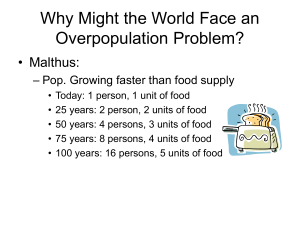
Chapter 6 – Cholera preparedness
advertisement

Annex 6E – Suggested logical framework for cholera preparedness and response Goal: To reduce the spread and limit mortality from cholera through an integrated approach CO-ORDINATION, INSTITUTIONAL FRAMEWORK, INFORMATION MANAGEMENT Objective: To improve leadership and coordination of cholera preparedness and response, ensuring a cholera risk reduction focus and including all related sectors, levels and stakeholders/partners. Expected result: Effective coordination mechanisms are established and provide guidance for all sectors and stakeholders/partners on common approaches and standards for cholera preparedness and response, ensure all gaps and vulnerabilities are covered without duplication. Outcome Multi-sectoral coordination framework for cholera preparedness and response (including taskforce and technical working groups, subnational coordination structures) is established and functional Suggested indicators Suggested activities - - - - 1 Terms of reference for the cholera taskforce with defined coordination arrangements and structures including technical (sub) working groups and sub-national coordination platforms with clear functions, roles and responsibilities # and % of meetings 1held by the multi-sectoral national taskforce per identified time period (daily or weekly during an outbreak, quarterly interoutbreak periods) # and % of meetings held by the sub-national taskforces (daily or weekly during an outbreak, quarterly inter-outbreak periods) # and % of cross border coordination meetings held (daily or weekly during an outbreak, quarterly inter-outbreak periods) Who does what where matrix document - - Reference (in the toolkit) Establish a cholera taskforce (or similar overall coordination mechanism) at national level, integrating all related sectors and stakeholders. Support coordination functions and regular meetings (to analyse epidemiologic data, conduct risk assessments, preparedness and response planning, reporting, information management, definition of technical standards, resource gap analysis and mobilization, etc.). Identify and define technical (sub) working groups (i.e. surveillance, case Chapter 5 management, WASH, community mobilization) as necessary for Annex 5A coordinating cholera preparedness and response activities. Identify and define coordination structures and leads at sub-national level, and promote their engagement into national activities. Set up cross-border coordination mechanisms among Ministries of Health and/or responsible authorities/stakeholders at local level. Develop a who does what where and when (4W) document and keep it updated on a regular basis. The denominator will depend on the time frame, if it is weekly, daily and over time in X # of months. UNICEF Cholera Toolkit v. 1.0 - Annexes Outcome Preparedness and response plans are developed with all key sectors and stakeholders Suggested indicators Suggested activities - Preparedness plan document Response plan document Preparedness and response checklist filled out by key responsible # and % of at risk districts/provinces have a cholera preparedness and response plan # of simulation exercises conducted on preparedness and response plans - # and % of health facilities or outreach staff that have technical standards and guidance available # and % or partners involved in cholera control have technical standards and guidance and are using them for control measures - - Cholera related sectors and actors receive technical support and guidance from the cholera taskforce/technical (sub) working groups - - - Cholera risk and capacity assessment identifies areas and communities at risk and capacity to prevent, prepare and respond to an outbreak Cholera related needs are identified based on a gap analysis and actions are defined to address the gaps - - Risk and capacity assessment document for preparedness Risk and capacity assessment during response Needs and gap assessment document (preparedness and response) Capacity and resource map document with actions against it to fill gaps Chapter 6 – Cholera preparedness - - Reference (in the toolkit) Conduct a national workshop with all key sectors and stakeholders to review the epidemiologic situation and risk assessment and produce a Chapter 6 preparedness and response plan with wide input Produce a preparedness plan with all key sectors and levels of service Annex 6A and delivery 6D Produce a response plan with all key sectors and levels of service delivery Conduct a national and sub-national simulation exercise to test plans Define and agree technical standards, standard operational procedures, and other technical guidance in all related sectors and levels Distribute key technical guidance, standards and tools to all partners and direct service providers including community health workers Chapter 6 Annex 6B Conduct a multi-sectoral risk and capacity assessment (preparedness and response) Identify areas for interventions for case management, WASH, enhanced Chapter 6 surveillance and early warning and communications (preparedness and response) Annex 6C Identify capacities gaps and what is required to be strengthened for cholera preparedness and response Conduct a needs and gap analysis with all key stakeholders to identify gaps in resources such as supplies, human resources, training and funding (preparedness and response) Based on needs and gap assessment identify a plan and responsible parties to fill gaps (preparedness and response) Chapter 6 Annex 6F and 6G Outcome Suggested indicators - Information on cholera preparedness and response activities is collected and analysed in a timely manner. Sector and partners receive it for guiding their implementation. - Communication plan document outlining the communication system and information management tools for operational response (all sectors) for preparedness and response # of cross border communication systems are established (where relevant) # and % of partners reporting to the cholera taskforce using pre-defined information management tools during response # and % of information bulletins published for partners and key stakeholders for cholera related activities (will vary if during preparedness and response) Reference (in the toolkit) Suggested activities - Define and implement information management tools/systems for cholera prevention and response (including epidemiological data, information on reported cases, information on CTC/CTU, information on community focused interventions) - Develop cross border communication channels where relevant - Train relevant staff on communications and information management - Analyse information from partners to identify needs and gaps in cholera response - Produce regular information bulletins outlining cholera preparedness and response activities Chapter 6 UNICEF Cholera Toolkit v. 1.0 - Annexes SURVEILLANCE AND EARLY WARNING AND MONITORING DISEASE TRENDS Objective: To improve early detection and consistent monitoring of disease trends Expected result: Cholera is detected early and monitored on a routine basis to inform action and adjust programs accordingly Outcome Suggested indicators Suggested activities - Early warning, alert and response network (EWARN) is set up in affected areas and those at high risk including across borders - # and % of alerts verified in the first 24 hours # and % of verified alerts responded to by partners within 48 hours - - Case-based surveillance for cholera is in place and functioning in affected areas and those at high risk for cholera - # and % health facilities meeting reporting deadlines (target 85%) # and % laboratories with no stock out of reagents # and % of weekly (daily) epidemiologic analyses completed # and % monthly summary reports - - Chapter 6 – Cholera preparedness Reference (in the toolkit) Set up and EWARN system using standard case definition with direct linkages to response from the health and WASH sectors (daily or weekly), including verification of rumours Train health staff and rapid response teams at all levels including the community on EWARN system Provide supplies and resources to manage the EWARN system Implement rapid field investigation and response to reported cases or alerts Chapter 3 Annexes 3A, 3D, 3E Set up or strengthen a case-based surveillance system in all health facilities, CTC/CTU and communities in affected areas or at risk areas and provide standard case definition Train health staff to use a uniform case definition for reporting of all suspected cases, and how to register using a line-listing that meets the case definition Collect stool specimens from 10-20 suspected cases for laboratory confirmation at the beginning of the outbreak, periodically throughout and to determine the end Where needed improve laboratory capacity through training, provision of laboratory supplies and periodic quality checks Map all cases to identify areas where cases are concentrated to better target areas for cholera control activities Analysis of and publication of a weekly (daily) surveillance data Analysis and publication of monthly summary reports Analyse data to identify and understand transmission routes and epidemiological trends Chapter 3 Annex 3C, 3F, 3G, 3H and 3I REDUCING / CONTAINING CHOLERA TRANSMISSION / SPREAD Objective: To prevent and control transmission of cholera among affected and at risk populations. Expected result: Transmission of cholera is eliminated/contained Reference (in the toolkit) Suggested indicators2 Suggested activities People access and use safe water supply for all purposes but specially for drinking and cooking - % of people accessing and using safe water (from chlorinated sources/by using household water treatment methods) for drinking and other purposes. - % of samples from water sources reporting more than 0.5 mg/l of FRC - % of people treating water for drinking at household level and having a FRC of 0.2 mg/l. - % of people recognising/indicating household water treatment and storage practices in FGD/household interviews and observation. - [Especially in high risk area and when there is indication of contamination of the water source] repair/ improve water points and undertake shock/emergency chlorination before they reinitiate their operation. - Undertake bucket chlorination in centralised water points (boreholes, wells, hand pumps). - [In areas where water supply systems are not available] Provide safe drinking water through water trucking, centralised treatment and distribution, etc. Train water vendors in safe water production and handling and in certain contexts in point of use/ household water treatment and [as appropriate] provide the required supplies for undertaking it. - Distribute supplies for household water treatment [including water containers, as per necessary]. - Monitor water quality at water distribution points and household level; and undertake follow up actions when problems are reported. Households, communities, institutions and food outlets practice safe food hygiene and follow national food safety standards (when existent) - % of inspections on institutions/outlets reporting good hygiene conditions - % of people recognising/indicating safe food hygiene practices in FGD/household interviews. - Train food providers on environmental health and food safety. - Communicate and undertake community mobilization to promote safe food practices among households. - Conduct regular inspections on institutions and food outlets to monitor Infants are given safe fluids and food - % of children under 6 months being exclusively breastfed - % of mothers using safe water in food production when they introduce solid food to infants -Provide health and hygiene education messages into all interventions at the community and facility level on how to ensure safe infant and young child feeding Outcome Chapter 9 Chapter 9 Chapter 7 and 9 2 The table presents suggested indicators for monitoring the accomplishment of the indicated outcomes. The list of activities aims to be as comprehensive as possible and should be selected depending on the specific context in which they are applied. UNICEF Cholera Toolkit v. 1.0 - Annexes Suggested indicators2 Outcome Risk of cholera transmission through excreta (faeces and vomit) is reduced because they are properly disposed People wash their hands with water and soap (or ash) at critical times Environmental hygiene is adhered to in markets and other public places 3 Suggested activities Reference (in the toolkit) - Undertake communication and community mobilization activities focused on behaviour/social-norms change, towards stop open defecation. - [When community facilities exist] support operation, maintenance and final disposal of excreta - [When other options are limited and the practice already exists] promote the use of flying toilets as a temporary measure, with special attention on effective collection, safe transport and disposal. - Communicate/train on appropriate procedures for disinfecting areas and materials soiled with faeces and vomit. - Distribute disinfectant (and sometimes tools for disinfection) at community level. - Household spraying is not recommended in all situations given its high resource/time consuming nature, lack of evidence on its effectiveness and issues around the risk of increased stigmatization of cholera patients and households. Chapter 7 and 9 - % of people washing their hands with soap (or ash) at critical times3. - % of households where soap [or ash] is available specifically for handwashing - % of public sanitation facilities where handwashing stations are available with soap (or ash) available for use - Undertake communication and community mobilization activities to promote handwashing with soap or ash [in cholera epidemics, use of sand is not recommended due the risk of it to be contaminated]. - Provide and maintain handwashing stations (ensuring soap is always available) as a complement of communal/public sanitation facilities (at markets, schools, and other institutions) and next to food preparation and serving / eating areas. - Distribute soap at household level [targeted for vulnerable groups, such as cholera patients’ families at CTC level], as part of non-food item kits. Chapter 7 and 9 - # of communal/public solid waste disposal sites created and in use - health risks around solid waste are contained, especially where contaminated with human faeces - Support activities on solid waste management, collection and disposal, with particular attention to markets and other public spaces - Establish solid waste management and disposal system and; with special emphasis on management and disposal of faeces in plastic bags (flying toilets), collected as part of the regular system. - Undertake communication and community mobilization activities to promote proper disposal of solid waste management at community level. Chapter 7 and 9 - [for development/prevention phase] % of communities reporting open defecation free status - % of people using appropriate sanitation facilities for excreta disposal [including disposal of children’s and babies faeces’] - % of people recognising/indicating practices for disinfecting items contaminated with faeces/vomit in FGD/household interviews. Critical times: Before handling and preparing food, eating or feeding; after defecating, cleaning children or attending somebody with cholera; after touching dead bodies during funerals. Chapter 6 – Cholera preparedness Outcome Precautions to prevent cholera transmission are taken at gatherings, with specific focus on funerals and when handling dead bodies [Especially in high risk areas] People identify the risk of cholera (and its transmission routes) and know how to prevent it. Reference (in the toolkit) Suggested indicators2 Suggested activities Chapter 9 - % of gatherings4 where safe food and personal hygiene practices are promoted and facilitated. - Train religious and community leaders, community health workers on how to keep people safe at gatherings (safe food and personal hygiene practices, with special emphasis on safe handling of dead bodies. - Provide/facilitate information and means for water treatment for drinking, handwashing stations, handling/disinfection dead bodies. - Undertake communication and community mobilization activities to promote proper hygiene measures in gatherings. - [With special emphasis on funerals] Identify risk practices for cholera transmission on gatherings and other social practices and use them to tailor communication/community mobilization activities. - % of people recognising cholera transmission routes and indicating measures for preventing it in FGD/household interviews and through observation - # of trained community mobilizers per 1,000 affected people. - Identify personal and community behaviours related to cholera [both, those which may increase the risk of transmission or provide a protective factor] and use it for developing IEC materials (printed, audiovisual, etc.). - Train community mobilizers on communication techniques and the use of IEC materials. Training should include information on case identification and referral. - Disseminate cholera preventive and response messages through various communication channels (mass media, interpersonal communication, through schools, etc.) [Each communication channel and type of messages has advantages and disadvantages. A complementary combination of them should be developed and used]. [Note: This must be linked with all other training/communication/ community mobilization-type of activities indicated before and should be part of the same communication strategy]. Chapter 7 and Annexes and chapter 9 This includes weddings, parties, funerals, religious/sports/political gatherings and any other congregation of people in which food might be sold/distributed and other “risky” hygiene practices are present (especially during funerals) can pose as special risk for cholera transmission 4 UNICEF Cholera Toolkit v. 1.0 - Annexes Outcome Transmission of cholera from CTC/CTU and other cholera treatment centres is eliminated through appropriate infection control measures Suggested indicators2 Suggested activities - # and % of CTC/CTU/health centres with appropriate isolation systems and practices in place - # and % of CTC/CTU/health centres using safe water supply. - # and % of CTC/CTU health centres using appropriate sanitation facilities, including disposal of wastewater and medical waste. - Train health staff on safe hygiene practices and handling of cholera patients, excreta (faces and vomit and contaminated items) and medical waste. - Provide means for isolation of cholera cases/treatment rooms within health facilities. - Provide appropriate water supply, including monitoring of water quality at a regular basis. - Provide handwashing facilities with disinfected water and soap, making them accessible for health staff, caregivers and patients. - Provide and maintain of appropriate sanitation facilities, ensuring they are easy to access and clean - Dispose faeces/excreta and wastewater appropriately, as part of the maintenance of the sanitation facilities (dislodging of latrines and final sludge disposal, wastewater treatment on site, etc.) Chapter 6 – Cholera preparedness Reference (in the toolkit) Chapter 8 Annex 8E and 8H, Annex 6G REDUCING CHOLERA MORBIDITY AND MORTALITY Objective: To reduce cholera morbidity and mortality Expected result: Early detection and appropriate case management of cholera to keep the CFR to < 1% Outcome Suggested indicators5 Establishment of a network of prepared Cholera Treatment Centres including ORP’s - - Children and adults who have AWD/cholera are effectively managed at treatment centers with quality services - - - # of CTC/CTU and ORP per population according to the national standards Map of all health facilities that have standards to be a treatment center Document outlining resource needs for treatment facilities including materials for a stockpile of supplies Warehouse supply list for stockpile # and % of health staff trained on case management protocols # and % of treatment facilities that have standard treatment guidelines available % no stockouts of supplies including ORS, zinc, IVF, antibiotics according to level of care) in CTC’s or other treatment facilities # and % of treatment facilities that have monitored quality of services in the last month (using CTC/CTU evaluation form) CFR for each treatment center Suggested activities Reference (in the toolkit) - Identify and map health facilities and partners with capacity to run cholera treatment centres. - Establish standards for setting up CTC/CTU’s and ORPs - Identify and train partners on how to establish treatment centers and monitor quality - Identify resource needs for the facilities including trained staff, supplies, data collection materials, oversight and funding - Stockpile heath, WASH and communications supplies and materials for use in high risk areas - Establish a database mapping all trainings completed by trainees and trainers for cholera - Establish a referral system Chpater and annexes 8 - Identify and train/refresh health staff including community health workers on early detection/active case finding, case management, infection control (see section above) in facilities and managing and reporting data - Distribute standard treatment guidelines for health staff at all levels - Provide health, WASH and communications supplies on a regular basis - Supervise health staff providing treatment on a routine basis - Monitor the quality of treatment centres on a regular basis - Integrate management of cholera into standard training for diarrhoea including IMCI and Integrated Community Case Management (iCCM) Chapter 8 Annex 8H 5 The table presents suggested indicators for monitoring the accomplishment of the indicated outcomes. The list of activities aims to be as comprehensive as possible and should be selected depending on the specific context in which they are applied. UNICEF Cholera Toolkit v. 1.0 - Annexes Cases in the community are detected early and adequately managed and referred - Population at risk is effectively vaccinated against cholera 6 7 - % of patients presenting at the health facility within 24h of developing symptoms # and % of community-based health works trained # trained community-based health workers/500 population % stockouts of community-based health worker supplies % of caregivers recognising/indicating why and how to access/use ORS, breastfeeding, proper feeding, care seeking, through FGD or household interviews. - Identify and train community-based health workers in detection, community-based surveillance, case management, hygiene and health promotion and reporting - Disseminate guidelines and standards to community-based health workers - Provide materials such as ORS, zinc, aquatabs, IEC materials to community-based health workers - Establish ORP at community level and the associated supply chain. - Especially in high risk areas, distribute ORS at household level and disseminate information on how to access them at community level. - Identify suitable home-made rehydration fluids and define – with the responsible health authorities –endorsement/support for their use. - Undertake communication and community mobilization activities for early detection of dehydration, rehydration at household level (using ORS or another government- supported rehydration fluid6) and early care seeking for treatment7. - Set up case referral systems and train/provide information to community health workers on location of cholera treatment centres. Chapter 9 % coverage of target population with 2 doses of oral cholera vaccine (OCV) - Undertake risk assessment to inform on areas and population at risk and targeted for vaccination - Prepare a strategy for OCV use for target populations with all stakeholders - Procure OCVs from UNICEF supply division - Conduct a communications campaign for OCV with other key messages such as health, hygiene and sanitation. - Develop and carry out a vaccination campaign - Evaluate and document campaign results including coverage, acceptance and impact Chapter 4 Annex 4A They might be sugar-salt solution, rice-based ORS, among others, and their use should be approved and endorsed by the health authorities. Main messages should include that household-based treatment is only an immediate measure, and must be followed by care by trained health staff. Chapter 6 – Cholera preparedness