Click here to
advertisement
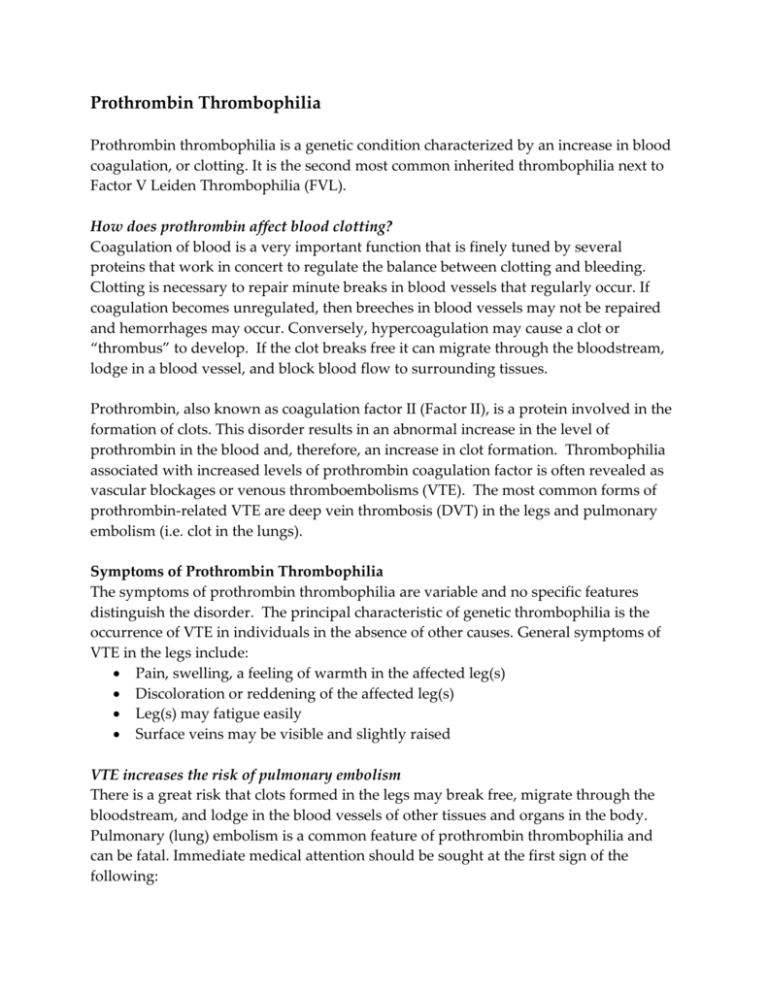
Prothrombin Thrombophilia Prothrombin thrombophilia is a genetic condition characterized by an increase in blood coagulation, or clotting. It is the second most common inherited thrombophilia next to Factor V Leiden Thrombophilia (FVL). How does prothrombin affect blood clotting? Coagulation of blood is a very important function that is finely tuned by several proteins that work in concert to regulate the balance between clotting and bleeding. Clotting is necessary to repair minute breaks in blood vessels that regularly occur. If coagulation becomes unregulated, then breeches in blood vessels may not be repaired and hemorrhages may occur. Conversely, hypercoagulation may cause a clot or “thrombus” to develop. If the clot breaks free it can migrate through the bloodstream, lodge in a blood vessel, and block blood flow to surrounding tissues. Prothrombin, also known as coagulation factor II (Factor II), is a protein involved in the formation of clots. This disorder results in an abnormal increase in the level of prothrombin in the blood and, therefore, an increase in clot formation. Thrombophilia associated with increased levels of prothrombin coagulation factor is often revealed as vascular blockages or venous thromboembolisms (VTE). The most common forms of prothrombin-related VTE are deep vein thrombosis (DVT) in the legs and pulmonary embolism (i.e. clot in the lungs). Symptoms of Prothrombin Thrombophilia The symptoms of prothrombin thrombophilia are variable and no specific features distinguish the disorder. The principal characteristic of genetic thrombophilia is the occurrence of VTE in individuals in the absence of other causes. General symptoms of VTE in the legs include: Pain, swelling, a feeling of warmth in the affected leg(s) Discoloration or reddening of the affected leg(s) Leg(s) may fatigue easily Surface veins may be visible and slightly raised VTE increases the risk of pulmonary embolism There is a great risk that clots formed in the legs may break free, migrate through the bloodstream, and lodge in the blood vessels of other tissues and organs in the body. Pulmonary (lung) embolism is a common feature of prothrombin thrombophilia and can be fatal. Immediate medical attention should be sought at the first sign of the following: Sudden dizziness or lightheaded feeling Coughing, often with the appearance of blood Shortness of breath; rapid breathing What are some of the warning signs of prothrombin thrombophilia? Prothrombin thrombophilia can be suspected if any of the following the VTE events have occurred: A first VTE before age 50 A first unprovoked VTE at any age A history of recurrent VTE Venous thrombosis at unusual sites (e.g. brain, mesentery, veins in the liver) VTE during pregnancy or the puerperium VTE associated with the use of oral contraceptives or hormone replacement therapy A first VTE in an individual with a first-degree family member with VTE before age 50 Women with unexplained fetal loss after 10 weeks’ gestation [ACOG guidelines; Practice Bulletin Number 113] Genetics of Prothrombin Thrombosis The instructions for the synthesis of the prothrombin protein, are encoded by the F2 gene (OMIM 176930). Prothrombin is also known as coagulation factor II or Factor II. An individual with prothrombin thrombophilia has a defective (mutated) copy of the F2 gene. The most common mutation in F2, named G20210A causes cells to produce elevated levels of prothrombin protein. How is prothrombin thrombophilia inherited? Each person has two copies of the F2 gene, one copy acquired from each parent. An individual with two normal copies (referred to as homozygous – same alleles) does not have a genetic predisposition for prothrombin thrombophilia. The G20210A mutation is said to be dominant. That is, an individual needs to possess only one defective copy of F2 G20210A along with a normal copy of F2 to exhibit symptoms of prothrombin thrombophilia. Such an individual is said to be heterozygous for the mutation (different alleles for the gene). An individual may also have two copies of the F2 G20210A mutation (i.e. homozygous for the mutation). The G20210A mutation causes higher levels of prothrombin in the blood, and, thus, more clots to form. The incidence of prothrombin thrombophilia varies among races. The disorder is prevalent in 2-5% of Caucasians, 0-0.3% of African Americans, and is extremely rare in Asian, African and Native American populations. What are some of the risks associated with prothrombin thrombophilia? The clinical features of prothrombin thrombophilia can vary widely. Some heterozygous individuals (normal F2/G20210A) may have recurrent VTE before age 30, while others may be asymptomatic until adulthood. Still, many individuals with the common G20210A mutation do not develop thrombosis at all. In addition, patients who are homozygous for the G20210A (G20210A/G20210A) mutation generally have greater risk of thrombosis than heterozgotes. In general, individuals with G20210A have a greater risk of thrombotic events and complications than those with a normal F2 gene (Table 1). Table 1 Risks and Complications Associated with Prothrombin Thrombosis Deep Vein Thrombosis Superficial Venous Thrombosis Adults heterozygous for G20210A allele have a 2-4 fold increased risk for DVT. Children have a 3-4 fold increased risk G20210A heterozygotes have a 4 fold increased risk Thrombosis in Unusual Locations Cerebral vein thrombosis- 6-10 fold increased in G20210A heterozygotes Hepatic, portal and retinal vein thrombosis Pregnancy Complications Pregnancy loss Placental abruption Preeclampsia Fetal growth retardation Various factors may predispose G20210A-positive individuals to thrombosis. These include both genetic and other causes (Table 2). Table 2 Factors That Predispose G20210A Individuals to Thrombosis Number of G20210A Alleles Heterozygotes have a 2-4 fold risk of VTE Homozygotes have a higher risk than heterozygotes Coexisting Genetic Abnormalities Mutations in Clotting Factor V Leiden (FVL)FVL - double heterozygotes (G20210A/G20210A/FVL/FVL) have a 20-60fold increased risk of VTE Circumstantial Risk Factors Pregnancy: 3-115-fold increased risk of VTE Oral Contraceptives: 16-59-fold increased risk of VTE Selective estrogen receptor modifiers (SERMs): Organ transplantation Central venous catheters: 2-3-fold risk of VTE Travel: 17-fold risk of VTE [Kujovitch, 2011] Genetic Testing for Prothrombin Thrombophilia A physician who suspects that a patient may have prothrombin thrombophilia, based on clinical symptoms, may order a genetic test to be performed. The patient’s blood sample is obtained and the DNA is them isolated from the blood. The DNA is then analyzed for the presence of the G20210A mutation. Diagnosis of prothrombin thrombophilia is based the presence of one or two copies (i.e. alleles) of the G20210A mutation. References Kujovitch JL. 2011. GeneReviews: Prothrombin-Related Thrombophilia (Last Update: March 29, 2011) American College of Obstetricians and Gynecologists (ACOG). Practice Bulletin Number 113. Inherited thrombophilias in pregnancy. 2010. Available online (registration or institutional access required). American College of Medical Genetics (ACMG). Technical standards and guidelines: Venous thromboembolism (Factor V Leiden and prothrombin 20210G>A testing): A disease-specific supplement to the standards and guidelines for clinical genetics laboratories. 2005. Available online. Additional Resources PubMed: Prothrombin thrombophilia Current literature National Blot Clot Alliance (http://stoptheclot.org/index.htm#.UbYfDOXD_IU) Resources for patients and families National Library of Medicine Genetics Home Reference: Prothrombin Thrombophilia Varga EA and Moll S. 2004. Prothrombin 20210 Mutation (Factor II Mutation). Circulation 110: e15-e18. Available online.