Common queries
advertisement

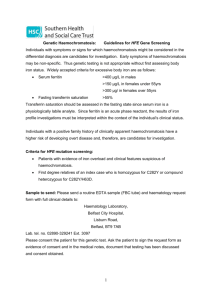
Common Queries (and hopefully some answers) Simon Watt Consultant Haematologist UHSM Haematology.Consultant@UHSM.NHS.UK B12 deficiency • • • • • • What is normal? Large intrapatient variation Investigations: Consider malabsorption eg. Coeliac Intrinsic factor Antibodies Schillings test not available Treatment • B12 injections if less than 100 or definite signs or symptoms • Consider oral if greater than 100 and asymptomatic and repeat in 3-6 months High ferritin • Acute phase marker • Also increased by liver disease • Suspect haemochromatosis when above absent • Check iron levels • TIBC saturation will be raised in haemochromatosis Hereditary Haemochromatosis Genetics and prevalence Odds ratio of developing clinical iron overload by genotype Prevalence of genotype amongst patients with clinical iron overload because of hereditary haemochromatosis (%) C282Y/C282Y 2300 60-90 C282Y/H63D 49 0-10 C282/WT 3.1 Rare H63D/H63D 6.3 0-4 H63D/WT 1.6 Rare WT/WT 1 15-30 Frequency of C282Y mutation in the population Thrombophila • Who to test? • Nobody? Thrombophilia screening Factor V Leiden (V resistant to cleavage by Protein C) Prothrombin gene G20210A variant (high II) Protein C Protein S Low Antithrombin Thrombophilia screening Antiphospholipid antibodies Anticardiolipin antibodies Lupus anticoagulant Anti-Beta2 glycoprotein I antibodies High homocysteine Thrombophilia? Recurrence Testing of relatives • Should only ever test 1st degree relatives • May make a difference to management eg OCP or pregnancy (rarely for men) • Only really useful if the affected relative has a known thrombophilia • May provide false reassurance if unknown/undetectable thrombophilia in family Neutropenia • • • • Common Rarely a serious cause found Multiple causes Note ethnic group Referral? • • • • If neutrophils less than 1 Progressive Associated with other FBC abnormalities Recurrent infection requiring antibiotics Some common causes • • • • • • • Auto-immune Myelodysplasia Liver disease/alcohol Portal hypertension Drugs B12/folate deficiency Infection and antibiotics Paraproteins • More common than you think • Probably 10-15% of over 80s • 3% of over 50s What could it be? • • • • • • MGUS-most common Approximately 1% per year progress to Asymptomatic myeloma Active myeloma Plasmacytoma Waldenstroms- IgM Assessment • • • • • Level and type of paraprotein IgA higher risk IgG less than 15g/l lower risk Normal SFLC lower risk IgM associated with Waldenstroms and not myeloma Assessment-doesn’t need HSC if • • • • FBC- normal or unchanged Calcium-normal No new pains eg back pain Renal function normal or stable Major Symptoms at MM Diagnosis Bone pain: 58% Fatigue: 32% Weight loss: 24% Paresthesias: 5% 11% are asymptomatic or have only mild symptoms at diagnosis Kyle RA, et al. Mayo Clin Proc. 2003;78:21-33.