Menopause - Cases
advertisement
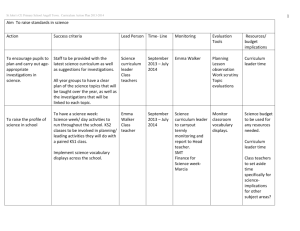
MENOPAUSE: PATIENT CASES 1. A healthy 50 year-old obese woman is currently going through menopause. She is having hot flashes (~8 per day) and night sweats (~1 per night). Her girlfriend recently started hormone therapy and suggested she try it. She has no significant medical history, surgical history, or family history. Her physician is asking you about the efficacy and safety of using hormone therapy in this woman. What recommendation would you provide at this time? Be specific. 2. A healthy 52 year-old woman is currently going through menopause. She is having hot flashes (~10 per day) and night sweats (~2 per night). She will not consider EPT and would like to know about other options and how long she will “suffer”. Her other medications include a multivitamin and ibuprofen prn for headache. What information and/or recommendations would you provide at this time? 3. A 61-year-old postmenopausal woman, presents to her physician suffering from unbearable vaginal dryness, itching, and pain during intercourse -- symptoms that were not as severe during her last checkup 1 year ago and at that time caused no distress. She reached menopause spontaneously at age 50 and has experienced no menopauserelated symptoms, including hot flashes. She does not have a personal or family history of cardiovascular disease, breast cancer, or uterine cancer. A dual-energy x-ray absorptiometry test to measure bone density 4 years ago was within normal ranges for her age. Pelvic examination is unremarkable except for fragile vaginal mucosa characterized by pallor, decreased elasticity, disappearance of rugae, and petechiae. Vaginal secretions are scant and odorless. She has no complaints or signs that could indicate a vaginal infection. Develop and assessment and plan for her vaginal symptoms. 4. A returning 45 year-old patient complains of depression, hot flashes, and difficulty sleeping for the past 6 or 7 months. Relevant medical history includes migraine without aura at age 37 years and normal Pap smear in last 12 months. She had a levonorgestrel IUD placed at 43 years, has 2 children, and has been married for 12 years. She does not smoke and drinks 1-2 alcoholic beverages on weekend days. 5. CC: “I have been having hot flashes for the past few months, and I just can’t take it anymore.” HPI: Emma Peterson is a 50-year-old woman who reports experiencing 2-3 hot flashes per day, occasionally associated with insomnia. She also states she is awakened from sleep, soaked by night sweats, about 2-3 times per week needing to change her pajamas and bed linens. Her symptoms began about 6 months ago, and over that time, they have worsened to the point where they have become very bothersome. She states that her mother was prescribed hormones for this, but she is hesitant to take them because she has heard that the medication may not be safe. PMH: Depression; GERD; HTN; hypothyroidism FH: Mother died of stroke at age 67; father died of lung cancer at age 62. Has one brother, 52, and one sister 48 who are alive and well, but both with HTN. SH: Married, mother of 2 healthy daughters ages 21 and 25. She is a RN in a neighboring physician’s office. She walks on her treadmill 3 times/week and follows a dieticiandesigned low-cholesterol diet. She does not smoke and occasionally drinks a glass or two of red wine with dinner. Meds: Hydrochlorothiazide 25 mg by mouth once daily; omeprazole 20 mg by mouth once daily; paroxetine 20 mg by mouth once daily; levothyroxine 75 mcg by mouth once daily. All: NKDA ROS: (+) hot flashes, night sweats and insomnia, vaginal dryness. (-) weight gain, constipation. LMP was 8 months ago. Physical Exam Gen: WDWN female in NAD VS – BP 128/78, P 78, RR 15, Wt 76 kg, Ht 5’6” Skin – warm, dry, no lesions HEENT, Neck/lymph nodes, lungs, CV, Abd – all normal findings Breasts – equal in size without nodularity or masses, supple, nontender Genit/Rect – Pelvic exam normal except (+) mucosal atrophy; stool guaiac (-) MS/Ext/Neuro – normal, expected findings Labs: TSH 2.46 mIU/L; total cholesterol 205 mg/dL; LDL 116 mg/dL; HDL 545mg/dL; triglycerides 220 mg/dL; serum creatinine 0.7 mg/dL; FSH 42 IU/L Other: Pap smear and mammogram normal Assessment: 50-year-old, symptomatic postmenopausal woman exploring treatment options. Questions a. What are the presenting signs and symptoms of menopause being experienced by Emma? b. What are the goals of therapy for Emma’s menopausal symptoms? c. What non-drug therapies may be recommended for Emma? d. What drug, dosage form, dose, schedule and duration would you recommend for Emma and why? e. What would you recommend for Emma’s monitoring plan? f. What if.... one of Emma’s sisters had ER+ breast cancer? Emma had a calculated LDL of >160 mg/dL and uncontrolled hypertension? 6. Theresa Hart is a 53-year-old who presents complaining of dyspareunia and reduced libido. As a result of this, she and her husband have not had sexual intercourse in more than 4 months. Prior to menopause (her LMP was about 13 months ago), TH describes their sex life as ‘vibrant’. She is quite distressed by this and is seeking your assistance. She is an otherwise healthy 54 yo female. She does note the occurrence of rare (< 1 time/week) vasomotor symptoms. Her mother is alive and well (has HTN) at age 78; her father died from an MI at age 74. She has 2 older sisters (ages 55 and 56); both alive and well. Questions a. What therapeutic options exist for Theresa? b. What treatment option would you recommend (drug, dose, route, etc.) for Theresa? c. How would you monitor the treatment plan for efficacy and side effects?