Early Warning Scores have lower accuracy when predicting
advertisement
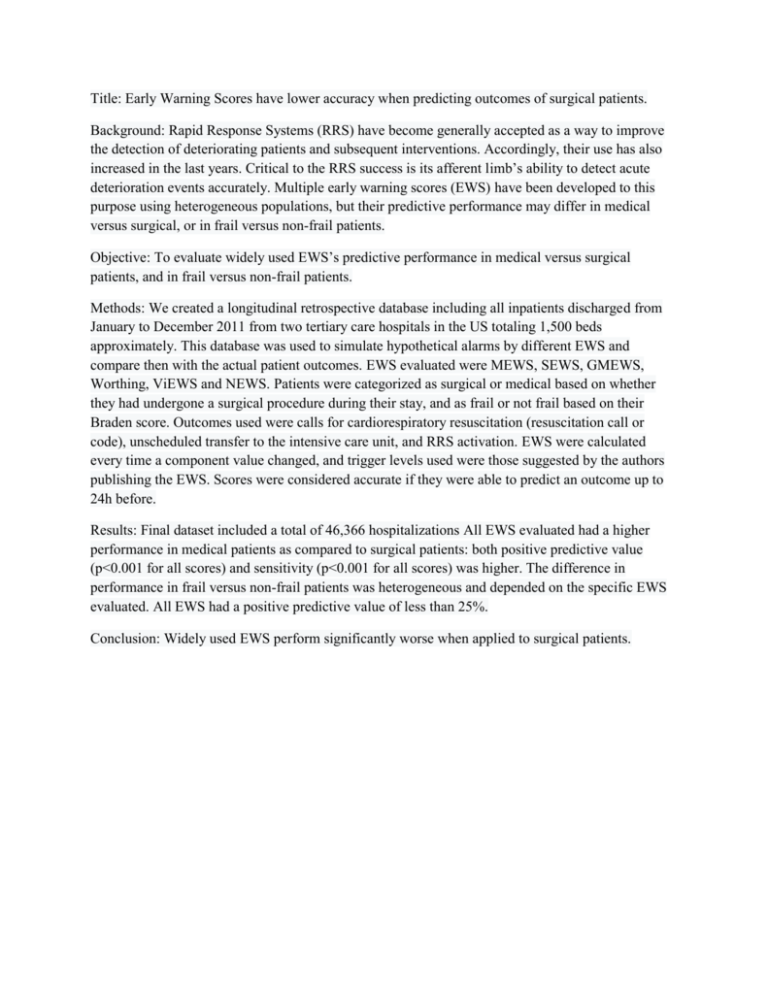
Title: Early Warning Scores have lower accuracy when predicting outcomes of surgical patients. Background: Rapid Response Systems (RRS) have become generally accepted as a way to improve the detection of deteriorating patients and subsequent interventions. Accordingly, their use has also increased in the last years. Critical to the RRS success is its afferent limb’s ability to detect acute deterioration events accurately. Multiple early warning scores (EWS) have been developed to this purpose using heterogeneous populations, but their predictive performance may differ in medical versus surgical, or in frail versus non-frail patients. Objective: To evaluate widely used EWS’s predictive performance in medical versus surgical patients, and in frail versus non-frail patients. Methods: We created a longitudinal retrospective database including all inpatients discharged from January to December 2011 from two tertiary care hospitals in the US totaling 1,500 beds approximately. This database was used to simulate hypothetical alarms by different EWS and compare then with the actual patient outcomes. EWS evaluated were MEWS, SEWS, GMEWS, Worthing, ViEWS and NEWS. Patients were categorized as surgical or medical based on whether they had undergone a surgical procedure during their stay, and as frail or not frail based on their Braden score. Outcomes used were calls for cardiorespiratory resuscitation (resuscitation call or code), unscheduled transfer to the intensive care unit, and RRS activation. EWS were calculated every time a component value changed, and trigger levels used were those suggested by the authors publishing the EWS. Scores were considered accurate if they were able to predict an outcome up to 24h before. Results: Final dataset included a total of 46,366 hospitalizations All EWS evaluated had a higher performance in medical patients as compared to surgical patients: both positive predictive value (p<0.001 for all scores) and sensitivity (p<0.001 for all scores) was higher. The difference in performance in frail versus non-frail patients was heterogeneous and depended on the specific EWS evaluated. All EWS had a positive predictive value of less than 25%. Conclusion: Widely used EWS perform significantly worse when applied to surgical patients.