View/Open
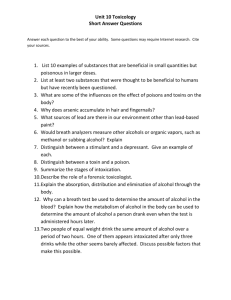
advertisement

Differences between Alveolar Air and Mouth Air For figures, tables and references we refer the reader to the original paper. In recent years, breath analysis has attracted a considerable amount of scientific interest. The volatile organic compounds (VOCs) in exhaled breath are representative of blood-borne concentrations through gas exchange in the blood/breath interface in the lungs. VOCs reflect products of metabolism in our body in the expired air. This enables monitoring of different processes in the body. As such, noninvasive breath analysis has the potential of replacing blood and urine analysis for many compounds. In this way, breath analysis could become extremely useful in the field of inhalation toxicology, where exposure to volatile compounds can be monitored by measuring the compound or its metabolites in the exhaled breath. An even more promising application of breath analysis is the diagnosis of different kinds of diseases.1 The ancient Greeks already knew that some diseases could be diagnosed from the typical odor of the patient's breath. Multiple diseases are characterized by a specific breath odor due to the presence of specific (often bad smelling) VOCs in breath (Table 1). In clinical practice, uncontrolled diabetes mellitus is characterized by the sweet smell of acetone, liver diseases by the smell of sulfur, and kidney failure reveals a fishy odor. These findings suggested that VOCs in exhaled breath can provide valuable information about the subjects' physiological and pathophysiological condition.2-5 Table 1. Intra- and Extraoral Causes of Halitosis (Bad Breath) and Their Related Compounds Breath analysis is a rapid and noninvasive technique. However, until recently, no adequate data were obtained because of the low VOC concentrations in breath, the high humidity of breath gas, and technical problems such as the lack of suitable sampling and analyzing techniques. Meanwhile, these problems have been overcome, and in the 1970s, Pauling detected more than 200 compounds in breath using gas chromatography (GC).6 GC followed by flame ionization detection,7-10 ion mobility spectrometry,8 and mass spectrometric detection11-13 has been widely used to separate, identify, and quantify a number of VOCs in human breath. As most VOCs in breath are present at levels of nanomoles or picomoles per liter, a preconcentration step is necessary. This can be achieved by absorption onto sorbent traps7-10,14,15 or by solid-phase microextraction8-11,16 prior to introduction of the sample into the GC. Preconcentrating breath gas followed by GC/mass spectrometry (GC/MS) seems to offer a reliable and sensitive method for VOC analysis.11-13 Before one can draw any conclusion from such GC/MS analysis, it is essential to know the compounds normally present in the breath of healthy volunteers, to act as a reference. A previous study reported substantial quantitative and qualitative differences in alveolar breath (air from the lungs) of normal humans. The concentration of VOCs varies widely (up to factor 10), and a number of VOCs were detectable in the breath of some subjects but not in others.13 In order to examine intraand extraoral diseases, a distinction between the oral and alveolar part of the breath is probably important. If mouth air, dead space air, and alveolar air are mixed, a dilution takes place. This dilution factor cannot be ignored because this factor unavoidably varies, e.g., when the test subject is breathing deeply or shallowly. Mixed expiratory sampling, which means that total breath is collected, has been used most often because this method is easy to perform in spontaneously breathing subjects. The present study examined for the first time the differences between alveolar air and mouth air for 40 healthy volunteers using GC/MS analysis. Materials and Methods Subject Selection. Forty volunteers (25 females) were enrolled (mean age 41). They were thoroughly questioned on their medical history. All confirmed they were not suffering from any known disease or were not receiving any medical treatment. Some took low-dose estrogen−progesterone combinations. All subjects signed an informed consent. The research was approved by the Clinical Trials Committee of the University Hospital of the Catholique University of Leuven. Sample Collection. Three samples per subject were taken: alveolar, oral, and environmental air, the latter to correct for differences in inhaled air. An adult expires ∼500 mL air with each breath. The first 150 mL is dead space air from the upper airways and nasopharynx, and the subsequent 350 mL is alveolar breath from within the lungs. Alveolar air was collected using a commercial device (BioVOC sampler, Markes International Limited, Rhondda Cynon Taff, UK). After 60 min of rest, the subjects performed a single slow vital capacity breath, into an inert, nonemitting Teflon bulb, which has an open end so that the first part of the breath passes through the sampler and only the last portion of exhaled air (150 mL) is trapped. Alveolar breath air was then transferred immediately from the sampler to a sorbent tube to capture all VOCs present in a sample. This procedure was repeated three times. In order to collect air from the mouth, a new Bio-VOC sampler was used. A specially designed coupling device, which fits a disposable mouthpiece, was placed at the open end of the sampler. Subjects were instructed not to breathe for 30 s. Then, air was drawn from the mouth to the Teflon bulb using a manual piston and transferred to a sorbent tube (repeated three times). The Bio-VOC sampler was also used to take a sample of room air (same procedure). Two-layer sorbent tubes containing 200 mg of TenaxTA and 200 mg of Unicarb (carbonized molecular sieve) (Markes International Limited) were used. The sorbent tubes were preconditioned with a constant flow (90 mL/min) of nitrogen (purity 6.0); a nitrogen purifier (Alltech Associates, Lokeren, Belgium) was used to further increase the purity) using the following temperature program: 1 h at 100 °C, 1 h at 200 °C, 1 h at 300 °C, and 30 min at 335 °C. They were then sealed by both Swagelok fitting and PFTE ferrules and stored at 4 °C. VOC Extraction and Analysis. Analysis of samples was performed by GC/MS combined with thermal desorption. An internal standard (2 μL, 0.5 mg/L p-bromofluorobenzene; Sigma-Aldrich-Fluka, Bornem, Belgium) was added using a Calibration Solution Loading Rig (Markes International Limited), which allows introducing calibration standards in the vapor phase. VOCs were desorbed and concentrated in a thermal desorber (Unity, Markes International Limited) at 250 °C onto a −10 °C cold trap for 6 min (helium flow 50 mL/min). The cold trap, packed with the same sorbents as the sorbent tubes, was then heated rapidly to 250 °C and VOCs were transferred to a gas chromatograph (HP6890N, Agilent Technologies, Diegem, Belgium). Column (capillary column, HP5MS, 30 m × 0.25 mm × 0.25 μm film thicknesses, Agilent Technologies) temperatures were ramped as follows: −40 °C for 1 min, 4 °C/min to 180 °C, 0.10-min hold and 30 °C/min to 300 °C, and 0.25-min hold. Liquid nitrogen was used as the cryogen. Column head pressure of helium carrier gas was set to 10 psi. Identification of VOCs occurred in a mass spectrometer (HP5973, Agilent Technologies). Mass range was applied from 10 to 350 amu. Data Management. Data from each chromatographic peak comprising retention time, library identification (NIST 98 library and a self-created database), and peak area (AUC, area under curve, response) were downloaded into a spreadsheet. VOCs were quantified by their ratio to the internal standard. Background VOCs were subtracted from VOCs in both mouth and alveolar breath. In this way, the gradient of each VOC was calculated as follows:12 A positive gradient indicates that the compound was formed endogenously or in the mouth, while a negative gradient indicates that the compound was derived from the environment. Statistical Analysis. The following procedure was used to identify the compounds that differ significantly between alveolar and mouth air. Altogether, 618 compounds were detected. In a first step, only those compounds that were present in at least 20 test subjects (50%) were selected. This resulted in 131 compounds. For every compound, a paired Wilcoxon test was performed. To correct for multiple testing, a Bonferroni correction (more stringent) and the Benjamini and Hochberg false discovery rate (Hochberg correction) (less stringent) were used. Results General Data. The chromatogram of the breath of a single person contained on average 145 compounds. The number of compounds was higher (p < 0.001) in mouth air (mean 152 compounds, SD 31) than in alveolar air (mean 139 compounds, SD 34). Altogether, 618 compounds were detected (533 in alveolar air, 519 in mouth air). In the environmental air, 387 compounds could be detected. Data of the environmental air are shown in Table 2. For alveolar air, 345 compounds had a positive gradient while 188 compounds had a negative gradient. For mouth air, the gradient was positive for 379 compounds and negative for 140 compounds. A total of 131 compounds could be detected in the breath of at least 50% of the test subjects. Other compounds were mostly present in the breath sample of only one volunteer. 35 compounds were common for all volunteers. In Table 3, all compounds present in the breath of at least 80% of the subjects are given together with the compounds with the highest gradient in both sorts of air. Table 2. VOCs Present in at Least 70% of the Environmental Samples, Ranked by Abundance a a Grad, gradient.b RT, retention time. Because alkylbenzenes and branched chain alkanes are difficult to distinguish from each other, they are given here with their retention time. Table 3. Breath VOCs Ranked by Abundance and Retention Time a Percentage of subjects in whom the components could be detected.b Mouth, average gradient in mouth air.c Alveolar, average gradient in alveolar air.d Retention time. Because branched chain alkanes and alkylbenzenes are difficult to distinguish from each other, they are given here with their retention time.e The 10 most positive gradients in mouth air as well as in alveolar air are in italic type.f The 10 most negative gradients in mouth air as well as in alveolar air are indicated in bold g For the compounds with an abundance below 80%, only those belonging to the ten most positive or negative gradients in mouth or alveolar air are given Differences between Alveolar and Mouth Air. Statistical analysis resulted in the identification of 84 compounds with a significant difference between the gradients in alveolar and mouth air after Hochberg correction and 47 compounds after Bonferonni correction (Table 4). Table 4. Compounds with a Significant Difference between Alveolar Air and Mouth Air after Bonferonni Correction a Average gradient in mouth air.b Average gradient in alveolar air.c p-value after Bonferonni correction = original p-value × 618.d Retention time. Discussion In this study, GC/MS was used to examine the differences between alveolar air and mouth air in 40 healthy volunteers. Because of the very low concentrations of the VOCs in breath, preconcentrating was necessary. This was achieved by absorption onto sorbent traps containing Tenax TA and carbonized molecular sieve. Previous studies have reported low background concentrations of VOCs in cleaned Tenax TA sampling tubes.17,18 Some studies showed artifact formation in Tenax sampling for benzaldehyde, acetophenone, phenol,19-23 and some ketones and aldehydes.24 However, analysis of sorbent tube blanks showed that background levels of these compounds were negligible. Other studies reported benzene and toluene contamination.17 In our study, benzene was found in 50% of the blanks and care should be taken in interpreting these results. No other contamination was found in the blank runs. The results of a series of healthy volunteers indicate that GC/MS offers a detailed overview of the compounds in a person's breath. Part of the VOCs in the expired air originated from the subject's previous exposure to precursors, being the environment (negative gradient). Breath samples were taken at 10 different environments. This has largely increased the number of detected compounds because there was a marked difference between these different locations. Ethanol had the largest negative gradient, which is probably the result of the extensive use of it in the laboratory. In the environmental air, no less than 387 compounds were detected. In order to make a distinction between endogenous and exogenous compounds, it is thus necessary to make corrections for background concentrations of volatile compounds in the inspired air. In our study, gradients were calculated by subtracting inspired from expired air.12 For this technique, equilibration between VOCs in the body and room air is necessary. Therefore, test subjects had to be present in the room where sample collection occurred at least 60 min before measurements. Some compounds may have originated from food or liquid intake or use of tooth paste prior to examination. d-Limonene for example, the major component of the oil extracted from citrus rind, is present in many soda drinks and causes a large peak after drinking. Menthol is present in many tooth pastes. However, because this method will be used in clinical practice for diagnosis, we chose a general view of the breath composition of healthy, nonfasting people. We did not ask the volunteers to fast or to refrain from oral hygiene. Fasting is known to cause, for example, elevated concentrations of the ketones acetone, 2-pentanone, and 2-butanone.25 We did, however, ask the volunteers to refrain from eating garlic, onions, or any spicy food 24 h before measurements. Breath samples were also taken during the morning at least 30 min after consumption of any food or beverages and at least 2 h after oral hygiene. Other VOCs, frequently encountered in alveolar air, are of endogenous origin, conveyed to the lungs by the blood circulation and expired. Some of them were already identified as biomarkers for certain diseases. Acetone, the most abundant metabolite in alveolar air, is derived from decarboxylation of acetyl-CoA when lipolysis or lipide peroxidation occurs. Acetone levels are elevated in diabetes mellitus, which explains the sweet smell of the breath of these patients.26 Other ketones that were detected are 2-pentanone and 2-butanone, which have an acetone-like odor.27 2-Butanone is known to be a marker for lung cancer.28 2-Propanol, present in breath at much lower concentrations than acetone, is also believed to be associated with diabetes.29 It has an ethanol/acetone-like smell.27 Dimethyl sulfide is, together with other sulfides, responsible for the characteristic odor in the breath of cirrhotic patients. Sulfur compounds are generated by incomplete metabolism of methionine. Under normal conditions, concentrations of these compounds are very low.3 High levels of 1propanol have been associated with lung carcinoma.28 It has an alcoholic and slightly stupefying odor.27 A number of compounds were (exclusively or not) produced in the mouth and some of them may play a role in oral malodor. Dimethyl sulfide, one of the sulfides frequently associated with oral halitosis, is formed by anaerobic bacterial breakdown of sulfur-containing amino acids in the oral cavity.30 The higher gradient in mouth air for 1-propanol is believed to be the result of bacterial fermentation of threonine in the mouth. The number of compounds was significantly higher in mouth air than in alveolar air. In mouth air, environmental compounds can be detected that are metabolized and excreted in another way than by expiration. A total of 84 of the 131 compounds present in the breath of at least 50% of the subjects showed a significant difference between alveolar and mouth air after Hochberg correction. Even after Bonferonni correction, which is a very stringent method to correct for multiple testing, 47 compounds could be detected with a significant difference. In most cases, this difference probably reflects the site of production (e.g., endogenous pathways of acetone, 2-pentanone, and isoprene). The alkanes and branched chain alkanes, which are clearly elevated in mouth air, are believed to be derived from cosmetic products like toothpaste. Some compounds have a negative gradient in both alveolar air and mouth air and are the result of background contamination (e.g., ethanol, xylenes). For methenamine, a very significant difference was found between alveolar (mean −7,67) and mouth air (mean 8,49). Methenamine is formed by a reaction of formaldehyde and ammonia and is also present in the environmental air. The reason for the large gradient in mouth air is not clear. An hypothesis is that because the equilibrium of the reaction between formaldehyde and ammonia is heavily weighted in favor of methenamine in an aqueous environment, more methenamine is formed in the mouth due to the saliva. In the body, methenamine is metabolized into ammonia and formaldehyde, which in turn breaks down into formate that is excreted in the urine or into carbon dioxide that is expired. Within the limits of this experimental setup, one could conclude that GC/MS makes it possible to analyze in detail the compounds in a person's breath. In this way, it may become a powerful tool for diagnosis of different diseases. Further research will be necessary to find out which compounds play a crucial role in the different pathologies. Because of the important influence of the environment and the large intersubject variation for some compounds, care should be taken when using breath analysis for diagnosis. The distinction between alveolar air and mouth air seems relevant because of the clear differences between thesetwo sorts of air and because some compounds can be produced both intraorally and endogenously (e.g., dimethyl sulfide). Acknowledgment This study was supported in part by the Fund for Scientific Research−Flanders and GABA International, Münchenstein, Switzerland.