2297_2969_CIBECabstr..
advertisement
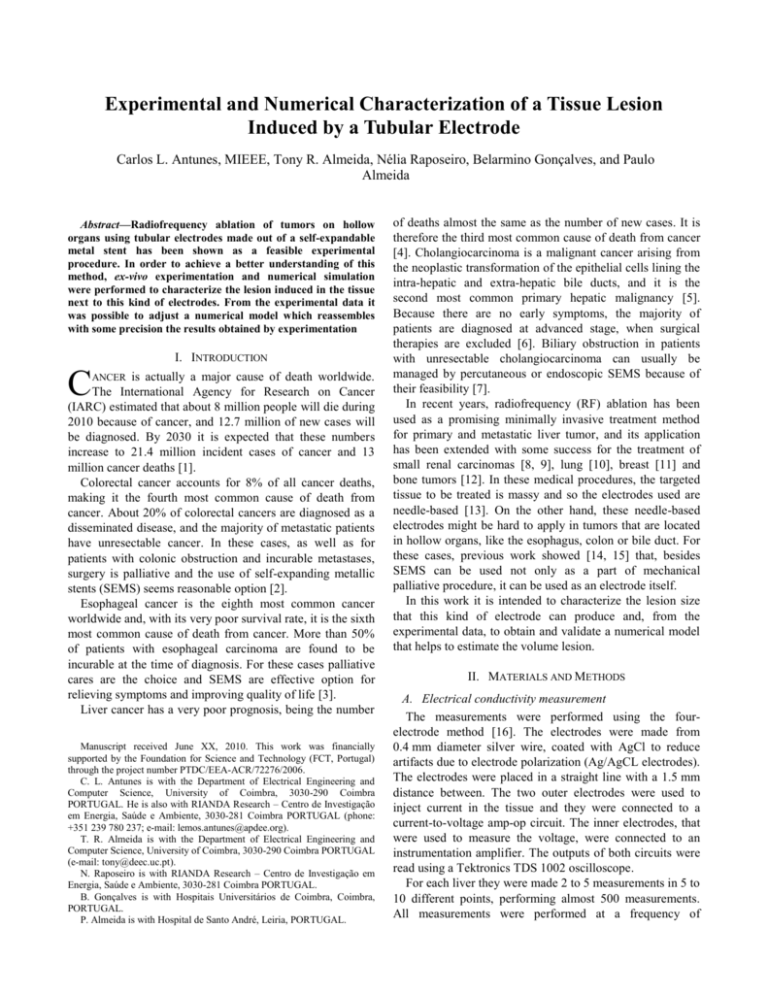
Experimental and Numerical Characterization of a Tissue Lesion Induced by a Tubular Electrode Carlos L. Antunes, MIEEE, Tony R. Almeida, Nélia Raposeiro, Belarmino Gonçalves, and Paulo Almeida Abstract—Radiofrequency ablation of tumors on hollow organs using tubular electrodes made out of a self-expandable metal stent has been shown as a feasible experimental procedure. In order to achieve a better understanding of this method, ex-vivo experimentation and numerical simulation were performed to characterize the lesion induced in the tissue next to this kind of electrodes. From the experimental data it was possible to adjust a numerical model which reassembles with some precision the results obtained by experimentation I. INTRODUCTION C is actually a major cause of death worldwide. The International Agency for Research on Cancer (IARC) estimated that about 8 million people will die during 2010 because of cancer, and 12.7 million of new cases will be diagnosed. By 2030 it is expected that these numbers increase to 21.4 million incident cases of cancer and 13 million cancer deaths [1]. Colorectal cancer accounts for 8% of all cancer deaths, making it the fourth most common cause of death from cancer. About 20% of colorectal cancers are diagnosed as a disseminated disease, and the majority of metastatic patients have unresectable cancer. In these cases, as well as for patients with colonic obstruction and incurable metastases, surgery is palliative and the use of self-expanding metallic stents (SEMS) seems reasonable option [2]. Esophageal cancer is the eighth most common cancer worldwide and, with its very poor survival rate, it is the sixth most common cause of death from cancer. More than 50% of patients with esophageal carcinoma are found to be incurable at the time of diagnosis. For these cases palliative cares are the choice and SEMS are effective option for relieving symptoms and improving quality of life [3]. Liver cancer has a very poor prognosis, being the number ANCER Manuscript received June XX, 2010. This work was financially supported by the Foundation for Science and Technology (FCT, Portugal) through the project number PTDC/EEA-ACR/72276/2006. C. L. Antunes is with the Department of Electrical Engineering and Computer Science, University of Coimbra, 3030-290 Coimbra PORTUGAL. He is also with RIANDA Research – Centro de Investigação em Energia, Saúde e Ambiente, 3030-281 Coimbra PORTUGAL (phone: +351 239 780 237; e-mail: lemos.antunes@apdee.org). T. R. Almeida is with the Department of Electrical Engineering and Computer Science, University of Coimbra, 3030-290 Coimbra PORTUGAL (e-mail: tony@deec.uc.pt). N. Raposeiro is with RIANDA Research – Centro de Investigação em Energia, Saúde e Ambiente, 3030-281 Coimbra PORTUGAL. B. Gonçalves is with Hospitais Universitários de Coimbra, Coimbra, PORTUGAL. P. Almeida is with Hospital de Santo André, Leiria, PORTUGAL. of deaths almost the same as the number of new cases. It is therefore the third most common cause of death from cancer [4]. Cholangiocarcinoma is a malignant cancer arising from the neoplastic transformation of the epithelial cells lining the intra-hepatic and extra-hepatic bile ducts, and it is the second most common primary hepatic malignancy [5]. Because there are no early symptoms, the majority of patients are diagnosed at advanced stage, when surgical therapies are excluded [6]. Biliary obstruction in patients with unresectable cholangiocarcinoma can usually be managed by percutaneous or endoscopic SEMS because of their feasibility [7]. In recent years, radiofrequency (RF) ablation has been used as a promising minimally invasive treatment method for primary and metastatic liver tumor, and its application has been extended with some success for the treatment of small renal carcinomas [8, 9], lung [10], breast [11] and bone tumors [12]. In these medical procedures, the targeted tissue to be treated is massy and so the electrodes used are needle-based [13]. On the other hand, these needle-based electrodes might be hard to apply in tumors that are located in hollow organs, like the esophagus, colon or bile duct. For these cases, previous work showed [14, 15] that, besides SEMS can be used not only as a part of mechanical palliative procedure, it can be used as an electrode itself. In this work it is intended to characterize the lesion size that this kind of electrode can produce and, from the experimental data, to obtain and validate a numerical model that helps to estimate the volume lesion. II. MATERIALS AND METHODS A. Electrical conductivity measurement The measurements were performed using the fourelectrode method [16]. The electrodes were made from 0.4 mm diameter silver wire, coated with AgCl to reduce artifacts due to electrode polarization (Ag/AgCL electrodes). The electrodes were placed in a straight line with a 1.5 mm distance between. The two outer electrodes were used to inject current in the tissue and they were connected to a current-to-voltage amp-op circuit. The inner electrodes, that were used to measure the voltage, were connected to an instrumentation amplifier. The outputs of both circuits were read using a Tektronics TDS 1002 oscilloscope. For each liver they were made 2 to 5 measurements in 5 to 10 different points, performing almost 500 measurements. All measurements were performed at a frequency of 470 kHz, which corresponds to the output voltage frequency of the ValleyLab RF power generator used during experimentation. Fig. 1. The four-electrode probe made for measuring the electrical conductivity. B. Ex-vivo experimentation Experimental work was performed on bovine livers collected at a local slaughter house, approximately two hours after abating the animals. In each liver a vertical hole with 89 mm of diameter was made in the center of it for placing the electrode. A biliar SEMS from Boston Scientific with a diameter of 10 mm and a length of 40 mm was used as electrode. The stent was placed in the liver and it was connected to the RF generator through a BI-PAL endoscopic biopsy. This forceps consists of a 3-pull ring handle, stainless steel cutting jaws, and a coiled shaft. An electrical wired was soldered to the forceps’ shaft, which is electrically connected to the jaws (Fig. 2). This way the electrode can be placed properly, achieving the electrical connection to the RF generator using the forceps’ jaws on the stent. Two RTD temperature sensors were placed at 1 and 2 cm of the electrode. A National Instruments NI USB-9219 acquisition board was used to read these sensors and the data was registered with LabVIEW SignalExpress software. Also, voltage, current intensity and electrical impedance measured by the RF generator were registered. (a) (b) Fig. 2. (a) forceps BI-PAL; (b) detail of the electrical connection. Fig. 3. Experimental setup. To obtain a current distribution around the electrode as symmetric as possible, a return pad was placed at each end of the liver. The RF generator was set to impedance control mode. Fig. 2 presents one of the typical setups used along the experimental test performed. There were performed RF ablation procedures for 5, 10 and 15 minutes, using an output voltage of 25, 50, 75 and 100V. After each procedure, the liver was cross sectioned along a plane containing the stent axis for measuring the dimension of the lesion induced. No histological examination was involved but visual observation. C. Numerical modeling The numerical simulation of the models consists on the analysis of a thermoelectrical coupled field problem. The temperature at each point of the tissue can be expressed by a simplified bioheat equation [14, 15]: c T k T J E t (1) where ρ is the density (kg/m3), c is the specific heat (J/kg·K), T is the temperature (K), k is thermal conductivity (W/m·K), J is the current density (A/m) and E electric field intensity (V/m). The right most term of (1) corresponds to the electrode energy. At RF frequencies the quasi-static approximation is valid and the biological tissue can be considered as a resistive material [17]. A RF voltage is applied between the stent and the return pad and the resulting voltage through the domain obeys Laplace’s equation: V 0 (2) where σ is the electrical conductivity (S/m) and V is the electric potential (V). Fig. 4. Geometrical model used for numerical simulation. A cylindrical model of 100 mm radius and 80 mm height was created for representing the liver tissue. At the center a second cylinder of radius 5 mm and height of 55 mm represents the hollow. The electrode is place at the bottom of the hole and its dimensions are 40 mm length and 10 mm diameter. The stent is made from 24 nitinol wires with 0.25 mm diameter. Each wire is a helix with a pitch of 25 mm. Twelve of the helices are clockwise and the others are counter-clockwise. The whole model have a total of 184 117 tetrahedra. The electrical potential applied to the stent is constant during all RF ablation procedure. Simulations were performed considering voltage values of 25, 50, 75 and 100 V. The bottom and the sides of the larger cylinder are considered at zero volts. The material properties used in our model are presented in TABLE I [18]. The electrical conductivity of the tissue was considered temperature-dependent and simulation was performed considering temperature coefficient of 2%/ºC. When temperature reaches 100ºC, electrical conductivity abruptly drops. By this way it is possible to simulate the electrical insulation verified when gas forms at this temperature value [19]. Element Electrode Hole Tissue TABLE I MATERIAL PROPERTIES USED IN SIMULATION [18] Material ρ [kg/m3] c[J/kg·K]; k[W/m·K] Nitinol 6450 840 18 Air 1.202 1 0.025 Liver 1060 3600 0512 σ[S/m] 1·108 0 σ(T) Dirichlet boundary conditions for the temperature were set to 22ºC for the surfaces away from the active electrode, except for the bottom plane, considered as a thermal insulator surface. The initial temperature of the tissue was set to 25ºC. The models were solved using the solver PARDISO implemented in the finite element software COMSOL Multiphysics (COMSOL, Inc. Burlington, MA, USA). Solving time took about 2.21 hours at 25 V, and 15 hours at 100 V. It was used a computer with a Intel Core 2 Quad CPU @ 2.34Ghz, with 8Gb of RAM, on a 64 bits platform. generator when its 999Ω security threshold is exceeded. This is due to the carbonization of the tissue next to the electrode which induces its electrical insulation. As it would be expected, temperature in the tissue starts to rise as soon as a voltage is applied. This temperature increase will depend on the time of the procedure and on the applied voltage. However, independently of the time considered, no lesion was induced in the tissue for an applied voltage of 25 V. It is shown in (a) (b) Fig. 5 (a) the result of a RF ablation procedure after 15 minutes at 25 V. Inspection shows that no lesion was induced in the tissue next to the electrode. On the other hand, in (a) (b) Fig. 5 (b) is visible the lesion induced in the tissue for an applied voltage of 75 V during 15 minutes. Fig. 6 displays the averaged maximum temperature values measured one and two centimeters away from the stent after 5, 10 and 15 minutes. Considering that cellular damage can be attained in a few minutes for a temperature of 50-52ºC [13, 20], it is possible to verify that the 50ºC threshold will be hardly exceeded at 2 cm from the electrode after 5 minutes for any applied voltage. (a) (b) III. RESULTS A. Experimental results All the data gathered from the measurement of the electrical conductivity in all the samples of liver used was averaged and standard deviation was calculated, thus reaching electrical conductivity value of 0.13±0.06 S/m. (c) Fig. 6. Averaged maximum temperatures obtained 1 and 2 cm away from the electrode after (a) 5 minutes; (b) 10 minutes; and (c) 15 minutes. (a) (b) Fig. 5. (a) Tissue after 15 minutes at an applied voltage of 25 V. It is observed the no damage was induced in the tissue next to the electrode; (b) Tissue damage after 15 minutes at 75 V. In each experimental RF ablation procedure it was possible to observe that the electrical current supplied by the RF power source increased with time, thus increasing the power supplied. This fact consequence of the electrical impedance drop measured from the RF generator. This was not totally verified at 100 V because the RF generator reaches its maximum current output of 2 A. Also, at 100 V the electrical impedance inverts its decrease tendency above 10 minutes, sometimes leading to the shutdown of the power Fig. 7. Cylindrical volume approximation of the lesion induced in the tissue. Numerical and experimental results. After each RF ablation procedure, the liver was cross sectioned and the height and the maximum width of the lesion induced were measured. The volume of the lesion was calculated and approximated to a cylindrical volume. Fig. 7 shows the average volume obtained considering the voltage applied and the time of the procedure (experimental results in solid line). As expected, a bigger lesion is obtained considering larger values of voltage and/or time. For 100 V it is possible to observe that the lesion volume does not significantly change in size after 10 minutes. B. Numerical simulation In Fig. 7 are shown the results obtained by numerical simulation. No results are presented for an applied voltage of 25 V because, even after 15 minutes, the temperature of the tissue never reached 50ºC so no lesion is induced in tissue. The volume of the lesion obtained by analysis of the numerical results almost agrees with measurements made after experimental procedure. However these results diverge for an applied voltage of 100 V, for which the volume obtained with numerical simulation after 5 and 10 minutes is considerable larger than the volume obtained experimentally. After 15 minutes, volumes obtained numerically and experimentally are close. IV. CONCLUSION Due to its good mechanical and biocompatibility characteristics, nitinol SEMS is a popular endoprothesis used for relieving stricture problems in hollow organs due to carcinomas. Besides its mechanical application, SEMS can be regarded as well as potential electrode for performing RF ablation therapy on the tumor. In this work numerical and experimental analyses were performed in order to characterize the lesion volume induced in biological tissue using this kind of tubular electrode. Results show that it is possible to achieve a regular lesion around the electrode. The volume of the lesion obviously depends on the voltage applied and the time of the procedure. Also, the volume of damaged tissue obtained can be considerable large which means precautions have to be taken in order not to injure the duct organ involved. Results obtained through numerical simulations are very close to those obtained with experimentation, providing this way an important tool to predict the dimension that might be obtained and in order to plan a RF ablation procedure. The temperature dependence of thermal properties of the tissue was not considered in this work due to the lack of data on this subject. Thus, this limitation of our model may lead to some inaccurate results, particularly for an applied voltage of 100 V. In this case, the rapidly temperature increase near the electrode may affect significantly the thermal and even the electrical properties of the tissue, which might explain the divergence between numerical and experimental results. However, considering the fragility of the hollow organs that undergo RF ablation procedure and the power that is delivered at 100 V, this voltage certainly will be hardly considered. ACKNOWLEDGMENT The authors would like to thank Dr. Nuno Pinto from Matadouro da Beira Litoral (Aveiro, Portugal) for his support on obtaining the liver samples used in this work. REFERENCES [1] J. Ferlay, et al. (2010, June 5th). GLOBOCAN 2008, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 [Internet]. Available: http://globocan.iarc.fr/ [2] J. Súarez, et al., "Stent or surgery for incurable obstructive colorectal cancer: an individualized decisión," International Journal of Colorectal Disease, vol. 25, pp. 91-96, 2010. [3] M. Burstow, et al., "Outcome of palliative esophageal stenting for malignant dysphagia: a retrospective analysis," Diseases of the Esophagus, vol. 22, pp. 519-525, 2009. [4] D. M. Parkin, et al., "Global Cancer Statistics, 2002," CA Cancer Journal for Clinicians, vol. 55, pp. 74-108, March 1, 2005. [5] M. Gatto, et al., "Cholangiocarcinoma: Update and future perspectives," Digestive and Liver Disease, vol. 42, pp. 253-260, April 2010. [6] M. Gatto and D. Alvaro, "New insights on cholangiocarcinoma," World Journal of Gastrointestinal Oncology, vol. 2, pp. 136-145, March 15 2010. [7] W. H. Paik, et al., "Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach," Gastrointestinal Endoscopy, vol. 69, pp. 55-62, 2009. [8] E. M. Merkle, et al., "Renal Cell Carcinoma: Follow-Up with Magnetic Resonance Imaging After Percutaneous Radiofrequency Ablation," in Methods of Cancer Diagnosis, Therapy, and Prognosis. vol. 6, ed: Springer Netherlands, 2010, pp. 108-113. [9] R.-T. Hoffmann, et al., "Renal cell carcinoma in patients with a solitary kidney after nephrectomy treated with radiofrequency ablation: Mid term results," European Journal of Radiology, vol. 73, pp. 652-656, 2010. [10] L. Crocetti and R. Lencioni, "Radiofrequency ablation of pulmonary tumors (in press)," European Journal of Radiology, 2010. [11] T. Kinoshita, et al., "Radiofrequency ablation as local therapy for early breast carcinomas," Breast Cancer, 2010. [12] D. Volkmer, et al., "The Use of Radiofrequency Ablation in the Treatment of Musculoskeletal Tumors (abstract)," Journal of the American Academy of Orthopaetic Surgeons, vol. 17, pp. 737-743, December 1, 2009. [13] Y. Ni, et al., "A review of the general aspects of radiofrequency ablation," Abdominal Imaging, vol. 30, pp. 381-400, August 2005 2005. [14] C. F. L. Antunes, et al., "Thermal Ablation in Biological Tissue Using Tubular Electrode," presented at the 14th Biennial IEEE Conference on Electromagnetic Field Computation, Chicago, USA, 2010. [15] C. F. L. Antunes, et al., "Effects of the Geometry of a Tubular Electrode on the Temperature Distribution in Biologial Tissue," presented at the 14th Biennial IEEE Conference on Electromagnetic Field Computation, Chicago, USA, 2010. [16] W. M. Telford, et al., "Resistivity Methods," in Applied Geophysics, 2 ed: Cambridge University Press, 1990, pp. 522-539. [17] R. Plonsey and D. Heppner, "Considerations of quasi-stationarity in electrophysiological systems," Bulletin of Mathematical Biology, vol. 29, pp. 657-664, 1967. [18] D. Haemmerich, et al., "Hepatic bipolar radio-frequency ablation between separated multiprong electrodes," IEEE Transactions on Biomedical Engineering, vol. 48, pp. 1145-1152, 2001. [19] D. Haemmerich, et al., "Hepatic radiofrequency ablation with internally cooled probes: effect of coolant temperature on lesion size," IEEE Transactions on Biomedical Engineering, vol. 50, pp. 493-500, April 2003 2003. [20] S. N. Goldberg, "Radiofrequency tumor ablation: principles and techniques," European Journal of Ultrasound, vol. 13, pp. 129-147, 2001.