appendix a - Ashpmedia.org

APPENDIX A
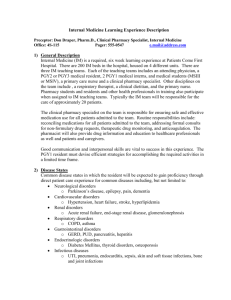
Internal Medicine Learning Activities:
Preceptor: Lauren Instructor, Pharm.D., Clinical Specialist, Internal Medicine
Office: 4S-115
Hours: 7am-3:30pm
Pager: 555-1234
1) General Description
Internal Medicine (IM) is a required, six week learning experience at the University Medical Center. There are
200 IM beds in the hospital, housed on 4 different units. There are three IM teaching teams. Each of the teaching teams includes an attending physician, a PGY2 or PGY3 medical resident, 2 PGY1 medical interns, and medical students (MSIII or MSIV). Other disciplines on the team include the clinical pharmacy specialist or clinical pharmacist, pharmacy students, a respiratory therapist, a clinical dietitian and the primary nurse.
Non-teaching teams are primarily hospitalist-based and pharmacists work regularly with them to identify and resolve medication-related problems for all patients.
The pharmacy resident is responsible for identifying and resolving medication therapy issues for patients and will work toward assuming care of all patients on the unit throughout the learning experience. The resident will provide and document therapeutic drug monitoring services for patients on their team receiving drugs requiring monitoring including, but not limited to, aminoglycosides and vancomycin. Documentation must be completed on the day service was provided. The resident is responsible for providing and documenting education to patients on their team who will be discharged receiving anticoagulation. Education and documentation must be provided no later than the day of discharge. The resident is responsible for completing non-formulary drug consults, within 48 hours of the request.
Good communication and interpersonal skills are vital to success in this experience. The resident must devise efficient strategies for accomplishing the required activities in a limited time frame.
2) Disease States
Common disease states in which the resident will be expected to gain proficiency through literature review, topic discussion, and/or direct patient care experience including, but not limited to:
Neurological disorders o Parkinson’s disease, epilepsy, pain
Cardiovascular disorders o Hypertension, heart failure, stroke, hyperlipidemia
Renal disorders o
Acute renal failure, glomerulonephritis
Respiratory disorders o Asthma, COPD
Gastrointestinal disorders o GERD, PUD, pancreatitis, hepatitis
Endocrinologic disorders o
Diabetes Mellitus, thyroid disorders
Infections diseases o UTI, pneumonia, endocarditis, skin and soft tissue infections, bone and joint infections
3) Goals and Objectives
See Internal Medicine summative evaluation for goals and objectives assigned to this learning experience.
4) Activities
Activity
Accurately gather, organize, and analyze patient specific information on assigned patients prior to pre-rounds with preceptor. For non-teaching services, review profiles to identify medication-related problems to discuss with hospitalist.
Meet with preceptor for pre-rounds @ 8:30 daily for teaching services. For nonteaching services, meet with preceptor for pharmacy rounds @8:30 daily.
Actively participate in IM teaching service team rounds @ 9:30 daily.
For non-teaching services, meet with each hospitalist covering services to resolve issues. (May round with them when feasible.)
Compose an accurate, concise progress note documenting direct patient care activities within time frame to be useful.
Complete consults for non-formulary drugs, recommending formulary, cost-effective alternative drug therapy to health care providers when possible..
Provide and document therapeutic drug monitoring services for patients receiving drugs requiring monitoring including, but not limited to, aminoglycosides and vancomycin.
Identify and report medication events (ADE or medication errors). May be initiated by pharmacy personnel or by other health care professionals.
R2.11.1
R2.11.2
R2.12.1
R2.12.2
R1.5.1
R1.5.2
R1.5.4
R1.5.5
R1.5.6
R2.1.1
R2.4.1
R2.12.2
R5.1.5
Objectives Covered
R2.2.1
R2.4.1
R2.4.2
E7.4.1
R2.4.3
R2.6.1
R2.6.2
R2.8.1
R2.1.1
R2.6.2
R2.8.1
E7.4.1
R2.4.1
R2.6.2
R2.8.1
R2.11.2
R2.12.2
Participate in MUE activities or other outcomes measures for patients on service.
Attend teaching discussion sessions in afternoons when applicable.
Respond to team, patient or family requests for drug information, and document question and response in the DI database on a timely basis.
Provide weekly “mini-in-service” drug information on rounds on topics requested by the team.
R2.4.1
R2.11.2
R2.12.1
R2.10.1
R2.12.1
R2.12.2
E7.4.1
R1.5.1
R1.5.2
R1.5.3
R1.5.4
R1.5.5
R1.5.6
R2.12.1
R1.5.1
R1.5.4
R1.5.5
R1.5.6
R2.1.1
Provide and document education to assigned patients discharged from the hospital on anticoagulants.
Activity Objectives Covered
R1.5.6
R2.11.1
R2.11.2
R2.12.1
R2.12.2
R5.1.1
R5.1.5
R5.1.6
5) Preceptor Interaction
Daily:
Weeks 5-6:
8:30
9:30
1:00 – 2:00
Pre-rounds with resident
Team rounds with resident and team
Preceptor office hour available for topic discussions, reviewing progress notes, patient updates, etc.
Expected progression of resident responsibility on this learning experience:
Day 1: 7:00 Preceptor to review IM learning activities and expectations with resident.
Weeks 1-2: Resident to work up assigned patients and present to preceptor prior to team or pharmacy rounds. Preceptor will attend and participate in rounds or problem resolution (modeling pharmacist’s role on the health care team).
Weeks 3-4: Resident to work up assigned patients and present to preceptor prior to team or pharmacy rounds. Preceptor may be present and participate, coaching the resident to take on more responsibility on the team.
Resident to work up assigned patients and may present to preceptor prior to team or pharmacy rounds. Preceptor may attend and observe the resident’s participation in rounds or on the unit, and/or may expect a summary report from the resident regarding activities and recommendations made by the resident. Preceptor will always be available for questions and may follow patients independently to monitor resident skill development in all aspects of the learning experience (facilitating the resident as the pharmacist on the team).
[The length of time the preceptor spends in each of the phases of learning will depend BOTH on the resident’s progression in the current rotation and where the rotation occurs in the residency program]
6) Evaluation Strategy
ResiTrak will be used for documentation of formal evaluations. For formative evaluations, resident will perform the activity appropriate to the snapshot with the preceptor. Resident and preceptor will then independently complete the snapshot. After both have signed the evaluation, the resident and preceptor will compare and discuss the evaluations. This discussion will provide feedback both on their performance of the activity and the accuracy of the self-assessment.
What type of evaluation
Formative + Formative Self
Formative + Formative Self
Summative
Summative Self-evaluation
Preceptor, Learning Experience Evals
Snapshot Who
TBD
TBD
Preceptor, Resident
Preceptor, Resident
Preceptor, Resident
Resident
Resident
When
End of week 2
End of week 4
End of learning experience
End of learning experience
End of learning experience