Respiratory failure 1. Insufficiency of external breathing is
advertisement

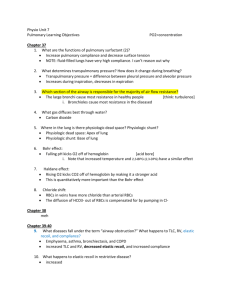
Respiratory failure 1. Insufficiency of external breathing is accompanied by: a) increasing the partial pressure of oxygen (pO2) and carbon dioxide (pCO2) in the blood; b) an increase in the pO2 and decrease pCO2 in blood; c) a decrease in pO2 and pCO2 in blood; + d) a decrease in pO2 and increase pCO2 in blood; e) an increase in pO2 and normal pCO2 in blood. 2. Centrogenic ventilation failure occurs when: a) lung diseases; b) the pathology of internal breathing; + c) pathology of the respiratory center; d) pathology of respiratory muscles; e) pathology of pleura. 3. Inhibition of the respiratory center leads to: a) the diffusion form of respiratory failure; + b) ventilation form of respiratory failure; c) perfusion form of respiratory failure; d) obstructive type of violations of the pulmonary ventilation; e) the valve mechanism of bronchial obstruction. 4. Alveolar hypoventilation is characterized by: + a) hypoxemia, hypercapnia, acidosis; b) hyperosmia, hypocapnia, alkalosis. 5. Obstructive type of hypoventilation develops at: a) damage of motor neurons of the spinal cord; b) restriction of unfolding of the lungs during breathing; c) decrease in pulmonary surface; + d) impaired patency of the airway; e) inhibition of the function of the respiratory center. 6. Obstructive type of hypoventilation develops at: + a) reducing of the total lumen of bronchi; b) the restriction of unfolding of the lungs during breathing; c) decrease in pulmonary surface; + d) impaired patency of the airway; e) inhibition of the function of the respiratory center. 7. Obstructive type of respiratory failure occurs wnen: a) pulmonary fibrosis; b) pneumonia; c) fracture of ribs; d) paralysis of the respiratory center; + e) bronchospasm. 8. Obstructive type of respiratory failure occurs when: a) pulmonary fibrosis; b) pneumonia; c) fracture of the ribs; d) paralysis of the respiratory center; + e) laryngospasm. 9. Obstructive respiratory failure may be due to: a) inhibition of the respiratory center; b) pulmonary edema; + c) pulmonary emphysema; d) spasm of smooth muscles of the diaphragm; e) pulmonary fibrosis. 10. Obstructive respiratory failure develops as a result of: a) inhibition of the respiratory center; b) pulmonary edema; + c) spasm of smooth muscles of the bronchial tubes; d) spasm of smooth muscles of the diaphragm; e) pulmonary fibrosis. 11. Obstructive type of hypoventilation occurs when: + a) spasm of the bronchi and bronchioles; + b) thickening of the bronchial mucosa; c) violation of the respiratory muscles; + d) laryngeal edema; e) reduction of the respiratory surface of the lungs. 12. Restrictive respiratory failure develops as a result of: + a) diffuse pulmonary fibrosis; b) airway edema; c) obstructive airways disease; d) spasm of bronchial smooth muscle; e) compression of the airway. 13. Restrictive type of hypoventilation occurs when: a) laryngeal edema; b) hypersecretion of the bronchial mucosa; c) spasm of bronchioles; d) strangulation; + e) pleuritis. 14. Restrictive type of hypoventilation develops wnen: a) reducing the total lumen of the bronchi; + b) restriction of the unfolding of the lungs during breathing; + c) reduction of pulmonary surface; d) violation of patency of the airway; e) spasm of bronchioles. 15. Restrictive respiratory failure develops as a result: a) airway edema; b) obstructive airways; c) spasm of bronchial smooth muscle; + d) removal of the lung; e) compression of the airway. 16. Restrictive type of hypoventilation occurs when: a) swelling of the bronchial mucosa; + b) surfactant deficiency; c) spasm of bronchioles; d) bronchial asthma; e) hypersecretion of mucus by bronchial epithelium. 17. Restrictive type of hypoventilation occurs when: a) laryngeal edema; b) hypersecretion of the bronchial mucosa; + c) pulmonary edema; + d) pneumonia; + e) pleuritis. 18. Perfusion form of respiratory failure develops at: a) shock; b) embolism of branches of the pulmonary artery; c) the weakening of the contractile function of the heart; + d) all of the above. 19. The distance for diffusion of gases can be increased: a) during hyperventilation; b) in violation of the mechanics of breathing; c) by increasing the number of functioning alveoli; + d) wnen fibrotic changes in the lungs; e ) the depression of the respiratory center. 20. Shortness of breath - is: a) hyperpnea; b) tachypnea; c) bradypnea; d) gasping breath; + e) dyspnea. 21. Shortness of breath is: a) frequent, deep breathing; b) frequent, shallow breathing; c) rare, deep breathing; d) rare, shallow breathing; + e) sense of lack of the air. 22. Hyperpnea is: a) rare breath; b) stenotic breathing; + c) frequent, deep breathing; d) frequent, shallow breathing; e) deep, rare breath. 23. Hyperpnea is observed at: + a) altitude sickness; b) increase in blood pressure; c) pneumonia; d) the action of drugs; e) depression of the respiratory center. 24. Bradypnea is: + a) rare breath; b) frequent, deep breathing; c) frequent, shallow breathing; d) periodic breathing; e) respiratory arrest. 25. Bradypnea is observed at: a) lowering blood pressure; + b) depression of the respiratory center; c) heart failure; d) hypoxia; e) pneumonia. 26. Tachypnea is: + a) frequent, shallow breathing; b) frequent, deep breathing; c) non-rhythmic breathing; d) deep, rare breath; e) rare, shallow breathing. 27. Tachypnea is observed at: a) drug poisoning; + b) pneumonia; c) edema of the larynx; + d) fever; e) increase in blood pressure. 28. Periodic breathing is: a) tissue; b) dissociated; c) Kussmaul; d) gasping; + e) Cheyne-Stokes 29. Periodic breathing is: a) breathing with changing the ratio between inhalation and exhalation; + b) alternating periods of breathing with periods of apnea; c) rapid breathing; d) breathing with varying amplitude; e) respiratory arrest. 30. In the pathogenesis of periodic breathing is important: + a) reducing the sensitivity of the respiratory center to CO2; b) the increased sensitivity of the respiratory center to CO2; c) stimulation of the respiratory center; d) the constant stimulation of inspiratory neurons of the respiratory center; e) reduction of the respiratory surface of the lungs. 31. Biot's respiration is: a) the alternation of apnea with respiratory movements that are growing by depth, and then decrease; + b) the alternation of apnea with respiratory movements of the same frequency and depth; c) deep, rare respiratory movements; d) deep, frequent respiratory movements; e) gradually fading respiratory movements. 32. Cheyne-Stokes respiration - is: + a) the alternation of apnea with respiratory movements that are growing by depth, and then decrease; b) the alternation of apnea with respiratory movements of the same frequency and depth; c) deep, rare respiratory movements; d) deep, frequent respiratory movements; e) gradually fading respiratory movements. 33. Terminal breathing include breathing of: a) Biota; b) Cheyne-Stokes; c) external; d) dissociated; + e) gasping. 34. The main pathogenic factor in the development of pulmonary edema is: a) reduction in vascular permeability; b) reduction of lymph flow; c) increasing the colloid osmotic pressure of the plasma; d) increasing the production of aldosterone; + e) increasing hydrostatic pressure in the pulmonary capillaries. 35. Respiratory failure is characterized by: +a) shortness of breath; b) anemia; + c) cyanosis; + d) changes in the content of O2 and CO2 in the blood; + e) changes in acid-base status. 36. What type of breathing develops in stenosis of the larynx? a) frequent, shallow breathing (polypnoea); b) frequent, deep breathing (hyperpnoea); c) rare, deep breathing with difficulty exhaling; + d) rare, deep breathing with difficulty inhaling; e) Biot's respiration. 37. Inspiratory dyspnea is observed the following pathological conditions: + a) I stage of asphyxia; b) emphysema of lungs; + c) laryngeal edema; d) bronchial asthma; + e) tracheal stenosis. 38. Expiratory dyspnea is observed the following pathological conditions: a) I stage of asphyxia; + b) emphysema of lungs; c) laryngeal edema; + d) bronchial asthma; e) tracheal stenosis. 39. Describe the breath when inspiratory dyspnea: a) constant amplitude; b) superficial; + c) difficult and lengthened inhalation; d) difficult and lengthened exhalation; e) the difficult inhaling and exhaling. 40. Describe the breathing during the expiratory dyspnea: a) constant amplitude; b) superficial; c) difficult and lengthened inhalation; + d) difficult and lengthened exhalation; e) difficult inhalation and exhalation.