Looking Ahead: Practicing Radiation Oncology in the
advertisement
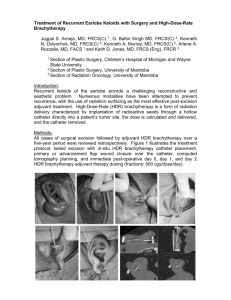
Simulation Training in the Treatment of Gynecological Malignancies with Brachytherapy: A Multi-Disciplinary Program Team: Lisa Singer, MD, PhD1 Steve Braunstein, MD, PhD1 Carly Hoffman, NP1 Tracy Sherertz, MD1 Lee-may Chen, MD2 Adam Cunha, PhD1 Christopher McGuinness, PhD1 1 Department of Radiation Oncology, University of California, San Francisco, San Francisco 2 Department of Obstetrics, Gynecology, and Reproductive Sciences, University of California, San Francisco 1 Overview Brachytherapy plays a crucial, cost-effective role in the treatment of gynecological malignancies1-4. It allows for the precise delivery of a high dose of radiation therapy to the tumor while minimizing dose to surrounding normal tissues. Cervical cancer is the third most common cancer in women world-wide. For locally advanced cervical cancer, when combined with external beam radiation therapy, brachytherapy is considered an irreplaceable standard of care. Despite the importance of brachytherapy, reviews of practice patterns in the United States have identified a decrease in brachytherapy use in clinically appropriate patient populations, with an associated decrease in overall survival with omission of brachytherapy 2,3. Brachytherapy requires technical training and interdisciplinary collaboration and this project aims to address the gap between brachytherapy needs and brachytherapy utilization by developing a novel simulation training (ST) program. ST in the use of brachytherapy for treatment of gynecological malignancies will provide trainees with a comprehensive, longitudinal training opportunity. Few ST programs currently exist in radiation oncology 5 and a review of the literature could not identify current programs in gynecological brachytherapy, representing an opportunity for educational innovation. The multi-disciplinary ST program will involve training in the gynecological physical exam, interstitial and intracavitary brachytherapy procedures, and treatment planning. Since a simulator for brachytherapy procedures could not be identified on the current market, the simulator used for physical exam teaching will be adapted to allow for procedural-specific skill training. The interdisciplinary nature of brachytherapy, as well as the use of manual ultrasound-guidance present challenges for 2 ST. To help overcome these challenges, the training team consists of clinicians in gynecological oncology and radiation oncology to provide support for brachytherapy and physical exam training, as well as medical physicists with medical device development experience to assist in treatment planning, brachytherapy physics education, and simulator design. By integrating training in treatment planning with procedural training, ST will strongly root a foundational science – physics – in clinical practice. In a recent survey of radiation oncologists, lack of guidance, lack of time, and emphasis on passing exams were cited as barriers to brachytherapy teaching6. ST will address each of these barriers by providing multi-disciplinary guidance, a portable opportunity for learning at opportune times throughout training, and an emphasis on the need for procedural training. Currently, residents in radiation oncology are required by the Accreditation Council for Graduate Medical Education to perform 5 interstitial and 15 intracavitary brachytherapy cases over four years. At UCSF, the treatment of gynecological malignancies involves both interstitial and intracavitary brachytherapy techniques7. ST will provide residents with both an increased number of learning cases and a non-clinical environment in which skills can be practiced and mastered. Portability of the ST program could allow for dissemination to other sites, including developing countries, where high cervical cancer rates in young women make brachytherapy training highly valuable. The proposed ST represents a multi-disciplinary collaboration on an innovative teaching method, with the goal of training physicians to safely and skillfully address the gap between brachytherapy needs and utilization in the treatment of gynecological malignancies. 3 Evaluation An online survey will be administered to participants before and after ST, asking trainees to rate confidence in skills related to physical exam, brachytherapy procedure, and treatment planning. Trainees will also have the opportunity to provide anonymous feedback regarding the program. A post-test will also be administered asking trainees to answer multi-choice questions related to short clinical vignettes and requiring use of skills addressed in ST. Survey results and post-test performance will be used to evaluate the ST program. 4 1. Kumar RV, Bhasker S. Optimizing cervical cancer care in resource-constrained developing countries by tailoring community prevention and clinical management protocol. Journal of Cancer Policy. 2014;2(2):63-73. doi:10.1016/j.jcpo.2013.11.002. 2. Han K, Milosevic M, Fyles A, Pintilie M, Viswanathan AN. Trends in the Utilization of Brachytherapy in Cervical Cancer in the United States. International Journal of Radiation Oncology*Biology*Physics. 2013;87(1):111-119. doi:10.1016/j.ijrobp.2013.05.033. 3. Gill BS, Lin JF, Krivak TC, et al. National Cancer Data Base Analysis of Radiation Therapy Consolidation Modality for Cervical Cancer: The Impact of New Technological Advancements. International Journal of Radiation Oncology*Biology*Physics. 2014;90(5):1083-1090. doi:10.1016/j.ijrobp.2014.07.017. 4. Tanderup K, Eifel PJ, Yashar CM, Pötter R, Grigsby PW. Curative radiation therapy for locally advanced cervical cancer: brachytherapy is NOT optional. Int J Radiat Oncol Biol Phys. 2014;88(3):537-539. doi:10.1016/j.ijrobp.2013.11.011. 5. Brown LC, Laack TA, Ma DJ, Olivier KR, Laack NN. Multidisciplinary medical simulation: a novel educational approach to preparing radiation oncology residents for oncologic emergent on-call treatments. Int J Radiat Oncol Biol Phys. 2014;90(3):705-706. doi:10.1016/j.ijrobp.2014.06.053. 6. Gaudet M, Jaswal J, Keyes M. Current state of brachytherapy teaching in Canada: A national survey of radiation oncologists, residents, and fellows. Brachytherapy. 2015;14(2):197-201. doi:10.1016/j.brachy.2014.11.004. 7. Tinkle CL, Weinberg V, Chen L-M, et al. Inverse Planned High-Dose-Rate Brachytherapy for Locoregionally Advanced Cervical Cancer: 4-Year Outcomes. Int J Radiat Oncol Biol Phys. 2015;92(5):1093-1100. doi:10.1016/j.ijrobp.2015.04.018. 5