ENDOCRINE SYSTEM Revised 2013 from Saunders Intro. To Med
advertisement
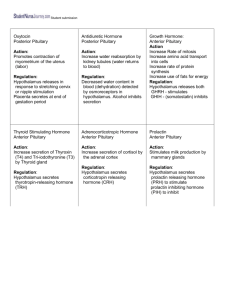
ENDOCRINE SYSTEM Revised 2013 from Saunders Intro. To Med/Surg Nursing, 5th Ed. Chapter 44 Pituitary and Adrenal Disorders Learning Objectives Identify data to be collected for the nursing assessment of adrenal and pituitary function. Describe the tests and procedures used to diagnose disorders of the adrenal and pituitary glands. Describe the pathophysiology and medical treatment of adrenocortical insufficiency, excess adrenocortical hormones, hypopituitarism, diabetes insipidus, and pituitary tumors. Assist in developing nursing care plans for patients with selected disorders of the adrenal and pituitary glands. Hormone Functions and Regulation Released in response to body’s needs Responsible for reproduction, fluid and electrolyte balance, host defenses, responses to stress and injury, energy metabolism, and growth and development Endocrine system: maintain homeostasis Maintenance of physiologic stability despite constant changes in the environment Hormone Functions and Regulation Feedback mechanisms Controls regulation of endocrine activity by either stimulating or inhibiting hormone synthesis and secretion Triggered by blood levels of specific substances May be positive or negative The Pituitary Gland Anatomy and Physiology Weighs approximately 0.6 g; located in the sella turcica, a small indentation in the sphenoid bone at the base of the brain Connected to the hypothalamus by the infundibular (hypophyseal) stalk Small and oval; diameter of about 1 cm Anatomy and Physiology Anterior lobe Larger of the two lobes: accounts for 70% to 80% of the gland’s weight Called the adenohypophysis Secretes • Growth hormone (GH), or somatotropic hormone • Adrenocorticotropic hormone (ACTH) • Thyroid-stimulating hormone or thyrotropic hormone • Follicle-stimulating hormone • Luteinizing hormone • Prolactin, or lactogenic hormone • Melanocyte-stimulating hormone Anatomy and Physiology cont’d Posterior lobe The smaller lobe Also called the neurohypophysis Secretes • Antidiuretic hormone (ADH), or vasopressin • Oxytocin Health History PUT YOUR THINKING CAPS ON AND CRITICALLY THINK.. QWhat are some problems R/T pituitary function that may bring a patient to seek medical care? Health History cont’d PUT YOUR THINKING CAPS ON AND CRITICALLY THINK… Q When doing your Review of Systems what should you ask about the patient’s general health state? Diagnostic Tests and Procedures Radiographic studies Conventional radiographs Computed tomographic (CT) scans MRI Cerebral angiography Laboratory studies Radioimmunoassay Enzyme-linked immunosorbent assay (ELISA) Hormone reserve activity also can be measured using a number of “suppression” or “stimulation” tests Disorders of the Pituitary Gland Hyperpituitarism Gigantism or Acromegly Cause Pathologic state caused by excess production of one or more of the anterior pituitary hormones Common factor is presence of a pituitary adenoma Growth hormone and prolactin often in excess • Overproduction leads to gigantism or acromegaly • Overproduction of prolactin causes prolactemia Hyperpituitarism cont’d Medical diagnosis Radiographic studies • CT scans using a water-soluble dye • MRI Laboratory studies • Anterior pituitary hormone levels, esp. GH levels • Glucose Tolerance Test Hyperpituitarism cont’d Medical treatment Drug therapy • Many drugs used; Somatostatin analogs, dopamine agonists, GH receptor antagonists, but Sandostatin is the most common drug Radiation Surgical management • Hypophysectomy: surgical removal of the adenoma or of the pituitary. This method is the treatment of choice. Post Op Nursing Care Assessment • Neurologic status and vision must be monitored closely with particular attention to level of consciousness, pupil size and equality, and vital signs • Strict Intake and output WHY? • Inspect nasal packing WHY ? • Signs and symptoms of infection Nursing Diagnosis and related Interventions Critically Think Now… What are your nursing interventions related to these Nursing Diagnosis? • Anxiety • Acute Pain and Impaired Oral Mucous Membrane • Risk for Injury • Risk for Infection Hypopituitarism Dwarfism Inadequate secretion of growth hormone during preadolescence Attainment of a maximum height 40% below normal Causes hereditary or related to damage to the anterior portion of the pituitary gland Panhypopituitarism Growth has been completed and some pathologic process impairs the function of the pituitary Hypopituitarism Signs and symptoms Depends on the stage of life which hormones are deficient Dwarfism • Occurs early; person as short as 36 inches but with proportional physical characteristics • Often have delayed or absent sexual maturation • Accelerated pattern of aging, thus shorter life span Hypopituitarism cont’d Signs and symptoms Panhypopituitarism ( growth is completed but some pathologic process impairs the function of the pituitary gland ) • Simmonds cachexia develops: Muscle and organ wasting and disruptions of both digestion and metabolism • Absence of ACTH affects ability to cope with stress • Thyroid-stimulating hormone is depleted • Decreased pigmentation of the skin • Gonads may become atrophied Hypopituitarism cont’d Medical diagnosis Health history Physical examinationwith dwarfism findings are diagnostic X-rays and CT scans to detect tumors Cerebral angiography Serum levels of pituitary hormones Medical and surgical treatment Deficient hormones are replaced as needed If caused by tumor, surgery, or radiation Important Interventions Education important: disturbances in body image, sexual function, nutritional status, and fluid balance can be improved if patient follows the prescribed therapy Acknowledge patient’s feelings and encourage expression of concerns; refer to a mental health counselor if patient has difficulty dealing with the effects of the disease Posterior Pituitary Disorders Characterized by deficient or excess amounts of ADH ( Anti diuretic hormone ) or “vasopressin” ADH helps to maintain fluid balance ^ ADH levels low urine output or fluid retention Low ADH levels more water passes through the kidneys than normal Diabetes Insipidus Results from underproduction of ADH Char by large volumes of dilute urine (polyuria) Urine will be very dilute Signs & Symptoms Copious amounts of very dilute urine, may exceed 30 liters/day Dehydration Thirst Hypotension, tachycardia, dizziness, weakness and fainting Medical Diagnosis and Trmt Diagnosis Based on health history, PE, 24 hr. urine output of > 4 L Treatment IV fluid volume replacement and vasopressors are required to maintain BP. Most common drug is DDAVP (Desmopressin) Nursing Interventions I&O IV fluid replacement Fall precautions VS Mon. thirst & weight Compensate for fluid loss Monitor for dizziness, weakness Monitor for palpitations Syndrome of Inappropriate Antidiuretic Hormone (SIADH) Cause Water imbalance related to an increase in ADH synthesis or secretion, or both Pathophysiology When ADH is elevated despite normal or low serum osmolality, kidneys retain excessive water Plasma volume expands, causing the blood pressure to rise. Body sodium is diluted (hyponatremia), and water intoxication develops Syndrome of Inappropriate Antidiuretic Hormone cont’d Signs and symptoms Weakness, muscle cramps or twitching, anorexia, nausea, diarrhea, irritability, headache, and weight gain without edema When the central nervous system is affected by water intoxication, the level of consciousness deteriorates Patient may have seizures or lapse into a coma Syndrome of Inappropriate Antidiuretic Hormone cont’d Medical diagnosis Laboratory tests of serum and urine electrolytes and osmolality Urine osmolality is high ( very concentrated ) and serum osmolality is low ( very dilute ) Radiographic studies of brain and lungs may be done to try to detect causative factors Medical Treatment Intended to correct the cause There are several approaches to therapy ( all are patient sensitive ) The focus is to promote elimination of excess water & keep Na & K+ levels balanced Lithium Carbonate or demeclocycline (blocks the effect of ADH) Strict fluid restrictions to 800-1000ml/day with a high Na diet ( ? cardiac patients ) Medical Treatment ( cont’d ) Hypertonic NS (3%) pulls Na out of the intracellular space and into the extracellular space thus ^ serum Na levels. Nursing Diagnosis and related Interventions Critically Think Now… What are your nursing interventions related to these Nursing Diagnosis? Risk for Injury Excess Fluid Volume Ineffective Therapeutic Regimen Management The Adrenal Glands Anatomy and Physiology A pair of small, highly vascularized triangular-shaped organs Located in the retroperitoneal cavity on the superior poles of each kidney, lateral to the lower thoracic and upper lumbar vertebrae Two parts: an outer portion called the cortex and an inner portion called the medulla Anatomy and Physiology cont’d Cortex secretes steroid hormones (mineralocorticoids & glucocorticoids ) also androgens and estrogen Medulla secretes epinephrine & norepinephrine Aldosterone Most important mineralocorticoid Regulates Na and K + Keeps blood volume balanced Renin, Angiotensin & Aldosterone Mineralocorticoids Are Key in maintaining adequate extracellular fluid volume Renin, angiotensin, and aldosterone Renin release is stimulated by decrease in extracellular fluid volume Renin acts on plasma proteins to release angiotensin I, which is catalyzed in the lung to angiotensin II Angiotensin II stimulates the secretion of aldosterone, which results in sodium and water retention Cortisol Most important glucocorticoid Has anti-inflammatory response Immune response Controls emotional state ACTH ADRENAL CORTICOIDTROPIC HORMONE Sent to adrenals by Pituitary Stimulates production of adrenal Serum ACTH levels are checked to see if Pituitary gland is sending messages to the adrenals Health History Critically think about these 3 areas? Present illness Past medical history Review of Systems & PE Adrenal Hypofunction/Addison’s Disease Most often caused by: • autoimmune disease process affecting the adrenal glands; results in deficiencies of cortisol and aldosterone • Occurs in 1 per 100,000 people • Decrease of ACTH production ( is a secondary cause ) • TB and fungal infections • Also abrupt withdrawal of exogenous steroids ( could cause Addison’s disease ) Signs & Symptoms Weakness, lethargy and malaise Skin hyperpigmentation (looks sun tanned ) Light headedness upon rising Due to hypovolemia (orthostatic hypotension) Have pt. move slowly, help getting out of bed Decrease tolerance to minor stress Variety of GI complaints Salt craving (due to hyponatremia ) Adrenal Hypofunction cont’d Acute adrenal crisis (Addisonian crisis) A life-threatening emergency bec. Of fluid and electrolyte imbalances Cause from abrupt withdrawal of steroid therapy Stress ( infections, illness, trauma, emotional disturbances ) Other precipitating factors are adrenal surgery, or pituitary destruction Adrenal Hypofunction cont’d Acute adrenal crisis (Addisonian crisis) Manifestations include symptoms of mineralocorticoid and glucocorticoid deficiency but are more severe: hypotension, tachycardia, dehydration, confusion, hyponatremia, hyperkalemia, hypercalcemia, and hypoglycemia If untreated, fluid and electrolyte imbalances can lead to circulatory collapse, cardiac arrhythmias, cardiac arrest, coma, and death Adrenal Hypofunction cont’d Medical diagnosis is made by: Clinical signs and symptoms discussed Variety of lab findings • Low serum cortisol level, low glucose, hyponatremia, hyperkalemia • Plasma ACTH concentration (ACTH stimulation test ) • If high Adrenals at fault; if low pituitary at fault EKG X-rays Adrenal Hypofunction cont’d Medical treatment Replacement therapy with glucocorticoids and mineralocorticoids Hydrocortisone is drug of choice because it contains both gluco and mineralocorticoids Nursing Dx & related Interventions Critically thinking time… put those caps on and FOCUS…. Risk for Injury Imbalanced Nutrition: Less Than Body Requirements Patient teaching on…..? Case Study A 39-year-old construction worker who complains of decreased energy, impotence, and abdominal pain is being tested for Addison disease. What data should the nurse collect when obtaining the patient’s health history? What physiologic changes in the body result in the abnormal symptoms of Addison disease? Adrenal Hypersecretion (Cushing’s Syndrome) Cause Production of excess amounts of corticosteroids, particularly glucocorticoid Overproduction: endogenous (internal) as well as exogenous (external) • Endogenous causes related to a tumor/neoplasm • Exogenous causprolonged administration of high doses of corticosteroids Adrenal Hypersecretion (Cushing Syndrome): Pathophysiology Excess levels of circulating corticosteroids will affect every body system Produces marked changes in personal appearance, including obesity, facial redness, hirsutism, menstrual disorders, hypertension of varying degrees, muscle wasting of extremities Additionally delayed wound healing, insomnia, irrational behavior, and mood disturbances such as irritability and anxiety Adrenal Hypersecretion (Cushing Syndrome): Clinical S/S Hallmark Findings that lead to diagnosis Truncal obesity Protein wasting, causing arms & legs to be thin Facial fullness, often called a “moon face” Purple striae on the abdomen, breasts, buttocks, or thighs; very thin friable skin Osteoporosis Hypokalemia of uncertain cause Irritability or mood swings ^ BP and easy bruising Adrenal Hypersecretion (Cushing Syndrome) Medical diagnosis Physical s/s Laboratory studies • 24-hour urine collection for free cortisol • Low-dose dexamethasone suppression test ( Should show drop of cortisol & steroid levels when compared to baseline; if not, then Cushing’s is considered ) Radiographic studies • CT scan and MRI if tumor is suspected as cause Adrenal Hypersecretion (Cushing Syndrome) cont’d Medical treatment Drug therapy • Mitotane (Lysodren), ketoconazole (Nizoral), aminoglutethimide (Cytadren), and metyrapone (Metopirone) Radiation • Administered externally or internally Surgical management Considerations…. Drug Therapy Lysodren There is a risk of acute adrenal crisis when patients are on drugs that suppress adrenal function. Radiation is not always effective; requires a long period of treatment and can destroy healthy tissue. Review Slide ! Addison’s Disease Lab values are Hypoglycemia, hyponatremia and hyperkalemia Cushing’s Syndrome Lab values are Hyperglycemia, hypernatremia and hypokalemia CRITICALLY THINK NOW ! What are your nursing interventions for this patient and why? Look closely at this slide. What do you think the relevance is between it and what you’ve learned thus far pertaining to the Endocrine System??? Are things always as they appear? Is it wise to jump to conclusions without looking closely at the facts and critically thinking? You’re half way there to finishing the Endocrine System. Keep your FOCUS and turn to Chapter 45 for Thyroid and Parathyroid Disorders