LCRS: Endocrinology Usama Asif Endocrinology 4: Insulin secretion
advertisement

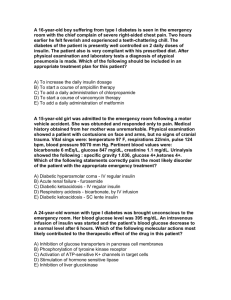
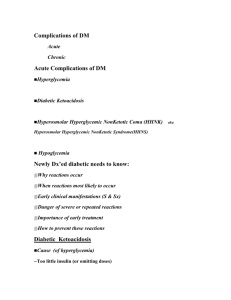
LCRS: Endocrinology Usama Asif ENDOCRINOLOGY 4: Insulin secretion & intermediary metabolism Dr Stephen Robinson (stephen.robinson@imperial.ac.uk) 1. Explain why the blood glucose concentration is closely regulated and list the hormones that control it - - - There are many factors that cause an increase in blood glucose level o Glucagon o Catecholamines o Somatotrophin o Cortisol However, there is just one factor that causes a decrease in blood glucose, and that is insulin Why is this the case? Well, glucose is an important substrate, particularly for the CNS, which relies on glucose entirely under normal conditions If blood glucose levels falls below the normal levels of 4-5mM – hypoglycaemia – then the brain function is impaired. Below a glood glucose of 2mM, coma and death occur Thus, one factor that decreases blood glucose is enough However, this leads to complications if insulin’s function is impaired: o Type 1 diabetes mellitus – defined as elevated glucose where insulin is required to prevent ketoacidosis – it is absolute insulin deficiency (markers = ketone bodies in the urine, glucose in urine and high bgl) o Type 2 diabetes mellitus – a more common health problem and a considerable burden. It is also defined in terms of glucose but is related to hypertension and dyslipidaemia – it is acquired insulin resistance There is no cure for diabetes mellitus; treatments help symptoms, complications, morbidity and mortality. Treated with diet, insulin replacement etc. 2. Draw a labelled diagram illustrating the relationship between the different types of cell in the islets of Langerhans. Describe the endocrine pancreas 3. Describe the structure of a typical islet of Langerhans, identifying the different cellular components and their principal endocrine secretions - The pancreas is important in the homeostasis of glucose (among other things) – the pathogenesis of diabetes showed the importance of the pancreas Most – around 98% - of the pancreas is exocrine. These secretions go to the small intestine and include hydrolytic enzymes for digestion There are small clumps of cells within the pancreatic tissue – remaining 2% - called islets of Langerhans. These are the endocrine cells of the pancreas LCRS: Endocrinology - - Usama Asif The cells are joined with tight junctions and the spaces between the cells are where hormone concentration is high There are three types of cell in the islets: o α-cell – these secrete glucagon o β-cell – these secrete insulin o δ-cell – these secrete somatostatin Somatostatin, as well as inhibiting somatotrophin, inhibits both insulin and glucagon: 4. List and describe the principal actions of insulin - - Insulin’s principal action is to decrease blood glucose levels It does this by: o Increasing glycogenesis – to store glucose as glycogen o Increasing glycolysis – using up the intracellular glucose means that glucose from the blood can be taken up by cells with the concentration gradient o Increasing glucose transport into cells – increasing the number of glucose transport proteins (GLUT4) on hepatocyte and skeletal muscle cell membranes allows greater take up of glucose o Decreasing lipolysis/ketogenesis and increasing lipogenesis – so that less energy is released via fat oxidation and so that the body can get its energy requirements by using glucose – more glucose used, more taken up, decreasing blood glucose o Increasing amino acid transport, increased protein synthesis and decreased proteolysis – so that gluconeogenesis from amino acids is driven down because the amino acids are used up The stimuli that cause insulin secretion from the β-cells are: o Increased blood glucose o Certain amino acids o Certain gastrointestinal hormones o Glucagon! o Parasympathetic activity (β-receptors) LCRS: Endocrinology - There are things that inhibit insulin secretion too: o Somatostatin (from δ-cells) o Sympathetic activity (α-receptors) - All of the above things result in decreased blood glucose Usama Asif 5. Draw a labelled diagram illustrating the factors which regulate the release of insulin 6. Describe the beta-cell sensing mechanism of glucose 7. Describe the main features of insulin synthesis, storage and secretion - The glucose sensor in the β-cell is glucokinase (also known as hexokinase IV) The glucose transporter GLUT2 on the β-cell is responsible for the transport of glucose into the cell Glucokinase converts glucose to glucose-6-phosphate in the rate-limiting step. This G6P can go off and take part in metabolic pathways It allows the cell to ‘see’ the ambient glucose concentration and thus, a rise in G6P levels causes insulin synthesis and release LCRS: Endocrinology Usama Asif Insulin synthesis - Insulin is synthesised as preproinsulin from the ribosome Once it exits the rough endoplasmic reticulum, it folds and the signal peptide is cleaved at the rER This leaves proinsulin Proinsulin goes to the Golgi apparatus and is packaged into vesicles, along with enzymes. These enzymes cleave C-peptide from the proinsulin molecule to yield C-peptide and insulin: LCRS: Endocrinology Usama Asif Insulin storage and secretion - - - Glucose enters the β-cell of the pancreas via the GLUT2 protein Glucose is converted to G6P The G6P undergoes glycolysis and produces ATP The ATP-sensitive K+ channel is stimulated with the ATP produces This depolarizes the cell, because of the influx of potassium This opens the voltage-gated Ca2+ channel causing the influx of calcium into the cell The calcium causes the vesicles containing insulin to migrate to the cell membrane and fuse with it Insulin is released (along with Cpeptide) = regulated secretion 8. List and describe the principal actions of glucagon - Glucagon’s principal action is to increase blood glucose It does this by: o Increasing hepatic glycogenolysis – liberating glucose from glycogen stores in the liver o Increased amino acid transport to the liver – transporting amino acids to the liver for gluconeogenesis o Increased lipolysis – fat breakdown to provide energy instead of glucose conserves glucose levels, also increases gluconeogenesis - The stimuli that cause glucagon release are: o Decreased blood glucose o Certain amino acids o Certain gastrointestinal hormones o Parasympathetic activity (a lot) o Sympathetic activity (a little) - There are things that inhibit glucagon release: o Somatostatin o Insulin - All of the above result in increased blood glucose LCRS: Endocrinology Usama Asif 9. Draw a labelled diagram illustrating the factors which regulate the release of glucagon Glucagon-like peptide-1 (GLP-1) - This is a gut hormone that is secreted in response to nutrients in the gut It is a transcription product of the proglucagon gene from L cells It stimulates insulin and suppresses glucagon (treatment for diabetes?) It increases satiety It has a short half-life due to the rapid action of the enzyme dipeptidyl peptidase-4 (DPPG-4) (use DPPG-4 inhibitors to treat diabetes?) 10. Discuss the insulin receptor and its function - Insulin binds to the insulin receptor It binds to the α-subunits of the receptor This changes the β-subunits of the tyrosine kinase domains This allows proteins to bind to it and it causes phosphorylation of cell protein substrates LCRS: Endocrinology Usama Asif 11. Describe the synthesis, storage and secretion of glucagon 12. Give an overview of the principal metabolic pathways for carbohydrates, proteins and fats, and the hormones that regulate these pathways LCRS: Endocrinology Usama Asif ENDOCRINOLOGY 5: Insulin action Dr Stephen Robinson (stephen.robinson@imperial.ac.uk) 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Learning objectives List and describe the effects of insulin across intermediary metabolism Describe the endocrine regulation of intermediary metabolism (from previous lecture) Describe and explain the metabolic changes in the fed and fasted state List the principal signs and symptoms of diabetes mellitus, and relate them to the underlying pathophysiology Distinguish between diabetes mellitus types 1 and 2 Explain the aetiology of type 1 diabetes mellitus Define insulin resistance and explain how it is related to diabetes, dyslipidaemia, hypertension and ischaemic heart disease Describe the consequences of insulin resistance on glucose, lipid and protein metabolism Explain how reduced insulin action is related to T2DM Describe the physiology and risks of obesity Describe the pathophysiology of type 2 diabetes Explain the metabolic changes associated with insulin induced hypoglycaemia Give an overview of the principal metabolic pathways for carbohydrates, proteins and fats, and the hormones that regulate these pathways (from previous lecture) - - Insulin has many actions: o Glucose: Decrease hepatic glucose output Increase uptake and storage of glucose o Proteins Decrease proteolysis o Lipids Decrease lipolysis Decrease ketogenesis o Growth o Vascular effects o Ovarian function o Clotting function: activates plasminogen activator inhibitor protein (PAI-1) o Energy expenditure – relation to leptins Insulin is a regulatory hormone that is countered with a balance of counterregulatory hormones, as will be apparent The GLUT-4 glucose transporter - In muscle and adipose tissue, the GLUT-4 glucose transporter protein transports glucose into the cells. It is a carrier protein It lies in vesicles and when it is needed i.e. when insulin stimulates it to, it migrates to the cell surface and becomes a cell surface protein It results in a sevenfold increase of glucose uptake LCRS: Endocrinology - Usama Asif It has a hydrophobic membranous component and a hydrophilic core Hormonal control of proteins - Proteins are broken down via proteolysis to form amino acids in the digestive system and are transported to the muscle and the liver In muscle - These amino acids can be used to assemble new proteins via protein synthesis - Some of these amino acids can be transported into the circulation, these amino acids are gluconeogenic and are transported to the liver for such purposes - Insulin promotes protein synthesis and inhibits proteolysis and amino acid transport out of the cell - Growth hormone and IGF-1 also promote protein synthesis - Cortisol promotes proteolysis - Glucose is present in the blood all the time, not only after meals. It is stored in the liver as glycogen and in the muscle. It is a very important glucose store In the liver - When the gluconeogenic amino acids reach the liver, they are taken up by the hepatocytes - In the liver, they can undergo protein synthesis LCRS: Endocrinology - Usama Asif The proteins in the liver can undergo proteolysis to increase the amount of amino acids The amino acids can undergo gluconeogenesis, producing glucose, which is transported out of the liver to the blood Insulin promotes protein synthesis and inhibits gluconeogenesis in the liver to keep hepatic glucose output down A protein deficiency and glucagon promote proteolysis Glucagon, catecholamines and cortisol promote gluconeogenesis The carbohydrates formed are a short term energy source: Hormonal control of lipids In adipocytes - Glucose is transported into the adipocyte via GLUT4 - This glucose is converted to fatty acids via acetyl-coA and stored as triglycerides - Or, the glucose is converted to glycerol-3-phosphate, which can be used in the manufacture of triglycerides - After a meal, triglycerides are transported to the adipocytes via chylomicrons using the enzyme lipoprotein lipase - Triglycerides are broken down to form glycerol and fatty acids - Insulin promotes the action lipoprotein lipase and the action and number of GLUT4 proteins - Insulin inhibits lipolysis and promotes lipogenesis – it encourages the long-term storage of triglycerides in the adipocytes because once glucose is formed from the fat, it cannot convert back to glucose again - Catecholamines, cortisol and growth hormone promote lipolysis LCRS: Endocrinology Usama Asif In the liver - The circulation diverts blood from the gut to the liver via the hepatic portal vein. Adipocytes in this circulation have a bigger effect on metabolism and endocrine control than adipocytes anywhere else - Glycerol -> TG (lipogenesis) or glucose (gluconeogenesis) - Glycerol in the blood can travel to the liver and under gluconeogenesis there or lipogenesis – this is shown by the fact that hepatic gluconeogenesis accounts for 25% of hepatic glucose output after a 10 hour fast, implying that fats are now taking over energy release In the brain - The brain can use glucose and ketone bodies but cannot utilise fatty acids - When there is a reduced glucose input to the brain, the liver produces ketone bodies: o The free fatty acids from lipolysis circulate in the blood and are taken up into the liver o The liver converts them into fatty acyl-coA species and into acetyl-coA via β-oxidation o The acetyl-coA is converted to acetoacetate and 3-hydroxybutyrate – two ketone bodies that are released into the circulation for use by the brain - Insulin inhibits this pathway (to conserve the fats so glucose can be used up instead) and glucagon promotes this pathway LCRS: Endocrinology Usama Asif Hormonal control of carbohydrates In the liver - Glucose uptake into the liver occurs via the GLUT4 protein where it is converted to glucose-6phosphate - The G6P is converted to glycogen - glycogenesis - Glycogen is also converted back to G6P, which is converted back to glucose and released as hepatic glucose output – glycogenolysis - Insulin promotes glycogenesis and the number and action of the GLUT4 - Glucagon and catecholamines promote glycogenolysis In muscle - Glucose is stored in muscle as glycogen, as in the liver - It is taken up by the muscle cell via GLUT4 - Glucose is used in glycolysis and oxidative phosphorylation - Insulin promotes the action and number of GLUT4. It also promotes the conversion of glucose into glycogen and glycolysis - Growth hormone, catecholamines and cortisol do the opposite LCRS: Endocrinology Usama Asif Putting the above all together In the fasted state - There is a low insulin to glucagon ratio - The [glucose] is between 3.0-5.5mmol/L - There is a high [fatty acid] - There is a rising and then low [amino acid] when fasting is prolonged (due to proteolysis and gluconeogenesis) - The above all occur because: o Increased proteolysis o Increased lipolysis o Increased hepatic glucose output via glycogenolysis and gluconeogenesis o The muscle begins t use lipids as a source of energy o The brain uses glucose and later, ketones - When fasting is prolonged, there is increased ketogenesis In the fed state - Stored insulin is released - There is thus a high insulin to glucagon ratio - The hepatic glucose output is stopped o Increased glycogenesis o Decreased gluconeogenesis o Increased protein synthesis and decreased proteolysis o Increased lipogenesis LCRS: Endocrinology Usama Asif Diabetes mellitus Type 1 diabetes mellitus - Absolute insulin deficiency - This results in a hyperglycaemic state and the person presents as if they were in an exaggerated fasted state, regardless of whether or not they have eaten - This means: o There is hepatic glucose output of glucose and ketones o There is increased proteolysis so [amino acid] in the blood increases o Lipolysis increases too, so there are high levels of glycerol and fatty acids in the blood - Because the glucose is not being removed from the blood it is filtered out by the kidney, causing glycosuria – glucose in the urine - There is also ketonuria – ketone bodies in the urine Insulin induced hypoglycaemia - This is caused by an overdose of insulin given (normally as a treatment for diabetes) - The increased insulin causes: o Increased glucagon storage and glucose levels fall o Increased catecholamines This happens because these counteract insulin (see above) o Increased cortisol } - o Increased growth hormone Glucose does enter muscle There is increased hepatic glucose output later because of glycogenolysis and gluconeogenesis Lipolysis is increased It can be treated with glucagon Insulin resistance – type 2 diabetes mellitus - Insulin resistance would reside in the liver, adipose tissue and the muscle tissue - There is a lack of response from the insulin receptor - There is a post-receptor effect on the metabolic pathway of glucose o There is an increase in the circulating fatty acids o A decrease in lipoprotein lipase means that there is low VLDL clearance, this drives triglyceride concentrations up and MDL levels down o This also has an effect on the cholesterol levels – these increase o Triglyceride levels increase and HDL cholesterol clearance decreases - However, there is enough insulin response to suppress ketogenesis and proteolysis - Insulin resistance resides in the metabolic actions, thus, this causes compensatory hyperinsulinaemia in the pancreatic output, resulting in a mitogenic pathway being stimulated: - LCRS: Endocrinology - Insulin resistance causes: - Type 2 diabetes mellitus presents with: o Insulin resistance o Obesity (in 60%-80%) of cases o Dyslipidaemia o Later insulin deficiency o Hyperglycaemia o Less osmotic symptoms o With complications How to control diabetes? - Caloric intake control, reduce calories as fat and refined carbs Increase caloric intake as complex carbs and soluble fibre Decrease sodium Conclusion - - Insulin has effects across intermediary metabolism You should be able to describe intermediary metabolism with; o Insulin deficiency effect and T1DM o Insulin induced hypoglycaemia o Reduced insulin action and T2DM Diabetes is no longer a death sentence, it is now a life sentence Usama Asif