Psychosocial History - Basin Counseling Inc.
advertisement

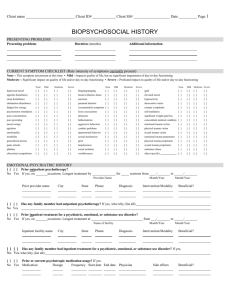
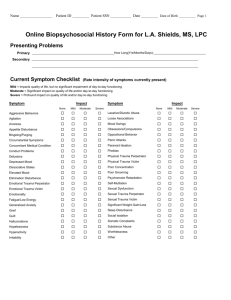
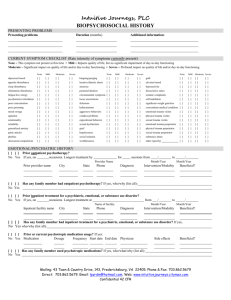
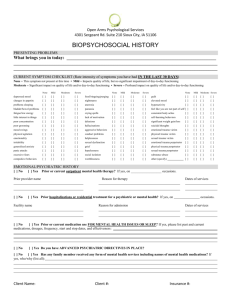
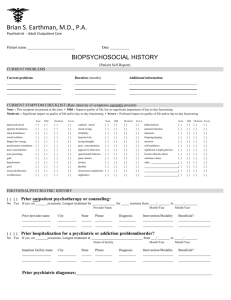
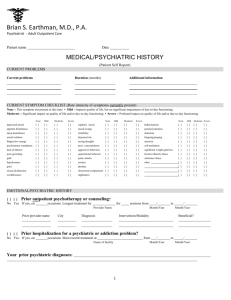
Client Name____________________________________________________ Date_______________________ Page __1__ PSYCHOSOCIAL HISTORY PRESENTING PROBLEMS:______________________________________________________________________________________ ____________________________________________________________________________________________________________ Duration:____________________________________________________________________________________________________ Additional information:_________________________________________________________________________________________ ____________________________________________________________________________________________________________ CURRENT SYMPTOM CHECKLIST: (Rate intensity of symptoms currently present) NONE = This symptom not present at this time MILD = Impacts quality of life, but no significant impairment of day-to-day functioning MODERATE = Significant impact on quality of life and/or day-to-day functioning SEVERE = Profound impact on quality of life and/or day-to-day functioning None Depressed mood ( ) Appetite disturbance ( ) Sleep disturbance ( ) Elimination disturbance ( ) Fatique/low energy ( ) Psychomotor retardation( ) Poor concentration ( ) Poor grooming ( ) Mood swings ( ) Agitation ( ) Emotionality ( ) Irritability ( ) Generalized anxiety ( ) Panic attacks ( ) Phobias ( ) Obsessions/compulsions( ) Mild ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) Moderate ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) Severe None ( ) binging/purging ( ) ( ) laxative/diuretic abuse ( ) ( ) anorexia ( ) ( ) paranoid ideation ( ) ( ) circumstance symptom ( ) ( ) loose associations ( ) ( ) delusions ( ) ( ) hallucinations ( ) ( ) aggressive behaviors ( ) ( ) conduct problems ( ) ( ) oppositional behavior ( ) ( ) sexual dysfunction ( ) ( ) grief ( ) ( ) hopelessness ( ) ( ) social isolation ( ) ( ) worthlessness ( ) Mild ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) Moderate ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) Severe ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) guilt elevated mood hyperactivity dissociative states somatic complaints self-mutilation weight gain/loss concomitant condition emotion trauma victim physical trauma victim sexual trauma victim emotional trauma perp physical trauma perpet sexual trauma perpetra substance abuse other (specify) None Mild Moderate ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) Severe ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) EMOTIONAL/PSYCHIATRIC HISTORY ( ) ( ) Counseling History No Yes If yes, on _____ occasions. Longest treatment by _______________________for ____ sessions from ____/____ to ____/____ Provider Name Mo Yr Mo Yr Prior provider name ________________ City ___________________ State __________________ Phone __________________ Diagnosis __________________ Intervention/Modality Beneficial? _____________________________ _____________________ ________________ __________ ________ __________________ ___________________ __________________ _____________________________ _____________________ ( ) ( ) Has any family member had counseling? If yes, who/why (list all):_______________________________________________________ No Yes ___________________________________________________________________________________________________________________________ ( ) ( ) Prior inpatient treatment for a psychiatric, emotional, or substance use disorder? No Yes If yes, on ______occasions. Longest treatment at _________________________ from ____/____ to ____/____ Name of Facility Inpatient facility name __________________ __________________ City State Phone Diagnosis _______ _______ _______ ______________ _______ _______ _______ ______________ Mo Yr Mo Intervention/Modality ______________________ ______________________ Yr Beneficial? ___________________ ___________________ ( ) ( ) Has any family member had inpatient treatment for a psychiatric, emotional, or substance use disorder? If yes, No Yes who/why (list all): ____________________________________________________________________________________________________________ ( ) ( ) Current Medications: If yes: No Yes Medication ____________ ____________ ____________ ____________ ____________ ____________ Dosage ______ ______ ______ ______ ______ ______ Frequency _____________ _____________ _____________ _____________ _____________ _____________ Start date _____________ _____________ _____________ _____________ _____________ _____________ Physician ____________________________ ____________________________ ____________________________ ____________________________ ____________________________ ____________________________ Client Name_____________________________________________________ Date_____________________ Page__2__ FAMILY HISTORY FAMILY OF ORIGIN Present during childhood: Present Present Not Entire part of present Childhood childhood at all Mother ( ) ( ) ( ) Father ( ) ( ) ( ) Stepmother ( ) ( ) ( ) Stepfather ( ) ( ) ( ) Brother(s) ( ) ( ) ( ) Sister(s) ( ) ( ) ( ) Other ( ) ( ) ( ) (specify) ____________________________________ Parents’ current marital status: ( ) married to each other ( ) separated for ____ years ( ) divorced for ____ years ( ) mother remarried ____ times ( ) father remarried ____ times ( ) mother involved with someone ( ) father involved with someone ( ) mother deceased for ____ years age of client at mother’s death ____ ( ) father deceased for ____ years age of client at father’s death ____ Describe parents: Father Full Name__________________ Occupation_________________ Education__________________ General Health______________ Mother _______________________ _______________________ _______________________ _______________________ Describe childhood family experience: ( ) outstanding home environment ( ) normal home environment ( ) chaotic home environment ( ) witnessed physical/verbal/sexual abuse toward others ( ) experienced physical/verbal/sexual abuse from others Special circumstances in childhood:______________________________________________________________________________________________________ ____________________________________________________________________________________________________________________________________ ____________________________________________________________________________________________________________________________________ IMMEDIATE FAMILY Marital status: ( ) single, never married ( ) engaged ____ months ( ) married for ____ years ( ) divorced for ____ years ( ) separated for ____ years ( ) divorce in process ____ months ( ) live-in for ____ years ( ) ____prior marriages (self) ( ) ____ prior marriages (partner) Intimate relationship: ( ) never been in a serious relationship ( ) not currently in relationship ( ) currently in a serious relationship Relationship satisfaction: ( ) very satisfied with relationship ( ) satisfied with relationship ( ) somewhat satisfied with relationship ( ) dissatisfied with relationship ( ) very dissatisfied with relationship List all persons currently living in client’s household: Name Age Sex Relationship to Client ________________ ___ ___ _________________ ________________ ___ ___ _________________ ________________ ___ ___ _________________ ________________ ___ ___ _________________ ________________ ___ ___ _________________ List children not living in same household as client: _________________ ___ ___ _________________ _________________ ___ ___ _________________ _________________ ___ ___ _________________ Describe any past or current significant issues in intimate relationships: __________________________________________________________________ ______________________________________________________________________________________________________________________________ ______________________________________________________________________________________________________________________________ ______________________________________________________________________________________________________________________________ Describe any past or current significant issues in other immediate family relationships: ______________________________________________________ _______________________________________________________________________________________________________________________________ _______________________________________________________________________________________________________________________________ _______________________________________________________________________________________________________________________________ MEDICAL HISTORY (check all that apply for client) Describe current physical health: ( ) Good ( ) Fair ( ) Poor ______________________________________________________ List any known allergies:_________________________________ Is there a history of any of the following in the family: ( ) tuberculosis ( ) heart disease ( ) birth defects ( ) high blood pressure ( ) emotional problems ( ) alcoholism ( ) behavior problems ( ) drug abuse ( ) thyroid problems ( ) diabetes ( ) cancer ( ) Alzheimer’s disease/dementia ( ) mental retardation ( ) stroke ( ) other chronic or serious health problems ____________ ______________________________________________ List any abnormal lab test results: Date __________ Result _____________________ Date__________ Result _____________________ Describe any serious hospitalization or accidents: Date ________ Age ____ Reason_____________________ Date_________ Age ____ Reason _____________________ List name of primary care physician: Name___________________________ Phone________________ List name of psychiatrist: (if any) Name___________________________ Phone________________ Client Name_________________________________________________________ Date _________________ Page __3__ SUBSTANCE USE HISTORY (check all that apply for patient) Family alcohol/drug abuse history: ( ( ( ( ( ) father ( ) stepparent/live-in ) mother ( ) uncle(s)/aunt(s) ) grandparent(s) ( ) spouse/significant other ) sibling(s) ( ) children ) other______________________ Substance use status: ( ( ( ( ( ( ) no history of abuse ) active abuse ) early full remission ) early partial remission ) sustained full remission ) sustained partial remission Substances used: (complete all that apply) ( ) alcohol ( ) amphetamines/speed ( ) barbiturates/owners ( ) caffeine ( ) cocaine ( ) crack cocaine ( ) hallucinogens (e.g. LSD) ( ) inhalants (e.g. glue, gas) ( ) marijuana or hashish ( ) nicotine/cigarettes ( ) PCP ( ) prescription__________ ( ) other_______________ First use age ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ Last use age ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ Treatment history: Consequences of substance abuse (check all that apply): ( ( ( ( ( ( ( ( ( ( ) outpatient (age(s)_________________ ) inpatient (age(s)__________________ ) 12-step program (age(s) ___________ ) stopped on own (age(s) ____________ ) other (age(s)_____________________ Describe:________________________ Current Use (Yes/No) _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ Frequency ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ Amount ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ) hangovers ( ) withdrawal symptoms ( ) sleep disturbance ( ) binges ) seizures ( ) medical conditions ( ) assaults ( ) job loss ) blackouts ( ) tolerance changes ( ) suicidal impulse ( ) arrests ) overdose ( ) loss of control amount used ( ) relationship conflicts ) other____________________________________________________________________________ DEVELOPMENTAL HISTORY (check all that apply for a child/adolescent client) Problems during Mother’s pregnancy: ( ) none ( ) high blood pressure ( ) kidney infection ( ) German measles ( ) emotional stress ( ) bleeding ( ) alcohol use ( ) drug use ( ) cigarette use ( ) other Birth: ( ) normal delivery ( ) difficult delivery ( ) cesarean delivery ( ) complications________________ Birth weight ____ Lbs. ____ oz. Infancy: ( ) feeding problems ( ) sleep problems ( ) toilet training problems Childhood health (enter age occurred) ( ) chickenpox _________ ( ) lead poisoning _____ ( ) German measles _____ ( ) mumps ___________ ( ) red measles _________ ( ) diphtheria _________ ( ) rheumatic fever ______ ( ) poliomyelitis________ ( ) whooping cough ______ ( ) pneumonia ________ ( ) scarlet fever_________ ( ) tuberculosis________ ( ) autism ( ) mental retardation ( ) ear infections ( ) asthma ( ) allergies to ____________________________________ ( ) chronic, serious health problems___________________ ______________________________________________ Delayed developmental milestones (check only milestones that did not occur at expected age): Emotional/behavior problems (check all that apply): ( ( ( ( ( ( ( ( ( ( ( ( ( ( ( ( ( ( ( ) sitting ( ) controlling bowels ) rolling over ( ) sleeping alone ) standing ( ) dressing self ) walking ( ) engaging peers ) feeding self ( ) tolerating separation ) speaking words ( ) playing cooperatively ) speaking sentences ( ) riding tricycle ) controlling bladder ( ) riding bicycle ) other_______________________________________ ) drug use ) alcohol abuse ) chronic lying ) stealing ) violent temper ) fire-setting ) animal cruelty ) hyperactive ) assaults others ) disobedient ( ( ( ( ( ( ( ( ( ( ) repeats words of others ) not trustworthy ) hostile/angry mood ) indecisive ) immature ) bizarre behavior ) frequently tearful ) self-injurious threats ) frequently daydreams ) lack of attachment Social Interaction (check all that apply): Intellectual/academic functioning (check all that apply): ( ( ( ( ( ) normal intelligence ( ) high intelligence ( ) learning problems ) normal social interaction ) isolates self ) very shy ) alienates self ( ( ( ( ) inappropriate sex play ) dominates others ) associates with acting-out ) other ________________ ( ) authority conflicts ( ) attention problems ( ) underachieving ( ( ( ( ( ( ( ( ( ) distrustful ) extreme worrier ) self-injurious acts ) impulsive ) easily distracted ) poor concentration ) often sad ) breaks things ) other______________ __________________ ( ) mild retardation ( ) moderate retardation ( ) severe retardation Current or highest education level _______________________________________________ Describe any other developmental problems or issues: ____________________________________________________________________________________ __________________________________________________________________________________________________________________________________ __________________________________________________________________________________________________________________________________ Client Name_________________________________________________________Date____________________ Page__4__ SOCIO-ECONOMIC HISTORY (check all that apply for client) Living situation: Social support system: ( ( ( ( ) housing adequate ( ) supportive network ) homeless ( ) few friends ) housing overcrowded ( ) substance-use-based friends ) dependent on others ( ) no friends for housing ( ) distant from family of origin ( ) housing dangerous/deteriorating ( ) living companions dysfunctional Employment: Military history: ( ( ( ( ( ( ( ( ) never in military ( ) served in military – no incident ( ) served in military – with incident __________________________ __________________________ __________________________ ) employed and satisfied ) employed but dissatisfied ) unemployed ) coworker conflicts ) supervisor conflicts ) unstable work history ) disabled:______________ Sexual history: ( ( ( ( ( ) heterosexual orientation ) homosexual orientation ) bisexual orientation ) currently sexually active ) currently sexually satisfied Financial situation: ( ( ( ( ( ) currently sexually dissatisfied ) age first sex experience _____ ) age first pregnancy/fatherhood _____ ) history of promiscuity age ____to ____ ) history of unsafe sex age ____to ____ ( ( ( ( ( ) no current financial problems ) large indebtedness ) poverty or below-poverty income ) impulsive spending ) relationship conflicts over finances Additional information:__________________________________________________ _____________________________________________________________________ _____________________________________________________________________ Legal history: ( ( ( ( ( ( Cultural/spiritual/recreational history: ) no legal problems Cultural identity (i.e. ethnicity, religion):_____________________________________________________ ) now on parole/probation ______________________________________________________________________________________ ) arrest(s) not substance-related Describe any cultural issues that contribute to current problem:__________________________________ ) arrest(s) substance-related ______________________________________________________________________________________ ) court ordered this treatment ______________________________________________________________________________________ ) jail/prison ______ time(s) Total time served:___________ Describe last legal difficulty:____________________________________________________________________________________________ ___________________________________________________________________________________________________________________ SOURCES OF DATA PROVIDED ABOVE: ( ) Client self-report for all. ( ) A variety of sources (if so, check appropriate sources below): Presenting Problems/Symptoms Family History Developmental History ( ) client self-report ( ) client’s parent/guardian ( ) other (specify)__________________ ( ) client self-report ( ) client’s parent/guardian ( ) other (specify)_______________ ( ) client self-report ( ) client’s parent/guardian ( ) other (specify)_______________ Emotional/Psychiatric History Medical/Substance Use History Socioeconomic History ( ) client self-report ( ) client’s parent/guardian ( ) other (specify)__________________ ( ) client self-report ( ) client self-report ( ) client’s parent/guardian ( ) client’s parent/guardian ( ) other (specify)_______________ ( ) other (specify)______________