Supplementary Information (docx 223K)
advertisement
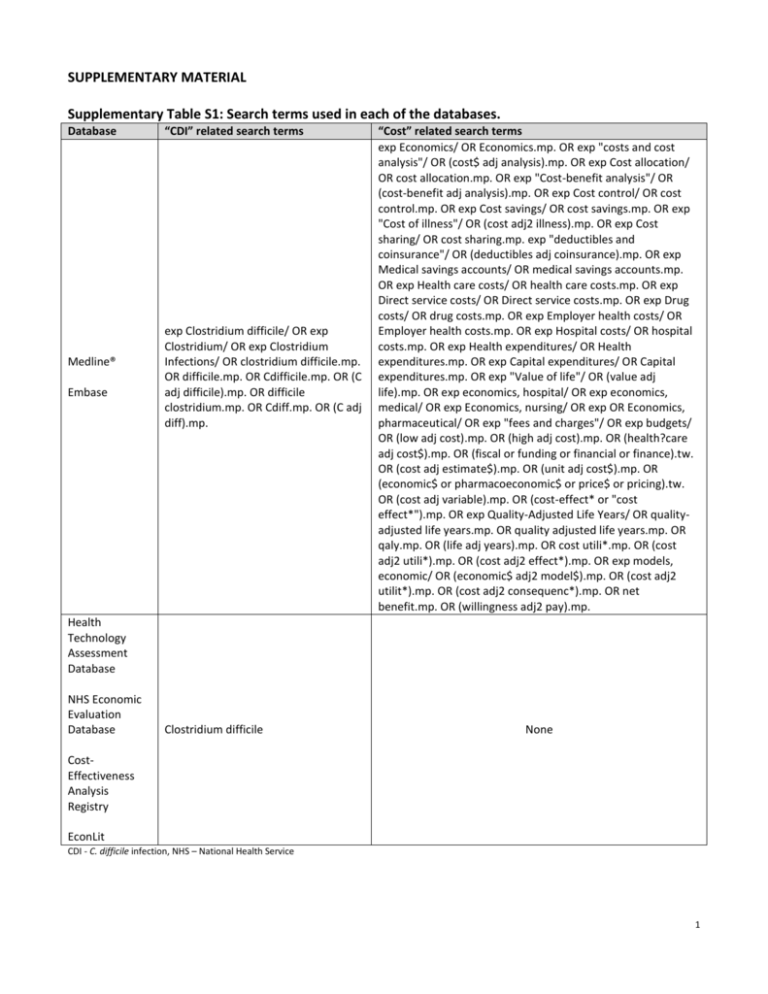
SUPPLEMENTARY MATERIAL Supplementary Table S1: Search terms used in each of the databases. Database Medline® Embase “CDI” related search terms exp Clostridium difficile/ OR exp Clostridium/ OR exp Clostridium Infections/ OR clostridium difficile.mp. OR difficile.mp. OR Cdifficile.mp. OR (C adj difficile).mp. OR difficile clostridium.mp. OR Cdiff.mp. OR (C adj diff).mp. “Cost” related search terms exp Economics/ OR Economics.mp. OR exp "costs and cost analysis"/ OR (cost$ adj analysis).mp. OR exp Cost allocation/ OR cost allocation.mp. OR exp "Cost-benefit analysis"/ OR (cost-benefit adj analysis).mp. OR exp Cost control/ OR cost control.mp. OR exp Cost savings/ OR cost savings.mp. OR exp "Cost of illness"/ OR (cost adj2 illness).mp. OR exp Cost sharing/ OR cost sharing.mp. exp "deductibles and coinsurance"/ OR (deductibles adj coinsurance).mp. OR exp Medical savings accounts/ OR medical savings accounts.mp. OR exp Health care costs/ OR health care costs.mp. OR exp Direct service costs/ OR Direct service costs.mp. OR exp Drug costs/ OR drug costs.mp. OR exp Employer health costs/ OR Employer health costs.mp. OR exp Hospital costs/ OR hospital costs.mp. OR exp Health expenditures/ OR Health expenditures.mp. OR exp Capital expenditures/ OR Capital expenditures.mp. OR exp "Value of life"/ OR (value adj life).mp. OR exp economics, hospital/ OR exp economics, medical/ OR exp Economics, nursing/ OR exp OR Economics, pharmaceutical/ OR exp "fees and charges"/ OR exp budgets/ OR (low adj cost).mp. OR (high adj cost).mp. OR (health?care adj cost$).mp. OR (fiscal or funding or financial or finance).tw. OR (cost adj estimate$).mp. OR (unit adj cost$).mp. OR (economic$ or pharmacoeconomic$ or price$ or pricing).tw. OR (cost adj variable).mp. OR (cost-effect* or "cost effect*").mp. OR exp Quality-Adjusted Life Years/ OR qualityadjusted life years.mp. OR quality adjusted life years.mp. OR qaly.mp. OR (life adj years).mp. OR cost utili*.mp. OR (cost adj2 utili*).mp. OR (cost adj2 effect*).mp. OR exp models, economic/ OR (economic$ adj2 model$).mp. OR (cost adj2 utilit*).mp. OR (cost adj2 consequenc*).mp. OR net benefit.mp. OR (willingness adj2 pay).mp. Health Technology Assessment Database NHS Economic Evaluation Database Clostridium difficile None CostEffectiveness Analysis Registry EconLit CDI - C. difficile infection, NHS – National Health Service 1 Supplementary Table S2: Quality assessment tool and how it was applied the COI studies. The application of each question to a COI study Section(s) in which the item should be found Answer options 1. The research question is stated Does the objective state that the economic impact of the disease is being determined? Examples of other terms that can be used include: cost, expenses, economic burden, financial impact If the actual disease (e.g., CDI) is not mentioned in the objective but represented within a group of diseases (e.g., hospital acquired infections), then put “partially” Objective Y N P 2. The economic importance of the research question is stated If question 1 is "yes" or “partially” then is the rationale behind the cost analysis stated? If question 1 is "no" then put “not applicable” Introduction Objective Y N NA Introduction Objective Y N P Objective Methods Y N P Does the study state which cost outcomes are being evaluated? For example, cost per patient, cost per episode, total cost Methods Results Y N Does the study provide details on the sample population in which the costs are being obtained from? For example, demographics Results Y N Does the study evaluate indirect costs? Objective Methods Y N NA If question 7 is "yes" then answer "yes" or "no" If question 7 is "no" then put "not applicable" Introduction Objective Methods Discussion Y N NA Are resource utilization variables reported separately from their costs? For example, if hospitalization costs are reported, is length of stay provided? Or if physician costs are provided, are number of physician visits reported? Results Y N Questions from Drummond and Jefferson (1) 3. The viewpoint(s) of the analysis are clearly stated and justified 4. The form of economic evaluation used is stated 5. The primary outcome measure(s) for the economic evaluation are clearly stated 6. Details of the subjects from whom valuations were obtained are given 7. Productivity changes (if included) are reported separately 8. The relevance of productivity changes to the study question is discussed 9. Quantities of resources are reported separately from their unit costs Does the study state the "perspective" or "viewpoint" of the cost analysis? Examples of perspectives include: hospital, government, patient, insurance company, society, caregiver A justification behind the perspective chosen should also be stated If the perspective is only stated and not justified, then put "partially" Are the epidemiological approach (e.g., incidence/prevalence-based approach (2, 3)) and method of resource quantification (e.g., topdown/bottom-up approach (2, 3)) stated? If one or the other is stated then put “partially” 2 Questions from Drummond and Jefferson (1) 10. Methods for the estimation of quantities and unit costs are described 11. Currency and price data are recorded 12. Time horizon of costs and benefits is stated The application of each question to a COI study Does the study describe how resource utilization and costs are estimated? For example, are they obtained from a survey, a database, or expert opinion? If the methods of either the resource utilization variables or costs are only reported, then put "partially" If the methods are discussed in the results or discussion sections then put “partially” Does the study state the year and currency in which the costs are evaluated in? If only one or the other is stated then put "partially" Does the study state the time horizon in which the costs are evaluated over? For example, costs over hospitalization/admission, year, lifetime Section(s) in which the item should be found Answer options Methods Y N P Methods Results Y N P Methods Results Y N 13. The discount rate(s) is stated If future costs are calculated, are the costs discounted? Methods 14. The choice of rate(s) is justified If question 13 is "no" then put down "not applicable" Methods 15. An explanation is given if costs or benefits are not discounted If question 13 is "no" then put down "not applicable" Methods 16. Details of statistical tests and confidence intervals are given for stochastic data 17. The approach to sensitivity analysis is given 18. The choice of variables for sensitivity analysis is justified 19. The ranges over which the variables are varied are stated 20. Incremental analysis is reported 21. Major outcomes are presented in a disaggregated as well as aggregated form 22. Conclusions are accompanied by the appropriate caveats Are descriptive statistics presented for cost estimates (e.g., mean, median, standard deviation, max, min, range)? Are confidence intervals or p-values given? If either/or is stated, then put "partially" Is a sensitivity analysis conducted around costs? If the description of sensitivity analysis is found in the results and discussion sections, put “partially” Results Methods Y N NA Y N NA Y N NA Y N P Y N P Y N NA Y N NA If question 17 is "no" then put "not applicable" Methods If question 17 is "no" then put "not applicable" Methods Did the study mention the use of a comparison group? If this is done for only part of the cohort then put “partially” Results Y N P Are the costs reported by subgroups, such as sex, age, region, resource? Results Y N Are the limitations around the cost analysis (e.g., cohort, cost methods) discussed? Discussion Conclusions Y N COI - Cost of illness; CDI - C. difficile infection; Y- Yes; N – No; P- Partially; NA- Not applicable. 3 p-value - - $13,819 <0.05 Study results and expert opinion 6w (Jan and Apr 1997) LOS Mean cost per patient SUM $11,240 - - - St. Paul’s Hospital 1y (1996) 1y Cost per patient SUM $714 - - - Hospitalization, procedures, drugs Hannover Medical School finance department 1y (2006) LOS Median cost per patient HM - - $9,730 - Hospitalization, laboratory, drug therapy Antrim Area Hospital Corporate Information Department 2y LOS Mean cost per case SUM - - $4,124 - Surgery, pharmaceuticals, laboratory, radiology, nursing care, and other Japanese Diagnosis Procedure Combination database 2y (Jul to Dec for each year from 2007 to 2010) LOS Total costs SUM RA PSM $33,547 $33,547 $23,670 $26,580 $6,814 $6,967 <0.001 <0.001 <0.001 Bed, treatment, laboratory Study results, government sources, and expert opinion 7m (Dec 1994 to Jun 1995) LOS Mean cost per patient SUM - - $9,703 - SUM $40,186$78,933 - - - - -$1,522$18,563 <0.05 for groups 1, 2, and 5 Cost of comparison group (US 2014 $) RA Cost of those with CDI (US 2014 $) Mean cost per episode Type of method to calculate costs Attributable cost (US 2014 $) Cost outcome(s) Time horizon for costs LOS Time frame of data extraction 2y (2005 to 2007) Resource and cost sources Computerized clinical costing systems Resource utilization variables included Sample size of comparison group Sample size of those with CDI CDI definition based on Patient population Author and year of publication Supplementary Table S3: Summary of CDI COI studies by country. Australia Jackson 2011 (4) Hospitalized ICD code 233 - CDI readmission LAB, SYM 10 - Hospitalized LAB 100 - Hospitalized LAB, SYM 45 - Hospitalized LAB, SYM 87 - Hospitalization Canada Miller 2002 (5) Butterworth 1998 (6) Hospitalization and antibiotic therapy Laboratory and antibiotic therapy Germany Vonberg 2008 (7) Ireland Al-Eidan 2000 (8) Japan Yasunaga 2012 (9) Hospitalized, underwent elective digestive tract surgery for cancer ICD code Hospitalized, >65 years LAB, SYM 143,243 409 409 (PSM) United Kingdom Wilcox 1996 (10) 50 92 United States Hospitalized: 1) > 65 years; 2) renal disease; 3) cancer; 4) IBD; 5) concomitant antibiotic use LAB Jiang 2013 (12) Hospitalized ICD code 1,211 6,053 Hospitalization Pant 2013 (13) Hospitalized, children with IBD ICD code 447 12,163 Hospitalization Campbell 2013 (11) 4,521 - Hospitalization Health Facts electronic health record database Rhode Island Department of Health’s Centre for Health Data and Analysis Healthcare Cost and Utilization Project Kids’ Inpatient Database LOS Mean hospital costs (depending on the patient group) PSM 2y (Jan 2010 to Dec 2011) LOS Mean costs Median costs PSM $35,473 $20,998 $17,474 $9,714 $17,999 $11,284 <0.0001 - 1 year (2009) LOS Mean hospitalization charges RA $46,084 $35,439 $10,644 <0.001 6 y and 2 m (Apr 2005 to Jun 2011) - 4 Attributable cost (US 2014 $) Type of method to calculate costs Cost outcome(s) Time horizon for costs Time frame of data extraction LOS Mean hospitalization cost RA $42,027$201,174 $22,19678,878 $11,823$122,295 <0.001 Sammons 2013 (15) Hospitalized, children, community- and hospital-onset of CDI ICD code, LAB 4,474 8,821 Hospitalization Pediatric Health Information System database 5 y and 8 m (Jan 2006 to Aug 2011) LOS Mean total cost PSM, RA - - $19,207$95,118 - $32,921 26,674 $6,247 - 1.5 y (Jan 2007 to Jun 2008) $21,245 $16,987 $4,258 - Tabak 2013 (16) Wilson 2013 (17) Ali 2012 (18) Kim 2012 (19) Kuntz 2012 (20) Hospitalized Hospitalized, underwent closure of loop ileostomy Hospitalized, underwent liver transplants Hospitalized, underwent radical cystectomy for bladder cancer Patients identified with CDI in an outpatient and inpatient setting Lipp 2012 (21) Hospitalized McGlone 2012 (22) Hypothetical sample, hospitalized, >65 years (recurrence of CDI included in economic model) Pant 2012 (23) Hospitalized, underwent solid organ transplants LAB 255 765 Hospitalization Hospitals, clinical research database from CareFusion, and Centers for Medicare and Medicaid Services ICD code 217 13,245 Hospitalization Nationwide Inpatient Sample ICD code 5,159 193,174 Hospitalization Nationwide Inpatient Sample ICD code - - Hospitalization Nationwide Inpatient Sample - Emergency department visits, laboratory, pharmacy, physician visits, hospitalization - Hospitalization - Hospitalization, diagnostic procedures, drugs, surgical procedures, loss in productivity ICD code, LAB, AT (OPTS) 1,3161,650 ICD code (IPTS) ICD code - ICD code - - - - Hospitalization 5y (2004 to 2008) 5y (2004 to 2008) Mean cost per case LOS Median cost per case PSM p-value 5 y and 10 m (Jan 2005 to Oct 2010) Cost of comparison group (US 2014 $) HealthCore Integrated Research Database Cost of those with CDI (US 2014 $) Hospitalization Resource and cost sources 93332,799 Resource utilization variables included 93310,933 Sample size of comparison group Sample size of those with CDI ICD code Patient population CDI definition based on Author and year of publication Quimbo 2013 (14) Hospitalized: 1) immunocompromised; 2) CDI history; 3) concomitant antibiotic use; 4) renal impairment; 5) IBD; 6) > 65 years LOS Mean costs SUM RA $41,232 - $17,635 - $23,597 $20,399 <0.001 LOS Mean hospital charges SUM $148,173 $75,641 - <0.01 8y (2001 to 2008) LOS Hospitalization cost RA $57,368 $32,359 - <0.001 Kaiser Permanente Northwest/Colorado, Medicare and Medicaid 3 y and 3 m (Jun 2005 to Sept 2008) 180 d Costs per patient SUM $1,875$12,503 - - - New York State Department of Health’s Statewide Planning and Research Cooperative System 2y (2007 to 2008) LOS Mean cost per infection RA - - $30,049 - - - - $9,745$17,962 - SUM $55,755 $32,627 - <0.001 RA - - $72,167 <0.001 Government and published sources Nationwide Inpatient Sample - 1y (2009) 1y LOS Median cost per case (depending on the perspective and recurrence rate) Median hospital charges Mean hospital charges 5 Hospitalized with endstage renal disease ICD code - - Hospitalization Nationwide Inpatient Sample 1y (2009) LOS Peery 2012 (25) Hospitalized ICD code 110,553 discharges - Hospitalization Nationwide Inpatient Sample 1y (2009) Verlee 2012 (26) Hospitalized ICD code 49,516 - Hospitalization Michigan Health and Hospital Association 7y (Jan 2002 to Dec 2008) St Luke’s Episcopal Hospital accounting database 1 y and 2 m (Mar 2007 to May 2008) Arora 2011 (27) Hospitalized LAB, SYM 85 - Daily ward, ICU, diagnostic tests, physician visits, other health professionals, pharmacy Glance 2011 (28) Hospitalized with trauma ICD code 768 148,888 Hospitalization Nationwide Inpatient Sample Lesperance 2011 (29) Hospitalized with elective colon resections ICD code 10,077 695,010 Hospitalization Nationwide Inpatient Sample Hospitalization Healthcare Cost and Utilization Project Kids’ Inpatient Database Nylund 2011 (30) Pakyz 2011 (31) Hospitalized, children Hospitalized ICD code ICD code, AT 21,274 10,857 10,474,454 19,214 Hospital care, laboratory, and drugs University Health System Consortium Clinical Resource Manager program 2y (2005 to 2006) 3y (2004 to 2006) 4y (1997, 2000, 2003, and 2006) 6y (Apr 2002 to Mar 2007) <0.001 <0.001 LOS Median costs SUM $7,019 - - - LOS Mean charges (depending on if principal or non-principal diagnosis) SUM $27,458$90,185 - - - 3m Median hospital costs (depending on Horn’s index score) SUM $9,080$72,667 - - - LOS Median cost SUM $35,212 $13,589 - - LOS Hospital charges SUM $141,939 $65,863 - <0.05 LOS LOS Hospitalization Nationwide Inpatient Sample 1y (2007) LOS Wang 2011 (33) Hospitalized ICD code 78,273 - Hospitalization Pennsylvania Health Care Cost Containment Council 4y (2005 to 2008) LOS Nationwide Inpatient Sample 1y (2005) LOS Hospitalization p-value $65,097 41,2074,032,865 - Attributable cost (US 2014 $) $58,713 - 41,207 - Cost of comparison group (US 2014 $) $129,363 - ICD code ICD code Cost of those with CDI (US 2014 $) SUM RA Hospitalized Hospitalized with cirrhosis Type of method to calculate costs Mean charges Stewart 2011 (32) Bajaj 2010 (34) Cost outcome(s) Time horizon for costs Time frame of data extraction Resource and cost sources Resource utilization variables included Sample size of comparison group Sample size of those with CDI CDI definition based on Patient population Author and year of publication Pant 2012 (24) Median hospitalization charges per patient (depending on the year) Mean hospitalization cost SUM $25,544$35,437 $9,611$12,079 - SUM $64,720 $33,546 - <0.001 for 1997, 2000, and 2006 <0.001 $39,590 $15,139 RA $63,988 $32,825 - - SUM PSM $24,689 $24,689 $9,781 $15,778 $8,911 <0.0001 $24,413 $12,005 $12,408 $12,078 $7,166 $4,913 $86,572 $38,934 - Median hospitalization cost Mean cost per patient Mean hospitalization cost Mean hospital cost per admission PSM Median hospital cost per admission Total hospitalization charges RA <0.0001 <0.001 6 Fuller 2009 (35) Hospitalized ICD code - Hospitalization 2,478 (California) Hospitalized, DRG 127, 148, 182, 415, and 416 - 524 7,107 - Hospital’s private administrative data Zilberberg 2009 (37) Hospitalized with prolonged acute mechanical ventilation ICD code 3,370 3,36361,442 Hospitalization Nationwide Inpatient Sample Hospitalized with IBD ICD code Dubberke 2008 (39) Nguyen 2008 (40) Hospitalized, nonsurgical Hospitalized with IBD (Crohn’s disease and Ulcerative colitis) LAB ICD code 2,804 342-439 - 77,366 34224,252 - Hospitalization Room and board, pharmacy, laboratory, radiology, respiratory therapy, physical therapy Hospitalization Nationwide Inpatient Sample Barnes-Jewish Hospital’s Medical Informatics and Trendstar financial databases Nationwide Inpatient Sample Song 2008 (41) Hospitalized LAB 630 630 - John Hopkins Hospital administrative finance system Lawrence 2007 (42) Hospitalized, ICU LAB 75 1,760 Hospitalization Barnes-Jewish Hospital financial accounting system California: 1y (Oct 2005 to Sept 2006) 5y (2002 to 2006) 1y (2005) 1y (2003) 1y (2003) 7y (1998 to 2004) 4 y and 10 m (Jan 2000 to Oct 2005) 2.5 y (Jul 1997 to Dec 1999) LOS LOS LOS LOS and 180 d Mean patient cost Charges (depending on the DRG) Mean hospital costs p-value Attributable cost (US 2014 $) Cost of comparison group (US 2014 $) Cost of those with CDI (US 2014 $) Type of method to calculate costs Cost outcome(s) Time horizon for costs LOS California: Office of Statewide Planning and Development Reed 2009 (36) Ananthakrishnan 2008 (38) Time frame of data extraction Resource and cost sources Resource utilization variables included Sample size of those with CDI CDI definition based on Patient population Author and year of publication Sample size of comparison group Maryland: Health Services and Cost Review Commission 1,282 (Maryland) Maryland: 1y (Jul 2007 to Jun 2008) Maryland: $18,529 RA - - California: $28,167 SUM $8,527$44,217 $5,080$26,347 - <0.001 SUM $82,860 $63,219 - <0.001 Total cost Median hospital charges PSM SUM $21,600 $14,885 $11,483 - - Mean hospital charges Median total costs RA - $12,604 - SUM $17,575 $7,537 - <0.001 Mean costs (depending on the time horizon) RA $9,275$16,088 $6,563$10,517 $2,712$5,571 - Median costs (depending on the time horizon) PSM $16,099$30,259 $10,777$16,541 $3,580$7,932 - Ulcerative colitis: $40,854 Ulcerative colitis: $27,372 - <0.0001 Crohn’s disease: $39,038 Crohn’s disease: $23,379 Mean hospital charges SUM LOS Median costs PSM $22,824 $26,024 -$3,200 - LOS Median cost per patient SUM $60,711 $24,623 - <0.001 LOS 7 O'Brien 2007 (43) Zerey 2007 (44) Kyne 2002 (45) McFarland 1999 (46) Hospitalized Hospitalized, surgical Hospitalized ICD code ICD code LAB. SYM Nonprincipal diagnosis: 2,656 8,113 - - 1,553,597 - Recurrent CDI LAB, SYM 209 - Kofsky 1991 (47) Hospitalized LAB 155 - Yannelli 1988 (48) Hospitalized, suspected CDI SYM 126 (positive and negative) - Hospitalization, pharmacy, laboratory, imaging, emergency department Massachusetts hospital discharge databases Hospitalization Nationwide Inpatient Sample 5y (1999 to 2003) LOS Hospitalization Beth Israel Deaconess Medical Centre Hospital billing system 5m (Jan 1998 to May 1998 LOS Medical billing records and laboratory charges 3y and 5m (Aug 1993 to Dec 1996) Hospital - Clinic visits, antibiotics, laboratory tests, enteric pathogen and fecal leukocyte examinations, room charge, physician visit, and procedures Bed, laboratory tests, medical treatment Laboratory testing 1y (2000) Mean cost per stay LOS Median cost per stay Principal diagnosis: SUM, nonprincipal diagnosis: HM $11,717$34,377 $6,840$15,876 Nonprincipal diagnosis: $15,690 p-value Attributable cost (US 2014 $) Cost of comparison group (US 2014 $) Cost of those with CDI (US 2014 $) Type of method to calculate costs Cost outcome(s) Time horizon for costs Time frame of data extraction Resource and cost sources Resource utilization variables included Sample size of comparison group Sample size of those with CDI CDI definition based on Patient population Author and year of publication Principal diagnosis: 1,036 - $6,244 Median total charges SUM $72,496 $19,772 - <0.0001 Total charges Median hospital cost RA SUM $16,263 $7,616 $88,902 - <0.0001 <0.0001 Hospital cost RA $4,852 0.003 LT Mean per person SUM $15,665 - - - 1y (1988) LOS Mean charges per patient SUM $3,764 - - - 1.5 y (Jan 1986 to Jun 1987) 1.5 y Total cost to the hospital SUM $4,591 - - - CDI – C. difficile infection; COI – Cost-of-illness; US – United States; ICD – International Classification of Diseases; y – Year(s); LOS – Length of stay; RA – Regression analysis; LAB – Laboratory tests (related to CDI); SYM – Symptoms (related to CDI); w – Week(s); SUM – Summation; HM – Hard matching; PSM – Propensity score matching; m – Month(s); IBD – Inflammatory bowel disease; AT – Antibiotic therapy (vancomycin and/or metronidazole); OPTS – Outpatient setting; IPTS – Inpatient setting; d – Day(s); DRG – Diagnosis Related Groups; ICU – intensive care unit; LT – Lifetime. 8 Supplementary Table S4: Quality assessment results. Country Australia Canada Germany Ireland Japan United Kingdom United States Author and year Jackson 2011 (4) Miller 2002 (5) Butterworth 1998 (6) Vonberg 2008 (7) Al-Eidan 2000 (8) Yasunaga 2012 (9) Wilcox 1996 (10) Campbell 2013 (11) Jiang 2013 (12) Pant 2013 (13) Quimbo 2013 (14) Sammons 2013 (15) Tabak 2013 (16) Wilson 2013 (17) Ali 2012 (18) Kim 2012 (19) Kuntz 2012 (20) Lipp 2012 (21) McGlone 2012 (22) Pant 2012 (23) Pant 2012 (24) Peery 2012 (25) Verlee 2012 (26) Arora 2011 (27) Glance 2011 (28) Lesperance 2011 (29) Nylund 2011 (30) Pakyz 2011 (31) Stewart 2011 (32) Wang 2011 (33) Bajaj 2010 (34) Fuller 2009 (35) Reed 2009 (36) Zilberberg 2009 (37) Ananthakrishnan 2008 (38) Dubberke 2008 (39) Nguyen 2008 (40) 1 [+] + + + + + + + + + + [+] + + + + + + + + + + [+] + + + - 2 + NA + + + + + NA + NA + NA + + + + NA NA NA + + + NA NA + + + + + NA + NA 3 + + + + + [+] - 4 - 5 + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + 6 + + + + + + + + + + + + + + + + + + + + + + + + + + + + - 7 NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA + NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA 8 NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA + NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA 9 + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + 10 [+] [+] [+] + + + [+] + + + + + + + + + + + + + + + + [+] + + + + + + + + + + + + 11 [+] [+] [+] [+] [+] [+] [+] + + + + + [+] + [+] + [+] [+] [+] [+] + 12 + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + 13 NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA + NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA 14 NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA 15 NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA 16 + [+] + [+] + [+] + + + + + + + + + [+] + + + [+] [+] [+] [+] [+] + + + + + [+] + + + + + 17 + + + [+] [+] - 18 NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA + NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA NA 19 NA NA NA NA NA NA NA + NA NA NA NA + NA NA NA NA NA + NA NA NA NA NA NA NA NA + NA + NA NA NA NA NA NA NA 20 + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + 21 + + + + + + + + + + + + + + + + + - 22 + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + 9 Country Author and year Song 2008 (41) Lawrence 2007 (42) O'Brien 2007 (43) Zerey 2007 (44) Kyne 2002 (45) McFarland 1999 (46) Kofsky 1991 (47) Yannelli 1988 (48) 1 + + + + + - 2 + NA + + NA + NA 3 + + - 4 - 5 + + + + + + + - 6 + + + + + + + - 7 NA NA NA NA NA NA NA NA 8 NA NA NA NA NA NA NA NA 9 + + + + + + + 10 + + + + + + + - 11 + + [+] - 12 + + + + + + + + 13 NA NA NA NA NA NA NA NA 14 NA NA NA NA NA NA NA NA 15 NA NA NA NA NA NA NA NA 16 [+] + [+] + + [+] [+] - 17 - 18 NA NA NA NA NA NA NA NA 19 NA NA NA NA NA NA NA NA 20 + + [+] + + - 21 + + + + + 22 + + + + + + - 1 The research question is stated; 2 The economic importance of the research question is stated; 3 The viewpoint(s) of the analysis are clearly stated and justified; 4 The form of economic evaluation used is stated; 5 The primary outcome measure(s) for the economic evaluation are clearly stated; 6 Details of the subjects from whom valuations were obtained are given; 7 Productivity changes (if included) are reported separately; 8 The relevance of productivity changes to the study question is discussed; 9 Quantities of resources are reported separately from their unit costs; 10 Methods for the estimation of quantities and unit costs are described; 11 Currency and price data are recorded; 12 Time horizon of costs and benefits is stated; 13 The discount rate(s) is stated; 14 The choice of rate(s) is justified; 15 An explanation is given if costs or benefits are not discounted; 16 Details of statistical tests and confidence intervals are given for stochastic data; 17 The approach to sensitivity analysis is given; 18 The choice of variables for sensitivity analysis is justified; 19 The ranges over which the variables are varied are stated; 20 Incremental analysis is reported; 21 Major outcomes are presented in a disaggregated as well as aggregated form; 22 Conclusions are accompanied by the appropriate caveats; “+” refers to “yes”; “[+]” refers to “partially”; “-“ refers to “no”; “NA” refers to “not applicable”; Questions 1 to 22 are from Drummond and Jefferson (1); See Supplementary Table 2 for our interpretation of each question; Table format is based on Davis et al (49). 10 REFERENCES FOR SUPPLEMENTARY MATERIAL 1. Drummond M, Jefferson T. Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 1996;313:275-83. 2. Larg A, Moss JR. Cost-of-illness studies: a guide to critical evaluation. PharmacoEconomics 2011;29:653-71. 3. Hodgson TA, Meiners MR. Cost-of-illness methodology: a guide to current practices and procedures. Milbank Memorial Fund Quarterly - Health & Society 1982;60:429-62. 4. Jackson T, Nghiem HS, Rowell D, et al. Marginal costs of hospital-acquired conditions: information for priority-setting for patient safety programmes and research. Journal of Health Services & Research Policy 2011;16:141-6. 5. Miller MA, Hyland M, Ofner-Agostini M, et al. Morbidity, mortality, and healthcare burden of nosocomial Clostridium difficile-associated diarrhea in Canadian hospitals. Infection Control and Hospital Epidemiology 2002;23:137-140. 6. Butterworth SA, Koppert E, Clarke A, et al. Recent trends in diagnosis and treatment of Clostridium difficile in a tertiary care facility. American Journal of Surgery 1998;175:403-7. 7. Vonberg RP, Reichardt C, Behnke M, et al. Costs of nosocomial Clostridium difficile-associated diarrhoea. Journal of Hospital Infection 2008;70:15-20. 8. Al-Eidan FA, McElnay JC, Scott MG, et al. Clostridium difficile-associated diarrhoea in hospitalised patients. Journal of Clinical Pharmacy & Therapeutics 2000;25:101-9. 9. Yasunaga H, Horiguchi H, Hashimoto H, et al. The burden of Clostridium difficile-associated disease following digestive tract surgery in Japan. Journal of Hospital Infection 2012;82:175-180. 10. Wilcox MH, Cunniffe JG, Trundle C, et al. Financial burden of hospital-acquired Clostridium difficile infection. Journal of Hospital Infection 1996;34:23-30. 11. Campbell R, Dean B, Nathanson B, et al. Length of stay and hospital costs among high-risk patients with hospital-origin Clostridium difficile-associated diarrhea. Journal of Medical Economics 2013;16:440-448. 12. Jiang Y, Viner-Brown S, Baier R. Burden of hospital-onset Clostridium difficile infection in patients discharged from Rhode Island hospitals, 2010-2011: application of present on admission indicators. Infection Control & Hospital Epidemiology 2013;34:700-8. 13. Pant C, Anderson MP, Deshpande A, et al. Health care burden of Clostridium difficile infection in hospitalized children with inflammatory bowel disease. Inflammatory Bowel Diseases 2013;19:1080-5. 14. Quimbo RA, Palli SR, Singer J, et al. Burden of Clostridium difficile-associated diarrhea among hospitalized patients at high risk of recurrent infection. Journal of Clinical Outcomes Management 2013;20:544-554. 11 15. Sammons JS, Localio R, Xiao R, et al. Clostridium difficile infection is associated with increased risk of death and prolonged hospitalization in children. Clinical Infectious Diseases 2013;57:1-8. 16. Tabak YP, Zilberberg MD, Johannes RS, et al. Attributable burden of hospital-onset Clostridium difficile infection: a propensity score matching study. Infection Control & Hospital Epidemiology 2013;34:588-96. 17. Wilson MZ, Hollenbeak CS, Stewart DB. Impact of Clostridium difficile colitis following closure of a diverting loop ileostomy: results of a matched cohort study. Colorectal Disease 2013;15:974-81. 18. Ali M, Ananthakrishnan AN, Ahmad S, et al. Clostridium difficile infection in hospitalized liver transplant patients: a nationwide analysis. Liver Transplantation 2012;18:972-8. 19. Kim SP, Shah ND, Karnes RJ, et al. The implications of hospital acquired adverse events on mortality, length of stay and costs for patients undergoing radical cystectomy for bladder cancer. Journal of Urology 2012;187:2011-2017. 20. Kuntz JL, Johnson ES, Raebel MA, et al. Epidemiology and healthcare costs of incident Clostridium difficile infections identified in the outpatient healthcare setting. Infection Control & Hospital Epidemiology 2012;33:1031-8. 21. Lipp MJ, Nero DC, Callahan MA. Impact of hospital-acquired Clostridium difficile. Journal of Gastroenterology and Hepatology 2012;27:1733-1737. 22. McGlone SM, Bailey RR, Zimmer SM, et al. The economic burden of Clostridium difficile. Clinical Microbiology & Infection 2012;18:282-9. 23. Pant C, Anderson MP, O'Connor JA, et al. Association of Clostridium difficile infection with outcomes of hospitalized solid organ transplant recipients: results from the 2009 Nationwide Inpatient Sample database. Transplant Infectious Disease 2012;14:540-7. 24. Pant C, Deshpande A, Anderson MP, et al. Clostridium difficile infection is associated with poor outcomes in end-stage renal disease. Journal of Investigative Medicine 2012;60:529-532. 25. Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012;143:1179-87.e1-3. 26. VerLee KE, Finks JL, Wilkins MJ, et al. Michigan Clostridium difficile hospital discharges: frequency, mortality, and charges, 2002-2008. Public Health Reports 2012;127:62-71. 27. Arora V, Kachroo S, Ghantoji SS, et al. High Horn's index score predicts poor outcomes in patients with Clostridium difficile infection. Journal of Hospital Infection 2011;79:23-6. 28. Glance LG, Stone PW, Mukamel DB, et al. Increases in mortality, length of stay, and cost associated with hospital-acquired infections in trauma patients. Archives of Surgery 2011;146:794-801. 12 29. Lesperance K, Causey MW, Spencer M, et al. The morbidity of Clostridium difficile infection after elective colonic resection-results from a national population database. American Journal of Surgery 2011;201:141-8. 30. Nylund CM, Goudie A, Garza JM, et al. Clostridium difficile infection in hospitalized children in the United States. Archives of Pediatrics & Adolescent Medicine 2011;165:451-7. 31. Pakyz A, Carroll NV, Harpe SE, et al. Economic impact of Clostridium difficile infection in a multihospital cohort of academic health centers. Pharmacotherapy:The Journal of Human Pharmacology & Drug Therapy 2011;31:546-51. 32. Stewart DB, Hollenbeak CS. Clostridium difficile colitis: factors associated with outcome and assessment of mortality at a national level. Journal of Gastrointestinal Surgery 2011;15:1548-55. 33. Wang L, Stewart DB. Increasing hospital costs for Clostridium difficile colitis: type of hospital matters. Surgery 2011;150:727-35. 34. Bajaj JS, Ananthakrishnan AN, Hafeezullah M, et al. Clostridium difficile is associated with poor outcomes in patients with cirrhosis: A national and tertiary center perspective. American Journal of Gastroenterology 2010;105:106-13. 35. Fuller RL, McCullough EC, Bao MZ, et al. Estimating the costs of potentially preventable hospital acquired complications. Health Care Financing Review 2009;30:17-32. 36. Reed IJF, Edris BA, Eid S, et al. Clostridium difficile: The new epidemic. Internet Journal of Infectious Diseases 2009;7. 37. Zilberberg MD, Nathanson BH, Sadigov S, et al. Epidemiology and outcomes of clostridium difficile-associated disease among patients on prolonged acute mechanical ventilation. Chest 2009;136:752-8. 38. Ananthakrishnan AN, McGinley EL, Binion DG. Excess hospitalisation burden associated with Clostridium difficile in patients with inflammatory bowel disease. Gut 2008;57:205-10. 39. Dubberke ER, Reske KA, Olsen MA, et al. Short- and long-term attributable costs of Clostridium difficile-associated disease in nonsurgical inpatients. Clinical Infectious Diseases 2008;46:497-504. 40. Nguyen GC, Kaplan GG, Harris ML, et al. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. American Journal of Gastroenterology 2008;103:1443-50. 41. Song X, Bartlett JG, Speck K, et al. Rising economic impact of clostridium difficile-associated disease in adult hospitalized patient population. Infection Control & Hospital Epidemiology 2008;29:823-8. 42. Lawrence SJ, Puzniak LA, Shadel BN, et al. Clostridium difficile in the intensive care unit: epidemiology, costs, and colonization pressure. Infection Control & Hospital Epidemiology 2007;28:123-30. 13 43. O'Brien JA, Lahue BJ, Caro JJ, et al. The emerging infectious challenge of clostridium difficileassociated disease in Massachusetts hospitals: clinical and economic consequences. Infection Control & Hospital Epidemiology 2007;28:1219-27. 44. Zerey M, Paton BL, Lincourt AE, et al. The burden of Clostridium difficile in surgical patients in the United States. Surgical Infections 2007;8:557-66. 45. Kyne L, Hamel MB, Polavaram R, et al. Health care costs and mortality associated with nosocomial diarrhea due to Clostridium difficile. Clinical Infectious Diseases 2002;34:346-53. 46. McFarland LV, Surawicz CM, Rubin M, et al. Recurrent Clostridium difficile disease: epidemiology and clinical characteristics. Infection Control & Hospital Epidemiology 1999;20:43-50. 47. Kofsky P, Rosen L, Reed J, et al. Clostridium difficile--a common and costly colitis. Diseases of the Colon & Rectum 1991;34:244-8. 48. Yannelli B, Gurevich I, Schoch PE, et al. Yield of stool cultures, ova and parasite tests, and Clostridium difficile determinations in nosocomial diarrheas. American Journal of Infection Control 1988;16:246-9. 49. Davis JC, Robertson MC, Ashe MC, et al. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporosis International 2010;21:1295-306. 14