Final Med Exam Hints
advertisement

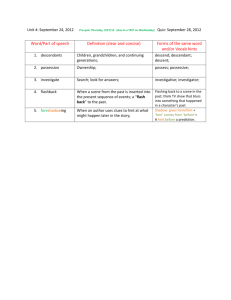
5th Med Final Exam Hints: Medicine: Short Cases: Categories: - Cardiovascular Respiratory Neuro MSK – connective tissue Endocrine CVS: Likely case: Murmur - Dx: Mitral regurgitation or aortic stenosis (B. Creeden prefers A.S) Possible valve replacement (always a left sided valve) Will be asked to auscultate pt’s praecordium o Hint: Quickly check for saphenous scars – sternotomy scar likely for valve replacement if scar not visible. o Ensure to feel for/find apex beat – shows where heart is! o See excess bruising while auscultating – valve replacement (warfarin levels = 3-4) o Can’t hurt to take pulse while auscultating Respiratory: Likely case: Crackles: - Dx: Fibrosis. o Will be soft/subtle but audible o Ask pt to cough. If cleared by coughing, NOT fibrosis o Unlikely to hear apical, likely bibasal or unibasal – fibrosing alveolitis o Hint: keep eyes open while auscultating to perform inspection for signs pointing to fibrosis eg: scleroderma, rheumatoid disease, clubbing Neuro: Hint: May be asked to look at patient and spot diagnose appropriate test you would perform. Likely case: CN Palsy: - Usually involves o ocular muscles o facial nerve palsy o fields of view (rare) Likely Case: Diabetic Foot: - Test vibration, temp, sensation, proprioception Probably no ulcer Not very suitable for short case (has happened) but better for long case as patient pedal hygiene and student hand washing separate issues. Likely Case: Parkinson’s: If patient is sitting in a chair with shoes on, they are likely prepared to be asked to walk. Not so much if in bed. - - Examination: GET PATIENT TO WALK TO ILLUSTRATE BRADYKINESIA, SHUFFLING GAIT, COGWHEEL RIGIDITY Tone o Expect hypertonia o Do bilaterally as Parkinson’s can present unilaterally o Reinforce maneuver makes tone become jerky Brisk reflexes Glabellar tap: Parkinson’s patient will continue to blink. Not specific test for Parkinson’s Likely Case: Stroke: - Probably pt with a very mild stroke exhibiting mild hemiparesis Muskuloskeletal/Connective Tissue Disease: Likely Case: Rash - High probability of being psoriasis; psoriasis is a stable rash. Ethically difficult to maintain a good clinical rash of cellulitis! Psoriasis pits nails and affects extensor surfaces. Psoriasis can mimic RA so check the nails and extensor surfaces carefully. Possible case: Discoid Possible Case: Myotonic Dystrophy - Balding Ptosis (eyelid infringes on pupil) Permanently corrugated forehead Likely Case: Rheumatoid Arthritis: - - If told patient has RA (Dr. Phelen often does this), job of short case is to determine whether active or not (red, hot, tender, swollen). Listen to the question being posed!!! Hint: Observe as much as possible without touching as patient may be in real pain. Be prepared to introduce self WITHOUT shaking hand. Ask pt to place hands on pillow, observe joints. Ask patient to put backs of hands to opposite cheeks to check extensor surfaces for tophi. Hint: brush hair back to check backs of ears for tophi! Palpation, always looking at pt for signs of tenderness: o Temp first o 4 point (index finger and thumb of both hands) over all joints, especially DIP and nails (tenderness and subluxation) o Hint: DIPs spared in RA, involved in psoriatic arthritis (psoriatic arthropathy). Sometimes only distinguishing feature o 6 point examination for wrists (tenderness and subluxation). Functionality Testing: use discrimination based on pt. current state o Write with pen? o Unbutton shirt –small buttons different level than large buttons o Pick up cup o Pass cup between hands o Cup with straw – probably can’t pick it up so ask to push it side to side. Give summary: Condition involves X joints, which are warm and tender to touch. Also has X present. Based on these findings this would be X (R.A.; psoriatic arthritis) which is/is not currently active. Likely case: Scleroderma: - - Observe: o Pinching of skin around nose, mouth, eyes o Sclerodactyly o Examine: Hands: CReST o C = calcinosis o Re = Reynaud’s (do not elicit as is painful condition! It’s there or it isn’t) o S = Sclerodactyly o T = Telangiectasia – usually in mouth though rarely found on chest Ask: Difficulty with swallowing? o Implies esophageal involvement – poorer prognosis Endocrine Acromegaly Thyroid (Graves’) – especially in SIVUH - If it is a thyroid exam, examiner will want to know 1 to 3 things: o Is thyroid involved? o What is thyroid status? - o Are eye signs present? Establish suspicion of Grave’s with examiner via observation of goiter? Ex-opthalmos? Next step is to determine status (active or not): Examination: o Pt to stick out tongue while looking at neck to r/o thyroglossal cyst o Diaphoresis o Pulse – will be tachy at rest o HPO of wrist o Acropatchy of fingertips o Establish fine tremor – place piece of paper on outstretched hands o Pre-tibial myxoedema – indicates hyperthyroid states o Reflexes – hyper in hyper, hung in hypo o Eye signs: Look for white of cornea between upper rim of pupil and eye lid Look from side, eye angle should normally be 30-40o? (Use hand to be dramatic about it) Look from above to see if protruding? Test lid lag Surgery Gastrointestinal: Likely case: Abdominal pain: If patient is jaundiced and asked to examine abdomen, begin with hands and arms. - - Palmar erythema and spider naevi – indicate chronic disease o Unlikely to palpate liver edge o If liver palpable, expect hard, craggy edge Hint: o Tender hepatomegaly: acute scenario o Non-tender hepatomegaly: chronic scenario Vascular: If FULTON is the examiner, likely topic: EVAR Question 1: What do you need to ensure is present for EVAR? - Strong femoral pulses bilaterally because that is the method of access. Question 2: What else do you need to know prior to EVAR? - Renal function. EVAR utilizes high doses of contrast medium which is cleared by the kidney. Impaired renal function in the presence of these volumes of contrast can result in contrast nephropathy. OBSTETRICS: Likely patients: - Small for dates (LMP very important here – dating accuracy) Diabetes Twins – in for a rest HTN (social hx: would BP be lower if home with family?) After ½ hour examiners will appear: Have patient sitting on 2 pillows for presentation Ten steps to 1H. Do in this order to keep examiners listening and you talking as little about obstetrics as possible!: 1. Introduce patient to examiners a. (eg: Examiner X and Examiner Y, I’d like you to meet Mary Murphy from Glasheen Rd.) 2. Reason for Admission: a. Eg: Mary Murphy is in for PPH following birth 2 weeks ago 3. Past medical and past surgical history 4. Past Obstetric History (KISS philosophy if normal) a. Know children’s names and ages b. Know heaviest weight at birth c. Confirm facts with patient: “isn’t that right Mrs. Murphy?” 5. Menstrual History a. On OCP? Bleed may have occurred as chemical withdrawal bleed from pill otherwise: b. Phrase along these lines: i. Not on pill ii. Her cycle is X days of which she bleeds X days iii. She is sure of her dates iv. Has had a scan in early pregnancy which concurred with her dates 6. Family History a. Always include a comment on these 5 (stating relevant negatives buys time): i. Diabetes? ii. iii. iv. v. HTN? Congenital Abnormalities Rheumatic Fever Multiple Pregnancies 7. Social History – make it about the family! a. Who minds the kids/siblings in her absence? b. Domestic situation i. If sensitive, “I would like to discuss afterwards.” c. What does the family do? i. Daughter in ballet? ii. Son playing hurling or football? iii. This gives a sense that you’ve got to know the patient a bit beyond her current situation d. Smoke/drink/etc… 8. Events of Pregnancy – do this late in the presentation so you don’t say something that has you talking the entire time about technical obstetrics and forget about the patient! a. Describe hx of pregnancy i. Booked on… ii. Scan on… agreed with dates iii. Had normal pregnancy until… b. Time to ‘guild the lily’: Ask the examiner a question about the patient they likely won’t know but is relevant to pt iii. (Did you happen to see the results of…?) i. Eg: normal until flank pains. Ask for result of msu query infection? ii. Normal until blood pv: what was blood group? Hb? iii. Normal until rash: what is rubella status? c. This is a bit of a distraction to both you and examiner, snaps them back from a day dream, and shows you were thinking beyond getting and presenting a good history. 9. On Examination: a. Mrs Murphy looks well/fatigued/pale/content/bored… b. CVS/Resp systems first: i. NB: mention haematinic murmur of pregnancy/reproduction if pregnant. All pregnant women have it! c. Of Abdomen: IPPA approach: i. Caution of pitfall: 1. Cephalic presentation? 2. Engaged/not engaged? ii. Make certain of presentation otherwise say unsure. Honesty makes fewer mistakes than guesses. iii. Auscultation: Can say you heard heart over the back on the L. side. If can’t find it again, fetus moved (which they should do all the time). iv. Look at feet/ankles. No matter how neatly the bed is made up by the nurses, rip up the end of the bed to look at the feet for: 1. oedema (and medial tibia) 2. varicose veins. Do not pull covers down from patient’s waist. Not a slick move! 10. In summary and Management