provide
review
procedures/encounters with feedback provided after care is delivered.
of
The privilege of progressive authority and responsibility, conditional independence,
and a supervisory role in patient care delegated to each resident must be assigned by the
program director and faculty members. The program director must evaluate each
resident’s abilities based on specific criteria, and per specific national standards-based
criteria when available.
Residency and Fellowship
POLICY ON SUPERVISION
Department of Anesthesiology
University of Colorado School of Medicine
Supervision
The attending provider is responsible for all care delivered by trainees. Trainees shall always be
appropriately supervised and the supervision of trainees is ultimately the responsibility of the attending
provider, who is accountable to the Medical Board. Each department shall have a mechanism in place
that communicates to the trainees the identity of the attending provider and back-up coverage by
another faculty member in the event that the attending provider is not immediately available.
Page 56 of 60
University of Colorado School of Medicine
Department of Anesthesiology
In the Department of Anesthesiology, residency
trainingProgram
is 3 clinical years. Candidates begin at the
Residency
PGY-2 level and complete training at the PGY-4 level. Fellowship or subspecialty training begins at the
PGY-4 level and finishes at the PGY-5 level.
If your program does NOT begin at the PGY1 level, in what specialty do your residents train for
the first year(s)?
The American Board of Anesthesiology allows almost any medical or surgical specialty. Many do their
PGY-1 year as a Transitional Internship. We initiated a PGY-1 year in 2010 that includes 9 months of
rotations in Internal Medicine, 2 months Emergency Medicine, and 1 month Anesthesiology. Only 4 out
of 12 residents in each class come through our PGY-1 year.
Please provide a narrative description of the ongoing resident evaluation and promotion
process for both cognitive and procedural skills. This should include the faculty evaluation
process, in-service examination, and residency/promotions committee process:
Anesthesiology residents are evaluated by the faculty at the completion of each rotation. The
Clinical Competence Committee meets three times each year to review resident performance and
make decisions regarding resident progression through the program. These decisions are based
on the residents’ clinical and technical skills, professionalism and results on the American Board
of Anesthesiology In-Training examinations as well as other standardized tests administered
during the CA-1 (PGY-2) and CA-2 (PGY-3) years.
Definitions
Resident: The term resident refers to individuals who are engaged in graduate medical education
training, including interns, residents, and fellows.
Fellow: Any individual engaged in any training period after already taking or qualifying for Board
Certification in their specialty.
Supervision: Refers to the authority and responsibility that a staff practitioner, as attending,
exercises over the care delivered to a patient by a resident or fellow.
Direct Supervision: Requires the presence of the attending faculty or supervising
resident, appropriate record keeping, and direct involvement of the attending faculty
or supervising resident during follow-up.
Indirect Supervision: Requires appropriate record keeping and discussion with
attending faculty or supervising resident either before or after the procedure.
LEVELS OF SUPERVISION
The trainee
will not be
performing
the
procedure
NA
Faculty
Present
(Direct)
1
Faculty in
hospital and
available for
consultation
(Indirect)
Faculty out
of hospital
but
available by
phone
(Indirect)
2
3
Supervising
Resident
Present
(Direct)
Supervising
Resident in
hospital and
available for
consultation
(Indirect)
Supervising
Resident out of
hospital but
available by
phone (Indirect)
The trainee
may perform
the
procedure
without any
supervision or
oversight
4
5
6
IND
Assign a supervisory level (NA, 1 – 6, or IND) to every procedure for every level of trainee.
NON-PROCEDURAL ACTIVITIES
Admit patients to this service
Perform History and Physical
Examination for patients on this service
PGY-2
PGY-3
PGY-4
NA
NA
NA
2
2
2
Page 57 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency
Treat and Manage patients on this service
2 Program
2
2
Make referrals and request consultations
Provide consultations within the scope
of his or her expertise
Use all skills normally learned during
medical school
1
1
1
2
2
2
IND
IND
IND
Render any care in a life-threatening
emergency
Supervise Allied Health Professionals
on this service
IND
IND
IND
NA
NA
NA
GENERAL PROCEDURES
Administration of surgical anesthesia
PGY-2
1
PGY-3
1
PGY-4
1
SPECIAL PROCEDURES
Insertion of peripheral arterial catheters
Pulmonary artery catheterization
Endotracheal intubation
Insertion of central venous catheters
Pain Management:
Consultation
Epidural analgesia
Nerve block analgesia
PGY-2
2
1
1
2
PGY-3
2
1
2
2
PGY-4
2
1
2
2
2
1
1
2
2
2
2
2
2
Rev. 4/2011
Transitions of Care Guidelines – Hand-off Process
Transitions of Care Guidelines – Hand-off Process
The University of Colorado Department of Anesthesiology complies with the Departments
of Anesthesiology, Surgery, and Neurosurgery
OR to ICU Handoff and Patient Care Guideline
This guideline is designed to improve the handoff process, ensure superior communication between
the surgical, anesthesia, and ICU teams, and provide coordinated care for all critically ill patients.
This guideline will be followed for all patients destined for the SICU, CTICU, and NeuroICU, whether
admitted directly from the OR or transferred to the PACU prior to admission to the ICU. Discussion on
plans for ICU versus floor admission should be discussed between surgical and anesthesia teams prior
to the completion of surgery.
The SICU and CTICU teams carry dedicated cell phones. The NeuroICU team is available by pager.
These numbers can be used to reach the ICU teams 24 hours a day, 7 days a week.
Page 58 of 60
University of Colorado School of Medicine
Department of Anesthesiology
SICU – 85916
Residency Program
CTICU – 83253
NeuroICU – 303-266-2353
* For Spine Cases – Burger/Patel admit to SICU, Witt/Finn admit to NeuroICU
After completion of signout to the ICU team, the ICU team will assume all patient care responsibilities.
This includes all care decisions during PACU admission prior to ICU transfer. PACU nursing team
members have been instructed to direct all communications to the ICU team.
The anesthesia and surgery teams will continue to place initial post-operative care orders.
Surgery Signout
During anesthesia emergence or directly following completion of the operative case, the operating
surgeon will call the ICU team with a signout for the patient being admitted. This communication will
include the following elements:
1.
2.
3.
4.
5.
6.
7.
Surgical procedure
Any complications
Drains
Planned perioperative antibiotics
Postoperative labs to be ordered and followed
Any special concerns/requests for postoperative care
A phone number to be reached (R2 resident or greater) for further communication
Anesthesia Signout
In the OR prior to completion of the case or on transfer to the PACU or ICU, the anesthesia
resident/CRNA/attending will call the ICU team for signout. This communication will include the
following information:
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
Pertinent past medical history
Allergies
Preoperative vital signs and clinical condition
Type of anesthesia, including any regional/nerve block adjuncts
Total I/O’s (including blood loss and any transfusions)
Any airway difficulties
Any significant hypotension or hemodynamic instability, including treatment
Any ICP related issues (Neurosurgery)
Any special concerns for postoperative care (including pain control)
A phone number to be reached for further communication
GME USMLE (and COMLEX) Examinations
The University of Colorado Department of Anesthesiology complies with the GME
Policy on USMLE (and COMLEX) Examinations.
Page 59 of 60
University of Colorado School of Medicine
Department of Anesthesiology
Residency Program
University Policy:
All Residents in GMEC approved programs are required to successfully complete the
USMLE Step 2 (CS and CK) or COMLEX Level 2 (CE and PE) examination, as evidenced by
obtaining a passing grade for that examination, prior to the mid-point in the first post-graduate
year (PGY1). Failure to demonstrate passage within the stated timeline may result in non-renewal
from the training program at the end of the academic year.
All Residents in GMEC approved programs are required to successfully complete the
USMLE Step 3 examination or COMLEX Level 3 examination, as evidenced by obtaining a passing
grade for that examination, prior to the mid-point of the second post-graduate year (PGY2).
Failure to demonstrate passage within the stated timeline may result in non-renewal or
termination from the training program at the end of the academic year.
All Fellows entering GMEC approved programs must have successfully completed the
USMLE Step 3 examination, COMLEX Level 3 examination or the Canadian LMCC examination, as
evidenced by obtaining a passing grade for that examination prior to starting a fellowship.
ACGME Specific Program Requirements
The program will provide current Accreditation Council for Graduate Medical Education
program requirements within this Program Manual annually.
Procedure:
1. Each Department must have an “Education Committee” or equivalent committee or committees
that oversee all ACGME programs.
2. Committee membership. The committee should include at least the following individuals: a. The
Program Director.
b. At least three faculty members involved in education who are full-time university
faculty members.
c. At least one resident from the program.
d. The Division Director or Department Chair should serve as an ex-officio member of the
committee.
e. It is recommended that at least one faculty member from each major participating
institution for the program be included on the committee.
3. Committee logistics. a. Committee meeting minutes must be available at the time of the
program internal review and site review. Programs may use the Annual Program Evaluation and
Action Plan template for the meeting minutes.
4. Committee responsibilities.
a. Program Action Plan.
1) Based on the program’s annual self-assessment, the program director will develop a written
improvement action plan. The approval of this plan should be recorded in the committee minutes.
2) The program improvement action plan must be forwarded to the GME office by August 1st of
each year as part of the Annual Program Evaluation & Action Plan template.
Page 60 of 60