A proposed Task Group of the Unconventional Brachytherapy
advertisement

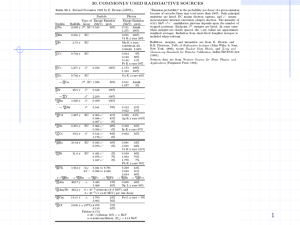
Skin Brachytherapy Task Group Page 1 of 3 April 2013 A proposed Task Group of the Clinical Brachytherapy Working Group of the Brachytherapy Subcommittee Skin Brachytherapy A. Description of the problem, scope of material, and main goals of the Task Group, Brachytherapy to treat skin lesions has a long history, going back to the 1910s. While mostly replaced as a routine treatment modality in the 1940s and 1950s with low-energy x-ray units, and then in the 1970s through the 1990s by electron beams, skin brachytherapy has seen a resurgence recently due, at least in part, to the availability of new applicators and approaches. This task group will review the physical and dosimetric characteristics of available applicators, and suggest treatment and quality management (QM) procedures specific to skin treatments. B. Overview of the rationale for forming the Task Group on this topic relative to timing and content Brachytherapy using solid conical applicators, customized surface molds, and flap-style applicators have been successfully used in the treatment of basal cell carcinoma and squamous cell carcinomas.2 Skin brachytherapy is the preferred technique for patients with small shallow lesions or larger inoperable lesions due to the failure of prior surgeries or other co-morbidities. Several other advantages of skin brachytherapy include good conformality to patient anatomy (e.g. crevices around the ear and nose), as well as the convenience of out-patient clinic services to the patient with clinical outcomes at least as good as surgical results. As noted above, the number of applicators and approaches for skin brachytherapy ha increased markedly over the last decade.3,5 Several vendors offer solid conical applicators for the treatment of shallow tumors (less than 4 mm deep)1,3,4,6 . These applicators have been designed for use with 192Ir or miniature electronic brachytherapy high dose rate sources. Thermoplastic mold style applicators and flap style applicators are most commonly used with 192Ir sources and are generally used to treat larger surface lesions t hat are deeper seated and/or irregularly shaped. Even though treatments with these applicators are generally less cumbersome than external beam-based therapies, numerous challenges exist with the associated commissioning, use, and quality assurance procedures. In example, the choice of the appropriate applicator for each patient requires a considerable amount of medical physics work up and there are no current guidelines available discussing the breadth and standard of care for treatments with these types of applicators. The current practice commonly includes a prescription point 10 mm from the center of the catheter however this arbitrary point needs to be reevaluated from a physics perspective. This report will address the issues described above and facilities wanting to begin a skin brachytherapy program will Skin Brachytherapy Task Group Page 2 of 3 April 2013 find the topics and findings discussed useful for comparing applicator styles and developing QM procedures. C. Description of the Task Group per Task Group definitions This task group is in the category of emerging technology and educational as defined by the Therapy Physics Committee; and the report will include recommendations for quality management, jointly with ESTRO. D. Specific list of well defined charges 1. 2. Review all the commercially available applicators used for skin brachytherapy, including: a. Physical characteristics, b. Safe use and handling c. Dosimetric characteristics. Develop a rational, risk-based set of QM procedures for the applicators and skin brachytherapy procedures, beyond that appropriate for general brachytherapy. E. Brief outline of the report as intended by the proposed chair 1. Brief description of skin brachytherapy and need for the proposed publication. 2. Descriptions of commercially available applicators for skin brachytherapy, including: a. Physical characteristics, including a short description of the various sources used with a given applicator set. b. Handling and use c. Dosimetric characteristics 3. Presentation of a QM program for skin brachytherapy a. Discussion of the methodology for establishing the program b. QM steps for each applicator F. Proposed sunset date December 2016 G. Proposed membership list (Partial) Jose Perez-Calatayud (Co-chair) Regina Fulkerson (Co-chair) Sam Beddar Ravinder Nath Mark Rivard Zoubir Ouhib Sujatha Pai Yi Rong Others to be determined Skin Brachytherapy Task Group Page 3 of 3 April 2013 H. Timeline to monitor acceptable progress 1) 2) 3) 4) Time to first rough draft: December 2013 Time to first draft: December 2014 Time to a nearly final draft. December 2015 Time to a reviewable draft to be submitted to parent committee: July 2016 I. References 1. “Axxent Electronic Brachytherapy System Operator Manual, Appendix J.”, Xoft Inc., 2009. 2. Evans, M., Yassa, M., Podgorsak, E., Roman, T., Schereiner, L., and Souhami, L. 3. 4. 5. 6. 7. “Surface applicators for high dose rate brachytherapy in AIDS-related Kaposi's sarcoma”, Int. J. Radiat. Oncol. Biol. Phys., 39, 769- 774 (1997). Fulkerson, R., “Dosimetric characterization of surface applicators used with high dose rate 192Ir and miniature electronic brachytherapy sources,” PhD thesis, University of Wisconsin-Madison, 2012. Granero, D., Perez-Calatayud, J., Gimeno, J., Ballester, F., Casal, E., Crispin, V., and van der Laarse, R. “Design and evaluation of a HDR skin applicator with flattening filter”, Med. Phys, 35, 495- 503(2008). Ouhib, Z., and Kasper, M., “Clinical Guide to Surface Treatment of Skin Cancer with Brachytherapy”, Nucletron, 2010. Perez-Calatayud, J., Granero, D., Ballester, F., Puchades, V., Casal, E., Soriano, A., and Crispin, V., “A dosimetric study of Leipzig applicators”, Int. J. Radiat. Oncol. Biol. Phys., 62, 579-584 (2005). Rong, Y., and Welsh, J. S., “Surface applicator calibration and commissioning of an electronic brachytherapy system for nonmelanoma skin cancer and treatment,” Med. Phys.,37, 5509-5517 (2012).