3313 example of Clinical Planning Sheet
advertisement
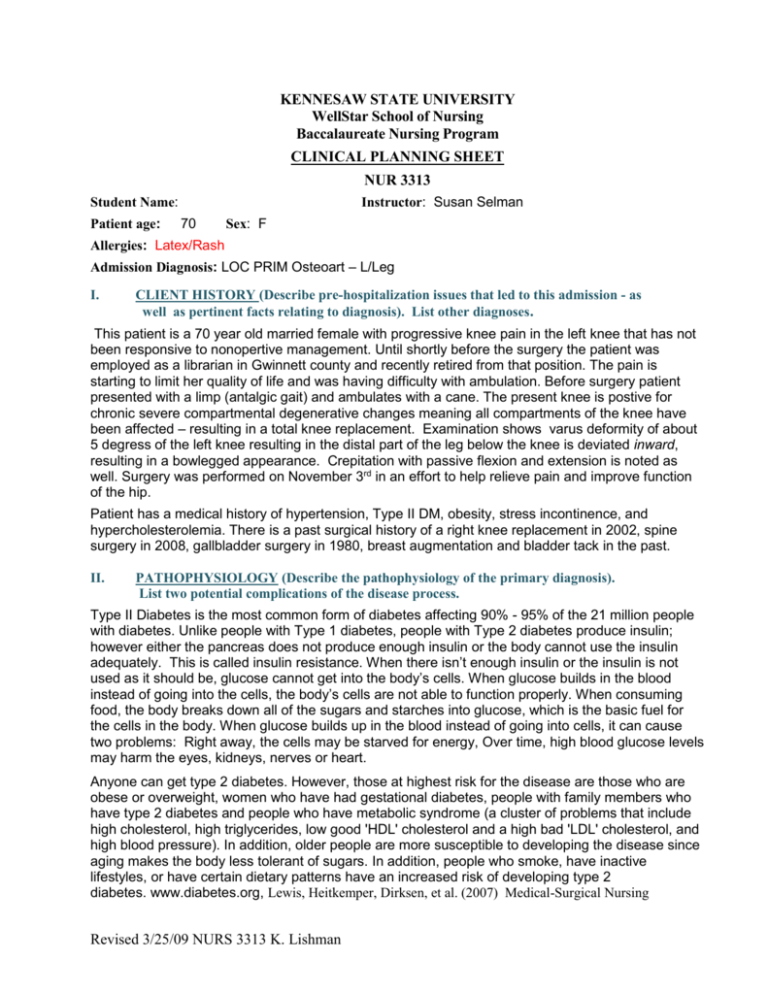
KENNESAW STATE UNIVERSITY WellStar School of Nursing Baccalaureate Nursing Program CLINICAL PLANNING SHEET NUR 3313 Instructor: Susan Selman Student Name: Patient age: 70 Sex: F Allergies: Latex/Rash Admission Diagnosis: LOC PRIM Osteoart – L/Leg I. CLIENT HISTORY (Describe pre-hospitalization issues that led to this admission - as well as pertinent facts relating to diagnosis). List other diagnoses. This patient is a 70 year old married female with progressive knee pain in the left knee that has not been responsive to nonopertive management. Until shortly before the surgery the patient was employed as a librarian in Gwinnett county and recently retired from that position. The pain is starting to limit her quality of life and was having difficulty with ambulation. Before surgery patient presented with a limp (antalgic gait) and ambulates with a cane. The present knee is postive for chronic severe compartmental degenerative changes meaning all compartments of the knee have been affected – resulting in a total knee replacement. Examination shows varus deformity of about 5 degress of the left knee resulting in the distal part of the leg below the knee is deviated inward, resulting in a bowlegged appearance. Crepitation with passive flexion and extension is noted as well. Surgery was performed on November 3rd in an effort to help relieve pain and improve function of the hip. Patient has a medical history of hypertension, Type II DM, obesity, stress incontinence, and hypercholesterolemia. There is a past surgical history of a right knee replacement in 2002, spine surgery in 2008, gallbladder surgery in 1980, breast augmentation and bladder tack in the past. II. PATHOPHYSIOLOGY (Describe the pathophysiology of the primary diagnosis). List two potential complications of the disease process. Type II Diabetes is the most common form of diabetes affecting 90% - 95% of the 21 million people with diabetes. Unlike people with Type 1 diabetes, people with Type 2 diabetes produce insulin; however either the pancreas does not produce enough insulin or the body cannot use the insulin adequately. This is called insulin resistance. When there isn’t enough insulin or the insulin is not used as it should be, glucose cannot get into the body’s cells. When glucose builds in the blood instead of going into the cells, the body’s cells are not able to function properly. When consuming food, the body breaks down all of the sugars and starches into glucose, which is the basic fuel for the cells in the body. When glucose builds up in the blood instead of going into cells, it can cause two problems: Right away, the cells may be starved for energy, Over time, high blood glucose levels may harm the eyes, kidneys, nerves or heart. Anyone can get type 2 diabetes. However, those at highest risk for the disease are those who are obese or overweight, women who have had gestational diabetes, people with family members who have type 2 diabetes and people who have metabolic syndrome (a cluster of problems that include high cholesterol, high triglycerides, low good 'HDL' cholesterol and a high bad 'LDL' cholesterol, and high blood pressure). In addition, older people are more susceptible to developing the disease since aging makes the body less tolerant of sugars. In addition, people who smoke, have inactive lifestyles, or have certain dietary patterns have an increased risk of developing type 2 diabetes. www.diabetes.org, Lewis, Heitkemper, Dirksen, et al. (2007) Medical-Surgical Nursing Revised 3/25/09 NURS 3313 K. Lishman III. PROCEDURES (Current/recent surgical/other invasive done during this admission and describe rationale for procedures). e.g. surgeries, cardiac catheterization, etc. The severe destructive deterioration of the knee joint indicated for total knee arthroplasty. Patient had left Total Knee Replacement surgical on 11/3/2009. The patient received spinal anesthesia. TheOsteophytes and soft tissues were debrided and removed as appropriate. The surgery involves exposure of the front of the knee, with detachment of part of the quadriceps muscle (vastus medialis) from the patella. The patella is displaced to one side of the joint allowing exposure of the distal end of the femur and the proximal end of the tibia. The ends of these bones are then accurately cut to shape using cutting guides oriented to the long axis of the bones. The cartilages and the anterior cruciate ligament are removed; the posterior cruciate ligament may also be removed but the tibial and fibular collateral ligaments are preserved. Metal components are then impacted onto the bone or fixed using polymethylmethacrylate (PMMA) cement. A round ended implant is used for the femur, mimicking the natural shape of the bone. On the tibia the component is flat, although it often has a stem which goes down inside the bone for further stability. A flattened or slightly dished high density polyethylene surface is then inserted onto the tibial component so that the weight is transferred metal to plastic not metal to metal. During the operation any deformities must be corrected, and the ligaments balanced so that the knee has a good range of movement and is stable. In some cases the articular surface of the patella is also removed and replaced by a polyethylene button cemented to the posterior surface of the patella. In other cases, the patella is replaced unaltered. www.nlm.nih.gov IV. CURRENT/RECENT DIAGNOSTIC TESTS/PROCEDURES (Dates and results: CXR, 12-lead ECG, scans. 12 lead ECG show normal, vital signs show normal V. LIST THREE NURSING DIAGNOSIS FOR THIS CLIENT IN ORDER OF IMPORTANCE OR PRIORITY. EXPLAIN THE RATIONALE FOR THE PRIORITY. 1. Acute Pain related to trauma caused by surgery a. Assessment of pain, noting pain level (0 - 10) b. Administer medication on a regular schedule c. Monitor effects of analgesic Goal: maintain pain control 2. Risk for Infection related to invasive procedure a. Monitor for signs and symptoms infection (fever, joint swelling, redness, warmth), neurovascular compromise and compare finding with the unaffected limb (diminished pedal pulses; capillary refill. cool and pale extremity) b. Monitor WBC count c. Monitor vital signs, increased pulse, increased respirations, decreased oxygen saturation. Goal: Patient will remain free of infection as evidenced by normal vital signs and absence of purulent drainage 3. Impaired Physical Mobility a. Encourage ROM will all unaffected extremities b. Maintain proper position in CPM machine c. Assist patient in position changes and monitor for skin breakdown Goal: Patient maintains strength in unaffected joints Revised 3/25/09 NURS 3313 K. Lishman CURRENT NURSING INTERVENTIONS (check, describe or quantify): Explain why the intervention is appropriate/necessary for your client. What other intervations did you do based on the clients pathophysiology, history, and current condition? Why? ____ Nasogastric Suction ____ Pacemaker Wires/Monitor ____ Feeding Tube (NG/GT/JT) size _____ suction _____ ____ Baseline Vital Signs _____________ ____ Glucose check times _____/_____ ____ Neuro Checks ____ Colostomy/Ileostomy ____ I & O ____ Foley Catheter ____ Dressing Change (describe) ______________________________ ____ Nephrostomy tubes/stents/supra pubic tubes ____ Mobility/ADL Level ____ Chest Tubes ________/________ ____ ROM Exercises ____ O2 ____ TED Hose ____ Oximetry(pulse oximetry) ____ Special Bed/Mattress (describe) ______________________________ ____ CPT ____ Restraints ____ Traheostomy _________________ ____ Drains - Constavac, JP, ________ Intercranial, etc. ____ Central Line(s). What type?_____ What's infusing?______________ ____ Precautions (what type?) ______________________________ ____ Other ______________________________ ______________________________ ____ Peripheral Line(s): What's _____ infusing?________________ ____ Saline/Heparing Lock location ____________________ ____ Casts ____ Traction ______________________ Revised 3/25/09 NURS 3313 K. Lishman VII. LABORATORY RESULTS (Remember to look at "trends in labs values". Circle abnormal value and state why this lab is abnormal specific to your patient) [dx, hx, meds, etc.] DATES: 11/4/2009 PURPOSE OF LAB TESTS TIMES: 03:48 Lab Glucose BUN Normal 65-105 7-21 Creatinine 0.5-1.04 WBC 4.8-10.8 RBC 4.20-5.40 Reasons for Abnormal ↑ 149 ↑ 23 ↑ 1.12 ↑ 12.3 ↓ 3.08 Hgb 12.0-16.0 ↓ 9.9 Hct 37.0-47.0 ↓ 29.3 Revised 3/25/09 NURS 3313 K. Lishman Determined in new patients to monitor closely the insuline dosage to be administered / or if need Measures amount of urea nitrogen in the blood. In conjunction with creatinine test is measurement of kidney and liver function Measure amount of creatinine in the blood. Part of measurement of renal function Measure total number of WBC in venous blood, function is to fight infection and react to foreign bodies Counts the number of circulating red bloods, routinely performed as part of complete blood count.Within each RBC are molecules of hemoglobin that permit the transpot and exhange of oxygen to the tissues Measure as part of complete blood count, Hgb serves as a vehicle of oxygen and carbon disoxide transport. Measure of the percentage of total blood volume that is made up by the red blood cells Stress can cause increased serum glucose levels Hypovolemia, dehydration can cause increased level (possiblity r/t NPO of surgery) Dehydration can cause increased level, in addition to urinary tract obstruction Increased level can indicate infection, stress, inflammation Decreased level may indicate hemorrage, anemia Decreased levels indicate anemia Decreased levels indicate anemia VIII. Medications: List all medications, including IV, IM, PO, SC and prn. FOR ALL IV PIGGYBACKS, please calculate flow rate and know if the medication is compatible with the rest of the IV drugs/ IV fluids which are listed for your patient. FOR IV PUSH DRUGS, please know push rate, compatibility with other IV meds/IV fluids and if they need to be diluted and with what. Medication (Brand and generic as listed on patient profile), dose, route and frequency. If IV, include info. from directions above Classification (general and pharmacologic) Nursing Implications (crossover allergies, vital sign check before giving, max dosage per 24 hours,etc.) Possible side effects Colace/docusate sodium 100mg capsule PO Qday Therapeutic: Laxative Pharmacologic: stool softner Assess for abdominal distention, bowel sounds, bowel function. Max dosage 50-400mg in 1-4 divided doses Lovenox/enoxaparin sodium 30mg SQ Q 12 hours Therapeutic: anticoagulant Pharmacologic: antithrombotic Assess for signs of bleeding, thrombosis. Max dosage 30mg q 12 hours Dizziness, headache, insomia, bleeding, anemia Lipitor/atorvastatin 40mg PO HS Therapeutic: lipid-lowering Pharmacologic: Reductase Inhibitor (statin) Evaluate serium cholesterol and triglyceride level,monitor liver function test, if muscle tenderness monitor CK level; avoid grapefruit juice, may be administered anytime of day; do not skip doses. Max dosage 80mg/day Dizziness, headache, insomian, weakness, abdominal cramps, constipation Actos/pioglitazone 15mg PO QD8 Therapeutic: antidiabetic Pharmacologic: thiazolidinediones Observe for s/s hypoglycemic reaction (sweating, hunger, weakness, dizziness, tachycardia). Max dosage 45mg/day Edema, hepatits, ↑ liver enzymes, anemai Amaryl/glimepiride 1mg PO QD8 Therapeutic: antidiabetic Pharmacologic: sulfonyureas Novolg (BS-100)/30 for >160 BS SQ Q6H Therapeutic: antidiabetic Pharmacologic: pancreatic Low weight Heparin/prevent DVT Decrease insulin resistance Stimulate release of insuline from pancrease and increase sensitivity of receptor sites Rapid acting, lower blood glucose by stimulating uptakein skeletal muscle and fat Revised 3/25/09 NURS 3313 K. Lishman Observe for s/s hypoglycemic reaction (sweating, hunger, weakness, dizziness, tachycardia). Assess for allergy to sulfaonamides, monitor CBC. Max dosage 8mg/day Observe for s/s hypoglycemia (sweating, hunger, weakness, dizziness, tachycardia) and hyperglycemia (confusion, drowsiness, flushed, dry skin, fruity breath, poluria, n/v) Max dosage depends on sliding scale. Throat irritation, mild cramps Dizziness, drowsiness, headache, photsensitivity, aplastic anemia Hypoglycemia, anaphylaxis, Onset 10-20 min, peak 1-3 hr, duration 3-5 hour Revised 3/25/09 NURS 3313 K. Lishman






