Antituberculin, Antivirals, Cancer
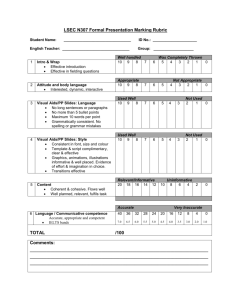
advertisement

Principles of Drug Action Antituberculin, Antivirals, Cancer Antituberculin Tuberculosis Caused by Mycobacterium tuberculosis Thought be eradicated ~1960, but wasn’t being treated properly & AIDS Problems Slow-growing Treated chronically `6-18 months but patients are noncompliant Side effects become prominent, possible drug toxicity Development of resistance – must use combination therapy HIV/AIDS patients Mycobacterium avium complex (MAC) includes M. avium, M. intercellulare – disseminated (throughout body?) infection Mt - normally pulmonary 1st Line Isoniazid (INH) A - well absorbed po, IM D - extensively distributed, inc. CSF Tx intracellular and extracellular org Inhibits biosynthesis of mycolic acid (unique to mycobacteria for construction of cell wall) M - acetylationinactive (bimodal – slow and rapid acetylators) INH hydrolysishydrazine (toxic), AcetylhydrolyzedacetylhydrazineHepTox <20, 0% HepTox >50, higher incidence of HepTox Main AE – NeuroTox: peripheral neuritis, muscle twitches, convulsion prevented by adm. of B6 (pyridoxine) – competive inhibitor Rifamycin Rifampin – an antibiotic inhibits DNA-dependent RNA polymerase also tx G+, G-, carrier formof N. meningitides (normal form DOCPen G) A - po, D- inc. CSF, E – bile, potent Phase I/II inducer (microsomal enzymes) Brightly colored, red-orange, colors body fluids (sweating blood) AE – thrombocytopenia, GIU Rifapentine – same as rifampin, but longer half-life Rifampin qd, Rifapentine - 2q week Ethambutol Interferes with arabinose glycan (component of cell wall) specific for mycobacteria A – po, D-widely, M- alcohol (non-P450)carboyxlic acid, AE – optical neuritis (↓visual acuity) – get baseline optical exam Pyrazinamide Unclear MOA, might be prodrug? M – hydrolyzed to pyrazinoic acid (active) AE – HepTox, hyperuricemia 1st Line for MAC Clarithromycin + Ethambutol Rifabutin (also rifamycin) Recommended w/ clarithromycin + ethambutol (nFDA) Azithromycin may be used in place of Clarithromycin Prophylaxis – Clarithromycin, Azithromycin, or Rifabutin (FDA) Duration?- indefinite 2nd Line (used with allergic reactions, unacceptable side effects) Aminoglycosides Streptomycin (used to be 1st, but must be given parenterally) only active against extracellular organisms Kanamycin Amikacin very polarIV, nephro, otoTox tx Gram -, mycobacterium, Gram + (?) Fluorinated Quinolones Moxifloxacin Ciprofloxacin Paraaminosalicylic acid (PASA) – antimetabolite of PABA Cycloserine Capreomycin Therapeutics Mycobacterium Tuberculosis, Fansasie, Leprosy Predisposed – Homeless, Smokers, drug users, HIV/AIDS Also Mycobacterium Avian Complex (MAC) in immunocompromised, HIV/AIDS, Transplant, Chemotherpay patients First Line Rifampin(HepTox), Isonizazid(SLE), Pyrazinamide, Ethambutol, Streptomycin(or 2nd?) 95-98% treated with Rifampin and Isoniazid over 9 months Adding Pyrazinamide reduces DOT 6 months If ResistantPyrazinamid and Ethambutol added Post-exposure prophylaxis – Ciprofloxacin/Levofloxacin 14 days Prophylaxis in Immunocompromised – Azitromycin Malaria Chloroquin (Plaquenil) PCP Bactrim Leprosy also mycobacterial – Mycobacterium Leprae (even slower growing, > 2years) Dapsone po, ~sulfonamide, tx 2years – life hemolytic anemia by inhibiting Glucose-6-phosphate dehydrogenase G6PH->NADPHreduces glutathione involved in RBC membrane Methemoglobinemia aromatic group metabolizes Fe2(red)Fe3 (blue), doesn’t bind O2 as well can withstand 15% conversion (normally 1%), changed back to nornal hemoglobin with methemoglobin reductase Cyanide poisoning Treat with NaNO2 methemoglobinemia, Fe3+ CN +thiosulfateNa thiosulfate Specific antidote – methylene blue Strong possibility of resistance, never use alone Rifampin + Dapsone +Clofazimine Clofazimine po, binds to guanine nucleotides of M. leprae (specific) antiinflammatory reaction, counters Erythema Nodosum Leprosum (ENL) AE - Red discoloration of skin Thalidomide Immunomodulatory (?) Agent po tx suppress ENL AE – sedation, teratogenic FDA System for Thalidomide Education and Prescribing Safety (STEPS) Program Antivirals Hepatitis A – spontaneously resolved, no antibiotics required B – reverse transcriptase virus Acute (resolves spontaneously) Chronic – when it doesnt resolve Monotherapy – NRTI or PEG-Interferons Nucleoside reverse transcriptase inhibitors (NRTI) Reverse transcriptase – RNA-dependent DNA polymerase Nucleoside (Base with sugar) nucleotide (base +sugar+phosphate) in vivo Entecavir (Baraclude) po, not Nephrotoxic less likely to provoke resistance Adefovir (Hepsera) prodrug po, NephTox Lamivudine (Epivir) also tx HIV/AIDS, resistance possible, Use if patient undergoing Highly Active Antiretroviral Therapy (HAART) Tenotovir (Viread) nucleotide (base + phosphate) analogue prodrug Telbivudine (Tyzeka) AE Severe acute exacerbation, requiring reinstitution of therapy Lactic Acidosis with Steatosis + Hepatomegaly Possible resistance to HIV meds unless on HAART Interferons – naturally-occurring antiviral proteins Pegylated to improve DOA, given once a week, sq, ~ug Peg interferon alfa 2a (Pegasys) Peg interferon alfa 2b (PEG-Intron) Serious Psychiatric side Effects C Acute:tx Pegylated interferons for 6 -24 weeks If viral RNA not cleared after 3 monthschronic tx Ribovirin (Copegus/Rebatol) Nucleoside analogue, azole – Interferes with viral RNA Replication Metabolized by deribosylation and amide hydrolysis (not P450) AE – teratogenic, 120hr t1/2, direct hemolytic anemiacardiac Avoid in CVD, may MI Newer Tx – Protease Inhibitors Hep C has vDNApolyproteins (protease) fxnl proteins maturation/replication Telaprevir (Incivek) – 750mg q7-9hrs po, P450 + inhibitor Begin tx w/ PEG-Inteferon + Ribovirin AE – skin rash, pleuritis, Ha Boseprevir (Viktrelis) – 800mg q7-9hrs po, met aldoketoreductase, P450+ inhibitor Begin after 4 weeks PEG-I and Ribovirin AE – fatigue, N, Ha HIV/AIDS 1987 – Zidovudine (NRTI) Now 26 drugs – 8 NRTI (1 nucleotide), 5 NNRTI, 10 Protease inhibitors, 1 fusion inhibitor, 1 entry inhibitor, 1 integrase inhibitor Combination therapy most effective, 6 different ones NRTI – Nucleoside (1 Nucleotide) Reverse Transcriptase Inhibitors po qd, -sine –dine, -bine All must be converted to triphosphate form before working Zidovudine (Retrovir) Met→ glucuronidation on ribose-hydroxyl groups AE – Granulocytopenia Abacavir (Ziagen) M - not p450, but by alcohol dehydrogenasecarboxyl acid + glucuronidation heavy drinkingethanol will compete w/ abacovir↑ Abacavir AE – severe hypersensitivity (5%) – don’t challenge it Tenofovir (Viread) nucleotide, tx resistant strains of HIV qd Emtricitadine (Entriva) Least toxic Didanosine purine, metxanthine oxidase, inhabitied by allopurinol Lamivudine (Epivir) Commonly used with other drugs in combinations Stavudine NNRTI – Non-nucleotide Reverse Transcriptase Inhibitors, “-vir-“ Non-competitive inhibitors of the enzyme Used with NRTIS synergistically “-vir-“ but not Enfurvirtide and Maraviroc – entry inhibitors po M – by P450, Nevirapine + Etravirine can induce its N+E – insomnia, hallucinations, psychosis Nevirapine (Viramune) Etravirine (Intelence) Delavirdine ~ not used Efavirenz (Sustiva) Rilpirivine-sedation AE – Skin rash, Steven-Johnson syndrome (more common with N+E) Protease Inhibitors – -vir except Abacavir(NRTI), Tenovir (NRTI), Raltegravir (Integrase inhibitor) M – P450 to different extents + inhibit +induce (except Atazanavir (Reyataz)) Ritonavir –used with other protease inhibitors to block their metabolism Lopinavir(only with Ritonavir) - Lopinavir + Ritonavir (Kaletra) Saguinavir (Fortivase?) least potent inhibitor AE – Diarrhea (exc Indinavir (Crixivan)skin rash) po, should be taken with food (exc Indinavir w/ empty stomach) Atazanavir (Reyataz) – requires acidic medium to absorb Ritonavir Ritonavir/Lopinavir (Kaletra) Indinavir (Norvir) Amprenavir formulated w/ Vitamin E and PEG to enhance absorption taken with meal (but not high fat) Fosamphenavir – phosphate ester, no PEG, no worry about meals Tirpranavir (Aptiva) Must be Adm/ Ritonavir HepTox, intereferes with plateltsintercranial bleeding, bid Fusion inhibitor Prevents fusion of virus with cell preventing entry Enfurvirdide (Fuzion) binds to protein on virus (GP-41) Synthetic 36 amino acid peptide very expensive sq, only sq AIDS drug not metabolized by p450, but proteolysis AE – injection site reactions (Erythema, induration pain) Entry inhibitor Prevents virus from entering cell after fusion Maraviroc (Selzentry) binds to a chemokine (CCRI) receptor on host cell more so to CCR5 (tropism), test to see if CCR5 present A-po, M-P450* AE – Cough, URI, allergy, HepTox Integrase inhibitor Inhibits integration of viral DNA into host DNA Raltegravir (Isentress) po M - not P450 but glucuronidation enhanced by Rifampin and Rifabutin Highly Active AntiRetroviral Therapy (HAART) Reduces viral load allowing immune system to recover Opportunistic Infection Treatment Pneumocystic jiroveci pneumonia – Bactrim Bactrim, Septra Pentamidine Inhaler – prevention once a month, not DOC MAC/Tuberculosis Rifabutin (MAC), Rifampin (TB) – but nFDA Both induce hepatic microsomal enzymes Toxoplasmosis (Toxoplasma gondii) Pyrimethamine + Sulfadiazine – sequential blockade of folate metabolism in fungus Pyrimethamine – inhibits DHFA reductase Sulfadiazine – inhibits incorporation of PABA into DHFA Folinic acid (Leucoverin) – antagonist to inhibition of DHFA reductase reversing toxicity in humans (can only be taken up by active transport in humans) Cytomegalovirus (CMV) retinitis Ganciclovir – purine analog Foscarnet – phosphoric acid derivative Cidovir – pyrimidine analog Complicated dosing regimen, at first IV, then injected into eye topically Cryptococcus neoformans Cryptococcosis Cryptococcus meningitis Tx Amphotericin B + Flucytosine o/ Fluconazole Candidiasis Kaposis Sarcoma – slow-growing cancer Immune System Recovery Inflammatory Syndrome (IRIS) After HAART, when immune system begins to recover, it responds to previously acquired opportunistic infections (indolent or residual) Reacts with overwhelming inflammatory response Tx Corticosteroids, NSAIDS Antiretrovirals with Sulfamido Group (RSO2NHR) ~ Cross-reactivity with other sulfamides diuretics, sulfa antibiotics, Viagra, Ibutilide(Covert), Dofetilide, Anprenavir (Agrenase), Delavirdine, Famovudine, Darunavir(Prezista), Tipranovir (Aptivus), HIV/AIDS Therapeutics 2 Strains (HIV-1, HIV-2) – treated the same, in US, HIV-1 is predominant May present Sx differently Risk Factors Unprotected/Unsafe Sex Sharing Needles Any exchange of infected fluid Infected Blood (been tested since 1985 in US), Organ eg Ryan White, hemophiliac who got HIV from clotting factorsdiedmoney for AIDS Part A– Money to clinics to manage AIDS, for physicians, nurses, etc. Part B– AIDS Drug Assistance Program (ADAP), set up through health department Part C– Research Part D– AIDS education training(health care providers) centers Neonatal Transmission Progression of Disease Determinants of Effectiveness/Monitoring Parameters CD4 (protein receptor found primarily on T4 helper cells), normal=1000 Opportunistic infections, when CD4<350 HIV RNA/ Viral Load (controlled HIV/AIDS – 48,000) 1st 72 hours Can treat prophylactically (100% effective) Acute HIV Infection - 30-50% of newly infected have symptoms in first week very general Sx – diarrhea, fever, swollen lymph nodes, ~etc 1st 3 months, Viral load increases, CD4 count decreases ~ 3 months antibody production (For 90% of people) Can test for HIV/AIDS now by looking for antibodies w/ ELISA (main screening) Western Blot – more accurate test Up to 20 years – Dormant period Dormant period ends AIDS CD4 <350AIDSOpportunistic infections, cancers ~200 Fungal infections ~ Candidiasis, PCP ~ 50 MAC Therapy Can increase CD4 by 100-150 cells/yr Drug pressure on virusvirus mutate Must use drugs every day to prevent resistant, Adherence must > 95% May Genotype the patient if Viral Load >1000 to determine drug resistance For Naïve patient (with no drugs before) Use 3 drugs 2 from NRTI class (NRTI=Backbone Class) in combination Zidovudine + Lamivudine (Combivir) Tenofovir + Emtricitadine (Truvada) Abacavir + Lamivudine (Epzicom) 3rd drug – Choose one from other class) NNRTI – Efavirenz (Susteva), Neirapine (Viramune) popular Tenofovir + Emtricitiadine + Efavirenz (Atripla), qd PI – eg Ritonavir (Kaletra) SI - Raltegrovir (Isenstress) only one Leave a couple classes untouched at first Monitor CD4, viral load every 3 months Viral load should change log 10 If not completely controlled after 3-6 months, change therapy Only use <3 for prophylaxis With low compliance/experienced patients Don’t re-genotype – presence of wild virus + mutated virus genotype not reliable Main Dis with PIs and NNRTIs Cancer Mechanism Oncongenes - cause rapid growth Tumor suppressor genes/TNF – suppress oncogenes Anticancer agents Cytotoxic Cancer drugs grow fast need more supply, take up more drugs But lack specificitySmall TI → toxic side effects Often drugs dosed in mg/m2 (BSA) Adverse Effects Severe NV - Promote release of 5HT tx Prochlorperazine(Compazine), Dronabinol (Marinol) – active ingredient in THC, po Nabilone (Cesnet) – analog of THC, po Metoclopramide (Reglan) – D2 antagonist↑AcH↑GI motility 5HT3 blockers “-setron” work locally in GI Tract and Centrally in CTZ, po and IV Ondansetron (Zofran) – po, IV Granisetron (Kytril) – po, IV Dolasetron (Azimet) - IV Palosetron (Aloxi) – IV Apepitant (Emend) Neurokinin-1 Receptor Inhibitor in CNS, po Fosaprepitant (Emend for injection) IV, 1 hr before chemotherapy, daily for 2 days after Myelosuppession Hemorrhaging, Infection Filigastrin – stimulates neutrophil production Epoetin – recombinant erythropeoitin, stimulates RBC Emetogenic Chemotherapy Destroy cellsexcess DNA/RNApurinesuric acidhyper uricemia Xanthine Oxiase inhibitors (po) Allopurinol (competitive) Febuxostat (Uloric) – noncompetitive Immunosuppression →Opportunistic infections PCP – Bactrim, Septra Serratia Narcesseus – Cephalosporins, Ceftrixaone Alopecia Carcinogenic Teratogenic, esp w/combination chemotherapy (up to 6 diff. drugs) Alkylating Agents Forms covalent bonds w/ DNA and other biomolecules Mustards (Nitrogen) Mustard Gas CLCH2CH2-S-CH2-CH2-Cl Sulfur changed to Nitrogen Liquid and Vesicant, IV Tx Hodgkins, Lymphoma, Leukemia AE – Myelosuppression Cyclophosphamide (Nitrogen mustard prodrug) M- P450 alkylating agent (not vesicant) Tx – multiple myeloma, lymphoma, leukemias, retinoblastoma, neuroblastoma, ovarian, breast cancr AE – Urotoxicity (hemorrhagic cyptitis, hematuria c/o cytotoxic substances in urine) adm /Mesna Mesna (Hs-CH2Ch2-SO2 Na) very polar Restricted to intravascular compartment reduces incidnece of hematuria, hemmorhagic cystitis Mechlorethamine AE - ~Cyclophospamide + MyeloSup Ifosfamide testicular cancer, w/ Mesna Nitrosylureas Lomustine (Ceenu) – po, IV Carmustine (Bicnu) - IV Produces reactive intermediatesreact with DNA D – into CNS tx brain tumors (globlastomasa, astrocytomas) Adm – q 6 weeks AE – MyelTox, NV, Platinum Derivatives A – IV, E – Renal, MOA – Bind covalently to DNA Cisplatin (Platinol) AE - NV(100%), NeuroTox, NephroTox, MyS, OtoTox Adm - Frequently in combo Tx – bladder, testicular, ovarian Carboplatin (Paraplatin) Less toxic than Cisplatin Tx – ovarian, lung Oxaloplatin (Eloxatin) + 5-fluorouracil + Leucovorin for colon cancer AE – persistent NeuroTox (parasthesia) esp. on contact w/ cold Temozolomide (Temodar) Purine-like analog M – hydrolyzed in vivo reactive triazine derivativealkylates DNA A – orally, IV Tx – brain tumors - astrocytomas (resistant to nitrosylureas), glioblastomas AE - MyS Antimetabolites Antifolates Inhibit DHFA reductase Methotrexate A- po, IV, IM, intrathecally D- 50% protein-bound NSAIDS, sulfonamides can displace MTX E – renal excretion (aTS) Compete with same transporter as Pencillins, NSAIDS Probenecid interferes with secretion tx cancer daily, tx Rheumatoid arthritis weekly, narrow TI DOC for Choriocarcinoma 15-30 mg qd, or 1mg/kg qod 75%cure rate Maintenance of remission for acute lymphoblastic lymphoma (ALL) Breast cancer, Epidermoid, Head, Neck, Lung Cancers Osteocaricnoma rescue therapy – lethal dose of methotrexate t/ antidote leucovorin Leucovorin – 5-formylTHFA, antidote to DHFA-reductase blockade dose measured w/ BSA Psoriasis Rheumatoid Arthritis Tox - MyS, HepTox, Diarrhea, Ulcerative Stomatitis (Open Sores in mouth) Pemetrexid (Alinta) MOA – Inhibits DHFA reductase, thymidilate synthetase, also glucinamide ribonuclotide formyl transferase (purine biosynthesis) A – IV infusion w/ Cisplatin Required – Adm/ Low-dose folic acid, B-12 on week preceding + on day of Recomm – Corticosteroid (Dexamethasone 4mg po bid) day of and after Tx malignant pleural mesothelioma, non-small cell lung cancer (NSCLC) AE – NV, Pruritis, Erythema, MyS?, Pyrimidine Analogs Converted to nucleotide (phosphorylation) intracellularly, 5-Fluorouracil M – 5-F deoxyuridine Monophosphate (5F-dUMP) – active form MOA – Inhibits thimydylate synthetase A – IV(cream, solution), topical Tx – GI (gastric, colon, rectal), Breast, Ovarian Head, neck, sqaumous cell carcinoma Topically for premalignant keratoses, basal cell carcinoma ~Systemically Adm w/ Leucovorin AE – MyS, oral sores Cytrarabine (Ara-C) ~Cytosine w/ arabinose instead of ribose Tx IV Acute lymphocytic leukemia (ALL), acute myelocytic leukemia (AML) Copecitabine (Xeloda) Analog of cytidine M(thymidine phosphorylase)5-Fluorouracil Thymidine phosphorylase – higher in tumor cells than in normal cells A- po AE – Hand-Foot syndrome (become irritatednumbness/paresthesia, blister) Diarrhea, MyS Gemcitabine (Gemzan) IV, Analog of Cytidine MOA – Interferes with DNA biosynthesis Tx pancreatic cancer (problem – no problem until major symptomsliver) Also, breast, ovarian Azacitadine (Vidaza) MOA - Incorporated into DNAhypomethylation , prevents protein binding Tx myeloplastic syndrome denovo radiation Sx anemia, leukopeniainfection, thrombocytopeniableeding A – sq, IV Purine Analogs 6-mercaptopurine po, MOA – interferes with DNA synthesis M (xanthine oxidase)→6-mercaptouric acid (inactive) %Competes with Allopurinol for XO Tx Leukemias Pentostatin (Dipent) Tx IV, Hairy Cell Leukemia MOA – Inhibits Adenosine deaminase AE - MyS Plant/Natural Products Antimitotic - Interfere with mitosis by decreasing microtubule function Cell cycle specific for mitosis Vinca Alkaloids From Vinca Rosea (periwinkle plant), large dihydroketo molecules MOA - Bind to α-tubulinprevents formation of microtubule↓cell division Vinlastine, tx choriocarcinoma(MTX-resistant), Hodgkin’s disease AE –MyS Vincristine tx neuroblastoma, Wilms tumor(kidney), ALL AE – neurotoxicity (paresthesias, areflexia, pruritis), ~MyS Vinorelbine – semi-synthetic tx NSCLC, AE-~NeurTox, MyS Taxane Derivatives MOA - Stabilize formation of microtubules, halts mitosis Paclitaxel (Taxol) from Yew tree bark (slow-growing tree) Use precursor in leaves to make it insoluble in water IV Cremophor EL (Castor oil(?)Polyoxyethylated castor oil) possibly allergy to solvent pretreat patient with diphenhydramine, cimetidine/ ranitidine, and corticosteroid Tx ovarian, breast, squamous cell (head and neck), AIDS-related, kaposi’s sarcoma Docetaxel (Taxotere) insoluble in solution, lower incidence of hypersensitivity tx breast, gastric, prostate, NSCLC, squamous cell cancer (head, neck) still need antiinflammatory pretreatment Carboxitaxel (Jevtana) Still need pretreatment, dissolved in polysorbate 80, complex diluting process tx prostate cancer refractory to docetaxel nab-paxitaxel (Abraxane) Paxitaxel attached to nanosized albumin particles (nab), suspension given IV particles – 0.4-0.6 mcm (must be less than 7mcm) suspensions also given IV – propofol(emulsion), amphotericin B (colloid) tx breast cancer no premeds needed for nab Epothilones – from swine bacterium (Sorangium cellulosum)-myxobacterium MOA ~ taxanes Ixabepilone (Exempra) Given in polyoxyethylated castor oilrequires premedication AE – NeurTox, MyS, NV Camptothecins – from Campotheca accuminata MOA – Inhibit topoisomerase I (cuts and ligates DNA strands)prevents from unwinding/relieving torsional stress Topotecan (Hycamptin) – IV, po tx ovarian cancer, nFDA – small cell lung cancer AE – MyS Irinotecan (Camptosar) – only IV M(liver, hydrolysis) SN-38, much more active tx colon + rectal cancer Adm/ 5-FU + leucovorin AE – Diarrhea , MyS early onset D (due to AChE inhibitionChol)ttx atropine late onset D (24hrs after) SN-38 metaboliteexcreted in bile~inflammation severe, life-threatening ttx loperamide + fluids to replenish electrolytes Anthracycline Antibiotics All given IV, all color urine red (in addition to rifamycins, and phenazopyridine) Intercalate with DNA Doxorubicin tx ALL, AML, bone, bladder, wilms tumor, Neuroblastoma, lung, lymphoma CardioTox may be enhanced by cyclosphamide Epirubicin Idarubicin Valrubicin AE – CardioTox(affinity for DNA in tissueEKG abnormality, arrhythmia, CHF resistant to digitalis), MYS Tyrosine Kinase inhibitors Tyrosine Kinase – 1tm cell surface receptor binding site for growth factors (EGF, VEGF, PDGF) activationcellular proliferation in normal cells receptor down regulation mutated cellsget overgrown Tinibs - Small Molecule TKIs MOA - Competitively inhibit tyrosine phosphorylation at ATP site A – po, M ~P450, AE – diarrhea, skin rash, yellowing of skin, (Mys – not major AE) Tx depends on specific GFr and tissue Imatinib (Gleevec) Gefitinib (Iressa) Saratenib (Nexavar) Nitatinib (Tasigna) - prolongs QT interval Sunitinib (Sutent) Lapatinib (Tykerb) Desatinib (Sprycel) Vandetanib (Zactema) Pazopanib (Votrient) – severe HepTox ~Pegaptanib (Mecugen) – pegylated oligonucelotide, VEGF antagonist tx neovascular (wet) macular degeneration (major cause of blindness in US) A – intravitreous inj MOA – reacts with VEGF, preventing VEGF from reacting with TK Large Molecule TKIs Bind to extracellular GF-receptor site A – IV, monoclonal antibodies Bevacizumab (Avastin) – tx Breast, Glioblastoma, Lung Cancer Cetuximab (Erbitux) Trastuzuab (Herceptiv) tx Breast, Gastric Panituumab (Vectibix) tx colorectal cancer