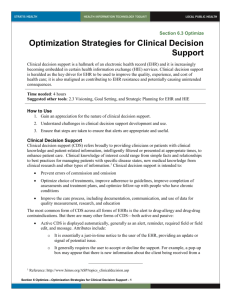
6 Optimization Strategies for Clinical Decision Support
advertisement

Section 6.2 Optimize Optimization Strategies for Clinical Decision Support Clinical decision support (CDS) is a hallmark of an electronic health record (EHR) and it is increasingly becoming embedded in certain health information exchange (HIE) services. Clinical decision support is heralded as the key driver for EHR to be used to improve the quality and cost of health care; it is also maligned as contributing to EHR resistance and potentially causing unintended consequences. As such, it is very important to thoroughly plan for clinical decision support, keep the software current, and take steps to ensure alerts are appropriate, useful, and used within the context of clinical judgment. Time needed: 30 – 40 hours Suggested other tools: Section 4.6 Workflow and Process Improvement for EHR and HIE How to Use 1. Gain an appreciation for the nature of clinical decision support. 2. Understand challenges in clinical decision support development and use. 3. Ensure that steps are taken to ensure that alerts are appropriate and useful. Clinical Decision Support Clinical decision support (CDS) refers broadly to providing clinicians or patients with clinical knowledge and patient-related information, intelligently filtered or presented at appropriate times, to enhance patient care. Clinical knowledge of interest could range from simple facts and relationships to best practices for managing patients with specific disease states, new medical knowledge from clinical research and other types of information.1 Clinical decision support is intended to: Prevent errors of commission and omission Optimize choice of treatments, improve adherence to guidelines, improve completion of assessments and treatment plans, and optimize follow-up with persons who have chronic conditions Improve the care process, including documentation, communication, and use of data for quality measurement, research, and education The most common form of CDS across all forms of EHRs is the alert to drug-allergy and drug-drug contraindications. But there are many other forms of CDS—both active and passive. Active CDS is displayed automatically, generally as an alert, reminder, required field or field edit, and message. Attributes include: o It is essentially a just-in-time notice to the user of the EHR, providing an update or signal of a potential issue. 1 Reference: http://www.himss.org/ASP/topics_clinicaldecision.asp Section 6 Optimize—Optimization Strategies for Clinical Decision Support - 1 o It generally requires the user to accept or decline the support. For example, a pop-up box may appear that there is new information about the client being received from a health information exchange organization (HIO), such as an update to a medication list or reminder that a lab test is due. This may only need to be clicked off to populate the EHR. The decision whether to view the information as it is coming in should be the user’s choice. Another example may be that an assessment has been initiated, but there are certain highlighted fields that still need data to be entered. The user can complete the entries or ignore them until a later date. o It must be important and relevant, or it will be ignored (i.e., declined without consideration as to whether it is important or not). This is often referred to as “alert fatigue” and is generally a consequence of poor design and lack of stakeholder input into the clinical decision support system. For example, if every time a common drug, such as acetaminophen, is ordered or prepared for administration there is an alert that it could have an adverse effect on the liver, the alert will be considered an annoyance by most users. However, if a client was already taking a specific drug being considered, an alert about this would be well-received by users. The greater the complexity or integration of information, the more intrusiveness is accepted by the user. Passive CDS is displayed on user request. Examples include a user setting a preference for what information is displayed on a client dashboard, whether certain information will be presented in table or graphic format, or that the user can have access to additional information (e.g., training materials for client, drug information) upon request. Forms of CDS in Behavioral Health EHRs In addition to alerts concerning drugs delivered by e-prescribing systems or components of EHRs, the following forms of CDS are found in behavioral health EHRs: Assessment completion. One of the most common forms of CDS directs completion of the assessment. In its simplest form, this consists of reminders to complete empty data fields. It is especially useful for assessments that must be completed over a period of time. This form of CDS may also utilize more sophisticated branching logic to direct the user to various parts of an assessment, based on the client’s needs. Workflow notification directs users to perform certain tasks. For example, if a treatment plan requires review, this type of CDS can notify the user of an approaching deadline. Documentation that requires co-signature can be directed to the appropriate individual for action. Adding hyperlinks to documents in a document repository is another potential workflow support tool. Diagnostic assistance. Although there are competing schools of thought in behavioral health care about whether to focus on accurate diagnosis or objectively measured functional changes, both can benefit from CDS. For diagnostic support, the Structured Clinical Interview for Depression (SCID) can aid in arriving at a correct differential diagnosis. This assessment takes considerable time and is often limited to research settings. Another tool, a Web-based diagnosis checklist system called Isabel, is used to differentiate between a drug contraindication and a clinical diagnosis. This requires the collection of information that is typically outside the domain of behavioral health, but it may be helpful in evaluating drug therapies. Functional assessments—such as the Daily Living Assessment (DLA), Child & Adolescent [or Adult] Needs and Strengths Assessment (CANS/ANSA), and others—help improve objectivity in considering functional deficits that direct treatment. Section 6 Optimize—Optimization Strategies for Clinical Decision Support - 2 Therapy critiquing and planning software operates much like drug knowledge databases in supplying alerts and reminders about potential drug allergies or contraindications. Instead of drug information, these systems integrate clinical research, practice-based evidence, client preferences, and the choices being considered by the user to generate recommendations specific to the client’s needs. The knowledge database is a subscription service that is constantly updated with new findings. Client preferences may be derived from the client’s personal health record and/or from a client interview. For example, you may want to suggest some computer games to an adolescent client that would help direct the client to new behaviors. The software can tell you which games have recently proven helpful, which seem to have fallen out of favor, and new games that have been created. However, you may also wish to consider how much time the client spends on the computer before recommending any game. With this information—which could come from the client’s diary of computer use or from an estimate made during an assessment—the CDS may offer some alternative suggestions. Functional Magnetic Resonance Imaging (fMRI) is technology in its infancy, but it could help interpret clinical images, leading to quicker or improved evaluation of a client’s risk for a specific diagnosis or functional deficit, such as Alzheimer’s disease (see http://www.scirp.org/journal/PaperInformation.aspx?PaperID=39946). The technology could also help assess progression of conditions and track therapeutic effectiveness. It is imperative that any form of CDS be reviewed by the intended user, be from a trustworthy and reputable source, and be used only to supplant—not replace—professional judgment. Planning for Clinical Decision Support Take the following steps to make sure that the CDS supplied through your facility’s EHR and HIE is appropriate and useful: Engage stakeholders (those who will be using the system directly as well as those who use reports to measure outcomes) in: o Understanding their role in planning for CDS use o Establishing goals for use of CDS o Expressing concerns about CDS Translate goals with respect to CDS: o Describe actions users are expected to take when receiving an alert. o Obtain baseline performance data that demonstrates why the alert is necessary (or why an alert may not be necessary and could be turned off). o Anticipate desired outcomes by setting realistic quality and patient safety goals. o Annotate rationale and potential obstacles so all stakeholders are aware and can sign off on the approach to adopting CDS. Ensure EHR (and HIE, if applicable): o Is compliant with interoperability standards (technical, semantic, and process) to reduce errors in alert presentation. o Supports sensitivity setting (some EHRs support different levels of alerting depending on the user role). Section 6 Optimize—Optimization Strategies for Clinical Decision Support - 3 o Have CDS rules that are compatible with practice guidelines, protocols, and other evidence-based knowledge that is periodically refreshed as new knowledge becomes available. Many EHRs include a subscription to a drug knowledge database that may be refreshed monthly or quarterly. Code sets need to be refreshed annually and changes in best practice recommendations should be able to be pushed to the system when applicable. o Is compliant with regulations for both the Centers for Medicare & Medicaid Services and state requirements. Identify, select, or build CDS interventions needed to achieve goals at various point in clinical workflow. Stakeholders who are being asked to use clinical decision support must have a say in the system that will be used. Some behavioral health EHRs support facility development or extensive modification of many different forms of assessments. While this may seem like a good thing, evidence suggests that too much customization adds cost, reduces outcomes comparability, and puts a facility at risk either financially (for not collecting required data) or clinically (for not following evidence-based guidance). See: Thinking Customization? Proceed with Caution, available at: http://www.behavioral.net/print/article/thinking-customization-proceed-caution). Require stakeholder review, test, validation, and approval for all CDS support systems, changes made to these systems, and revision/update maintenance. It should be obvious that the acetaminophen example described above contributes to alert fatigue. But turning that rule off should be a stakeholder decision. Pros and cons should be weighed as any such decision is made. Consider both the probability and nature of harm that could occur, as well as the likelihood that retaining such alerts could mean that important alerts are ignored. Train users and monitor use. Ignoring alerts is commonplace and can be monitored through an audit logging process (if available in the EHR). However, misinterpreting an alert or making an erroneous selection are actions relative to alerts that are more difficult to identify and may require a manual audit. Measure results, evaluate effectiveness, and refine CDS support program. Users who are provided feedback on the results of using CDS are more apt to use it appropriately. For example, the fact that 92 percent of assessments were completed on time, compared to 73 percent without the EHR and its CDS, is strong evidence of value. Factors for Appropriate/Useful Alerts Use the checklist below to help stakeholders identify, select, or build CDS. For most behavioral health EHRs and HIE services, stakeholders will primarily be identifying and selecting, rather than building, CDS. Not all of these attributes may be available through your behavioral health EHR or HIO, but you can have your vendors consider adding them over time. Clinical decision support should be: Specific to client Relevant and important Accurate Clear and unambiguous Show justification for use Concise Section 6 Optimize—Optimization Strategies for Clinical Decision Support - 4 Provide alternative actions Make additional information accessible, if applicable Generated for all dangerous cases Directed to the right user Knowledge/credential-specific Tied to previous performance of user to avoid repetition of alerts Designed to make it difficult to overriding a “fatal” or “critical” alert Built to require a reason for overriding the alert (at least through a simple drop-down menu) Delivered to promote action rather than stop intended action Easy to see and use, not obstructing the primary view of the underlying information and not requiring multiple clicks, scrolling, page visits, or narrative typing Using CDS with the Client There is some evidence that suggests that CDS can be a turnoff for patients. One study reported that patient attitudes vary—and that patients whose providers have more positive attitudes about EHRs and patients who have a high locus of control about their own health care situation were more supportive of CDS aids. As a result, the authors recommend finding ways to educate clients about the value of CDS. These might include: Learning how best to use the EHR at the point of care—with respect to positioning, communicating with the client during data entry, using the EHR to validate the accuracy and completeness of data being collected, and providing information to the client via the EHR. Explain to the client why evidence in making decisions is important and how it supports upto-date treatment regimens. Adopting a client self-management model of care in which the EHR is a tool to support shared decision making. Copyright © 2014 Stratis Health. Section 6 Optimize—Optimization Strategies for Clinical Decision Support - 5 Updated 03-18-14