Neuroanatomy Ch 10 392-413 [4-20
advertisement

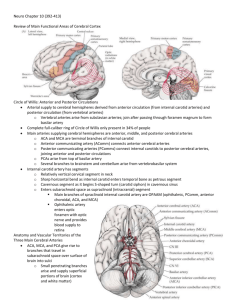
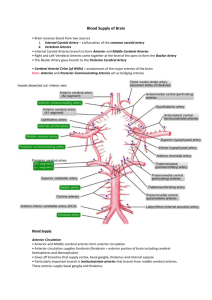
Neuroanatomy Ch 10 392-413 Cerebral Hemispheres and Vascular Supply Review of Main Functional Areas of Cerebral Cortex – face and hands of sensorimotor homunculi are on lateral convexities, while leg areas are in the interhemispheric fissure -in the dominant (usually left) hemisphere, Broca’s area is in the inferior frontal gyrus; Wernicke’s area is in the superior temporal gyrus, next to primary auditory cortex -Association cortex in the nondominant hemisphere (right) is important for attention to the contralateral body and space -primary visual hemifield lies along calcarine fissure of occipital lobe -optic radiations, white matter pathways carrying visual information from thalamus to visual cortex pass under parietal and temporal cortex Circle of Willis: Anterior and Posterior Circulations – supply to cerebral hemispheres derived from: 1. Anterior Circulation: internal carotid arteries arising from common carotid from aorta; at bifurcation of carotid, the common carotid splits into internal and external carotid 2. Posterior Circulation: vertebral arteries arise from subclavian arteries and ascends through foramina in the transverse processes of cervical vertebrae before entering foramen magnum and joining to form the basilar artery -anterior and posterior circulations meet at the circle of Willis, from which all major cerebral vessels arise, and provides major collateral flow -main arteries supplying cerebral hemispheres are anterior cerebral arteries (ACAs), middle cerebral arteries (MCAs), and posterior cerebral arteries -the ACAs and MCAs are terminal branches of the internal carotid arteries -the anterior cerebral arteries anastomose anteriorly at the anterior communicating artery (Acomm) -anterior and posterior circulations are linked to each other via posterior communicating arteries (PComms), which connect internal carotids to the posterior cerebral arteries, joining the anterior and posterior circulations -the posterior cerebral arteries (PCAs) arise from top of the basilar artery, formed by convergence of the two vertebral arteries -internal carotid artery has several named segments 1. Cervical Segment – is found in the neck 2. Petrous Segment – as cervical segment sharply bends and enters temporal bone 3. Cavernous Segment – as internal carotid begins an S-shaped turn, also known as carotid siphon within the cavernous sinus 4. Supraclinoid (intracranial Segment) – after cavernous segment, the artery passes anterior clinoid process to pierce the dura and bends posteriorly to enter subarachnoid space as this artery. There are several branches of this artery remembered by OPAAM -Ophthalmic, Posterior communicating, Anterior choroidal, Anterior Cerebral, Middle cerebral -ophthalmic artery branches just after internal carotid enters the dura Anatomy of Vascular Territories of the Three Main Cerebral Arteries – the three main arteries ACA, MCA, PCA give rise to many small branches that travel in subarachnoid space over brain and into sulci Vascular Territories of Superficial Cerebral Structures – 1. Anterior Cerebral Artery – passes in the interhemispheric fissure as it sweeps around the corpus callosum and branches into the pericallosal and callosomarginal arteries 2. Middle Cerebral Artery – turns laterally to enter depths of Sylvian fissure, where it bifurcates into the superior division and the inferior division a. Superior division supplies the cortex above Sylvian Fissure including lateral frontal lobe b. Inferior division supplies cortex below Sylvian Fissure including lateral temporal lobe and part of the parietal lobe 3. Posterior Cerebral Artery – curves back after arising from the top of the basilar and sends branches over the inferior and medial temporal lobes and over the medial occipital cortex a. Posterior cerebral artery territory includes inferior and medial temporal/occipital cortex Vascular Territories of the Deep Cerebral Structures – most important penetrating vessels at the base of the brain are the lenticulostriate arteries arising from the initial portions of the middle cerebral artery before it enters the Sylvian fissure -these arteries supply regions of basal ganglia and internal capsule Clinical Syndromes of Three Cerebral Arteries: Infarcts 1. Left MCA Superior Division – R face and arm weakness of upper motor neuron type and Broca’s aphasia 2. Left MCA Inferior Division – Wernicke’s aphasia and R visual field deficit, may seem crazy 3. Left MCA Deep Territory – R pure motor hemiparesis of upper motor neuron type 4. Left MCA stem – combination of above, w/ R hemiplegia, R hemianesthesia, R homonymous hemianopia, and global aphasia; Often a LEFT GAZE PREFERENCE 5. Right MCA Superior Division – L face and arm weakness, L hemineglect is present 6. Right MCA Inferior Division – profound L hemineglect, L visual field and somatosensory deficits present, motor neglect on the L side can also occur w/ mild L sided weakness 7. Right MCA Deep Territory – L pure motor hemiparesis of upper motor neuron type 8. Right MCA Stem – combination of above w/ L hemiplegia, L hemianesthesia, L homonymous hemianopia, and profound L hemineglect; usually RIGHT GAZE PREFERENCE 9. Left ACA – R leg weakness and R leg sensory loss; can cause R hemiplegia if large 10. Right ACA – L leg weakness and L leg sensory loss; can cause L hemiplegia if large 11. Left PCA – R homonymous hemianopia, can cause alexia without agraphia; may cause aphasia 12. Right PCA – L homonymous hemianopia, large infarct in thalamus may cause L hemisensory loss Watershed Infarcts – when cerebral artery is occluded, ischemia or infarction occurs in the territory supplied by the vessel, with other regions near vessels spared -when blood supply to two adjacent cerebral arteries is compromised, regions between the two vessels are most susceptible to ischemia and infarction -these regions between cerebral arteries are called watershed zones -bilateral watershed infarcts can occur in both ACA-MCA and MCA-PCA zones with severe drops in systemic blood pressure -a sudden occlusion of internal carotid or a drop in BP in pt w/ carotid stenosis can = ACA-MCA infarct -watershed infarcts can produce proximal arm/leg weakness because regions of homunculus involved include trunk and proximal limbs -in dominant hemisphere, watershed infarcts can cause transcortical aphasia syndromes -MCA-PCA infarcts can cause disturbances of higher-order visual processing -they can also occur between superficial and deep territories of MCA Transient Ischemic Attack (TIA) – typically last for 10 MINUTES, if more than an hour, they are usually small infarcts. 15% of patients with TIAs will have a stroke causing persistent deficits within 3 months, and half of them will occur within first 48 hours; they are warning signs of potentially larger ischemic injury to brain -can be caused by embolus occluding vessel that dissolves to allow blood to return, in-situ thrombus formation and/or vasospasm leading to narrowing of blood vessel lumen Transient Loss of Consciousness – MOST COMMON CAUSE is cardiogenic syncope including vasovagal transient episodes of hypotension, arrhythmias, and other non-neurological causes Ischemic Stroke – occurs when inadequate blood supply to a region of the brain lasts long enough to cause infarction -in an embolic infarct – piece of material (usually blood clot) is formed in one place and travels through bloodstream to lodge in and occlude a blood vessel supplying the brain (occur suddenly) -in a thrombotic infarct – blood clot is formed locally on the blood vessel wall, usually at the site of an underlying atherosclerotic plaque, causing the vessel to occlude (may have stuttering course) -Large vessel infarcts – involve major blood vessels on the surface of brain such as the MCA + branches, often caused by emboli, although thrombosis can occur in proximal vessels such as vertebral, basilar, and carotid arteries -Small vessel infarcts – involve small, penetrating vessels supplying deep structures, such as basal ganglia, thalamus, and internal capsules -small vessel infarcts are sometimes called lacunar infarcts because they resemble small lakes Source of Emboli – emboli are most commonly composed of thrombotic (blood clot) material -Cardioembolic infarcts occur in the heart, in conditions such as atrial fibrillation, MI and valvular disease -Artery-to-Artery emboli – arise from a stenosed segment of internal carotid artery, vertebral stenosis, or an ectatic dilated basilar artery -Dissection of carotid or vertebral arteries can cause thrombus formation -emboli can also include air emboli, septic emboli, fat/cholesterol emboli, disc emboli, and amniotic fluid emboli Lacunar Syndromes – Syndrome Pure Motor Hemiparesis Ataxic Hemiparesis Pure Sensory Stroke (thalamic lacune) Clinical Features Unilateral face, arm, and leg weakness with dysarthria Same as pure motor hemiparesis, but with ataxia on same side as weakness Sensory loss to all primary modalities in contralateral face and body Sensorimotor Stroke (thalamocapsular lacune) Combination of thalamic lacune and pure motor hemiparesis Basal Ganglia Lacune Usually asymptomatic, but may cause hemiballismus Locations of Infarct Posterior limb of internal capsule Ventral Pons Posterior limb of internal capsule Ventral Pons Ventral posterior lateral nucleus of thalamus (VPL) Posterior limb of internal capsule, and either VPL or thalamic somatosensory radiation Caudate, putamen, globus pallidus, or subthalamic nucleus Stroke Risk Factors – hypertension, diabetes, hypercholesterolemia, cigarette smoking, prior history of vascular disease or stroke -atrial fibrillation, mechanical valves or other valvular abnormalities, patent foramen ovale, and decreased ejection fraction -hypercoagulable states are also risk factors Treatment and Diagnostic Workup of Ischemic Stroke and TIA Acute Management – do a CT scan to quickly find an ischemic event; most often not seen in the first few hours of symptoms, but a hemorrhage will always be visible -if hemorrhage is ruled out by CT, patients can be treated with the thrombolytic agent tissue plasminogen activator (tPA) with a good outcome if given within 4.5 hours of stroke onset, earlier the better; tPA carries risk of intracranial hemorrhage -if patients are not eligible for tPA or in patients who have had TIA, aspirin can reduce risk of recurrent stroke Diagnostic Evaluation – begins with history/physical exam, including questions about stroke risk factors and continues with diagnostic tests -blood flow in major cranial and neck vessels should be assessed with ultrasound or magnetic resonance angiography or CT angiography; important in suspected internal carotid stenosis -possibility of cardioembolic source should be investigated with ECG to look for cardiac ischemia or arrhythmias, and an echocardiogram to look for structural abnormalities or thrombi -studies have shown that patients with atrial fibrillation are at risk of embolic stroke and the risk is reduced when treated with warfarin (Coumadin), an oral anticoagulant Medium-to-Long Term Management – common complications include hemorrhagic conversion, seizures, and delayed swelling. With large MCA infarcts, substantial edema and mass effect may develop -measures for lowering intracranial pressure include hemicraniectomy where a portion of skull is removed over region of swelling and is later replaced after danger has passed -Preventive measures are most important in reducing incidence of recurrent stroke -risk factors such as hypertension, smoking, and hypercholesterolemia should be addressed -medications such HMG-CoA reductase inhibitors (statins) should be addressed to reduce cholesterol levels -antiplatelet drugs like aspirin have been shown to reduce risk of ischemic stroke recurrence Carotid Stenosis – atherosclerotic disease most commonly leads to stenosis of internal carotid artery just beyond carotid bifurcation -thrombi formed on a stenotic internal can embolize to form TIAs, or infarcts of MCA, ACA, or ophthalmic artery -can be associated with MCA territory symptoms such as contralateral face-arm, or face-arm-leg weakness, contralateral sensory changes, contralateral visual field defects, aphasia, or neglect -ophthalmic artery symptoms such as ipsilateral monocular visual loss is known as amaurosis fugax and ACA territory symptoms such as contralateral leg weakness -carotid stenosis can be detected on physical exam as a whooshing sound (bruit) that continues into diastole and is best hear with the bell at engle of jaw -symptomatic carotid stenosis – when patients have carotid stenosis along with transient monocular blindness on same side or TIAs/strokes causing symptoms on contralateral side -mainstay treatment for symptomatic carotid stenosis is carotid endarterectomy where the carotid is exposed and clamped temporarily -incision is made and the atheromatous material is shelled out, eliminating the stenosis -in less severe carotid stenosis, angioplasty and stenting can be performed if patient is at high surgical risk for traditional carotid endarterectomy -if internal carotid becomes 100% occluded, it causes infarcts in the MCA, ACA, or watershed territories; may be completely asymptomatic if there is adequate collateral flow through anterior/posterior communicating arteries -occurs most often just beyond carotid bifurcation Dissection of the Carotid or Vertebral Arteries – a small tear can form in the intimal surface of carotid or vertebral arteries, allowing blood to burrow into vessel wall, producing a dissection; a flap protrudes into the vessel lumen where a thrombus can form and embolize distally -patients may describe feeling a pop at the onset -carotid dissection – may hear turbulent sound with each heartbeat and have ipsilateral horner’s syndrome and pain over the eye -vertebral dissection – most often posterior neck and occipital pain -TIAs or infarcts occur in anterior circulation with carotid dissection and in posterior circulation with vertebral dissection -diagnosis is with MRI/MRA, or CTA of the neck to show vessel irregularity, narrowing, and sometimes visualization of a false lumen in the vessel wall adjacent to the true lumen -primarily treated with intravenous heparin followed by warfarin anticoagulation Venous Drainage – superficial veins superior sagittal sinus cavernous sinus More specifically: Superior sagittal sinus transverse sinuses sigmoid sinus Cavernous sinus superior petrosal sinus transverse sinus and inferior petrosal sinus internal jugular vein -in the cavernous sinus, the internal carotid, and CN III, IV, V1, V2, and VI pass through Sagittal Sinus Thrombosis – often associated with a hypercoagulable state and occurs with increased frequency in pregnant women and within first few weeks post partum -obstruction of venous drainage can cause elevated intracranial pressure, which can cause parasagittal hemorrhages and/infarcts -patients often have headaches and papilledema and a decreased level of consciousness -Superior sagittal sinus can be seen as a triangular region on axial CT and MRI; -sinus normally fills with intravenous contrast, but in sagittal sinus thrombosis there may be central, darker-filled defect, called the empty delta sign -magnetic resonance venography (MRV) should be performed or a conventional angiogram -treatment for sagittal sinus thrombosis can be anticoagulation therapy -venous thrombosis can occur less commonly leading to infarcts or hemorrhage in territories of deep cerebral veins or a major cortical vein