Description
advertisement
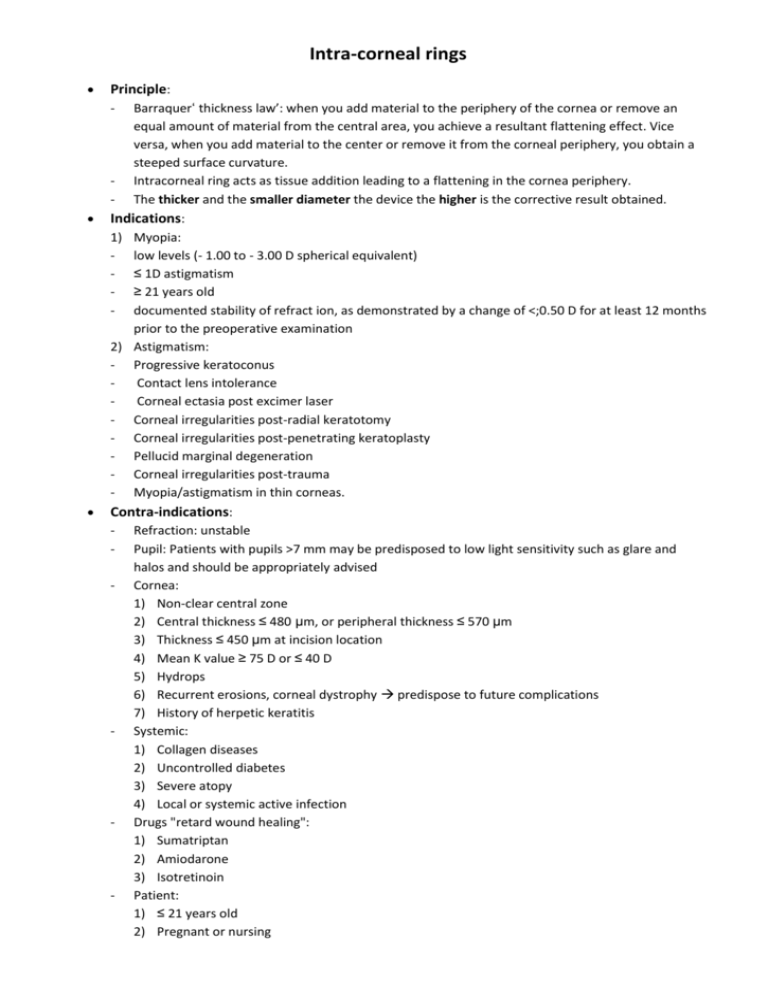
Intra-corneal rings Principle: Barraquer‘ thickness law’: when you add material to the periphery of the cornea or remove an equal amount of material from the central area, you achieve a resultant flattening effect. Vice versa, when you add material to the center or remove it from the corneal periphery, you obtain a steeped surface curvature. - Intracorneal ring acts as tissue addition leading to a flattening in the cornea periphery. - The thicker and the smaller diameter the device the higher is the corrective result obtained. Indications: 1) Myopia: - low levels (- 1.00 to - 3.00 D spherical equivalent) - ≤ 1D astigmatism - ≥ 21 years old - documented stability of refract ion, as demonstrated by a change of <;0.50 D for at least 12 months prior to the preoperative examination 2) Astigmatism: - Progressive keratoconus Contact lens intolerance Corneal ectasia post excimer laser - Corneal irregularities post-radial keratotomy - Corneal irregularities post-penetrating keratoplasty - Pellucid marginal degeneration - Corneal irregularities post-trauma - Myopia/astigmatism in thin corneas. - Contra-indications: - - - - Refraction: unstable Pupil: Patients with pupils >7 mm may be predisposed to low light sensitivity such as glare and halos and should be appropriately advised Cornea: 1) Non-clear central zone 2) Central thickness ≤ 480 µm, or peripheral thickness ≤ 570 µm 3) Thickness ≤ 450 µm at incision location 4) Mean K value ≥ 75 D or ≤ 40 D 5) Hydrops 6) Recurrent erosions, corneal dystrophy predispose to future complications 7) History of herpetic keratitis Systemic: 1) Collagen diseases 2) Uncontrolled diabetes 3) Severe atopy 4) Local or systemic active infection Drugs "retard wound healing": 1) Sumatriptan 2) Amiodarone 3) Isotretinoin Patient: 1) ≤ 21 years old 2) Pregnant or nursing Rings used: Material External diameter Internal diameter Arc length Thickness Intrastromal Corneal Ring segments "INTACS" conventional INTACS SK PMMA 8.1 mm 7.4 mm 6.77 mm 150̊ 0.25 - 0.45 mm "0.025 increment" 6 mm Cross section Refractive effect hexagonal -1 to -4 D 150̊ 0.40 mm (for steep K-value 57-62 D and cylinder > 5 D) 0.45 mm (for steep K-value > 62 D and cylinder > 5 D) oval Ferrara ring segments Keraring segments PMMA CQ-acrylic 5.6 mm 5.6 mm 4.4 mm 4.4 mm 160̊ 0.15 – 0.35 mm "0.025 mm increment" 90 - 210̊ 0.15 – 0.35 mm "0.05 mm increment" triangular triangular (6.0 mm for myopia up to 7.00 D, 5.0 mm for higher degrees of myopia) NB1: Both, Ferrara and Keraring segments, are triangular. The Prismatic effect, created by the triangular shape of the ring intending to eliminate the halo phenomena and obfuscation, would be expected due to the orthesis reduced diameter. NB2: - Use symmetric segments when the cone on the posterior float is within the central 3-5 mm optical zone and the sphere power > cylinder power on the manifest refraction notated in positive cylinder. - Use the asymmetric segments when the cone on the posterior float is located outside the 3 mm geometric center and the cylinder power,> the sphere power on the manifest refraction notated in positive cylinder. Pre-operative evaluation: 1) 2) 3) 4) 5) 6) 7) 8) 9) Corneal topography, posterior float Pachymetry Spherocylndrical power Manifest refractive spherical equivalent (MRSE) Best corrected visual acuity (BCVA) with spectacles Uncorrected visual acuity (UCVA) Keratometric (K) values Slit-lamp examination of the anterior segment Contact lens tolerance. Technique: - Anesthesia: topical with oral sedation Mechanical method: 1) Geometric center of the cornea is identified using the 11 mm zone marker and the center is marked using a Sinskey hook 2) The ‘incision mark’ of the procedure marker is aligned 1 mm from the limbus, at the 9 o’clock position for right eyes and at the 3 o’clock position for left eyes. 3) A superior-temporal radial 1.0 mm long incision is created to approximately 70% of the cornea thickness on the steepest axis of the topographic map NB: To identify the proposed incision location, draw a “blue” line across the center of the posterior view in the direction the cone is displaced. Then, draw a “red” line perpendicular to the “blue" line making a plus sign or “X” over the posterior view. The blue line represents the flat meridian,(where the Intacs will be placed),and the red line represents the steep meridian,(where the incision will be placed). 4) The intrastromal tunnels are initiated using a pocketing hook (formerly a stromal spreader) 5) A glide blade is introduced into the incision to assess incision length and to verify the adequacy of the pocket - 6) The vacuum centering guide (VCG) is placed along with the procedure marker on the corneal surface. The VCG and procedure marker are aligned with the geometric center of the cornea. 7) The KV 2000 vacuum system is started on the low setting and ramped up to the high setting 8) The Counter clockwise "CCW" & the Clockwise "CW" dissectors (corneal separators) are used to create the intrastromal tunnels in the desired directions and the Intacs inserts are implanted into the tunnels. 9) One or two 10-0 nylon sutures or tissue glue may be used to close the radial incision at the corneal surface Femtolaser method: 1) The disposable glass lens applanates the cornea to fixate the eye and helps to maintain the precise distance from the laser head to focal point 2) Parameters: pulse duration 600 femtoseconds, the inner to outer diameter of the Intacs tunnel set from 6.7 to 8.2 mm. Spot size is 1 µm and the energy is 6 µ J 3) After the original incision is reopened with Sinskey hooks, the Intacs segment is slightly rolled superiorly to achieve the proper entering angle with the wound. 4) The leading edge of the segment is inserted into the pocket 5) Once half of the segment is in the tunnel, the grasp of the forceps is released and the remainder of the segment is nudged into the tunnel with a Sinskey hook. Post-operative care: After surgery, patients receive antibiotic and corticosteroid eyedrops three times daily for 2 weeks. Patients are instructed not to rub their eyes following surgery. A plastic shield is recommended at night for several weeks to avoid eye rubbing. Complications: 1) epithelial defects at the keratotomy site 2) anterior and posterior perforations while creating the channel 3) extension of the incision toward the central visual axis or toward the limbus 4) shallow placement and/or uneven placement of the Intacs segments 5) infectious keratitis with the introduction of the epithelial cells into the channel during the channel dissection 6) asymmetric placement 7) persisting incisional gap 8) decentration, and stromal thinning 9) corneal stromal edema around the incision and channel from surgical manipulation 10) under- or over-correction 11) ↓ corneal sensitivity 12) Neovascularization at incision site - - NB: One or two Intacs segments: when the keratoconus is peripheral (similar to pellucid marginal degeneration), not central, it may be preferable to place a single segment instead of 2 segments. However some doesn't recommend single segment use. LASIK after Intacs: after ring segments have been removed from patients whose vision did not improve to a satisfactory level (e.g. due to undercorrection or induced astigmatism), LASIK has been performed with good success. The flap is created in a plane superficial to the previous ring segment channel.